Healthc Inform Res.
2022 Jan;28(1):3-15. 10.4258/hir.2022.28.1.3.
Review of Smart Hospital Services in Real Healthcare Environments
- Affiliations
-
- 1Department of Family Medicine, Seoul National University Hospital, Seoul, Korea
- 2Transdisciplinary Department of Medicine and Advanced Technology, Seoul National University Hospital, Seoul, Korea
- 3Department of Nuclear Medicine, Seoul National University Bundang Hospital, Seongnam, Korea
- 4Department of Emergency Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 5Department of Digital Health, Samsung Advanced Institute for Health Science & Technology (SAIHST), Sungkyunkwan University, Seoul, Korea
- 6Institute of Medical & Biological Engineering, Medical Research Center, Seoul National University College of Medicine, Seoul, Korea
- 7Department of Biomedical Engineering, Seoul National University College of Medicine, Seoul, Korea
- 8Biomedical Research Institute, Seoul National University Hospital, Seoul, Korea
- 9Department of Medicine, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2526489
- DOI: http://doi.org/10.4258/hir.2022.28.1.3
Abstract
Objectives
Smart hospitals involve the application of recent information and communications technology (ICT) innovations to medical services; however, the concept of a smart hospital has not been rigorously defined. In this study, we aimed to derive the definition and service types of smart hospitals and investigate cases of each type.
Methods
A literature review was conducted regarding the background and technical characteristics of smart hospitals. On this basis, we conducted a focus group interview with experts in hospital information systems, and ultimately derived eight smart hospital service types.
Results
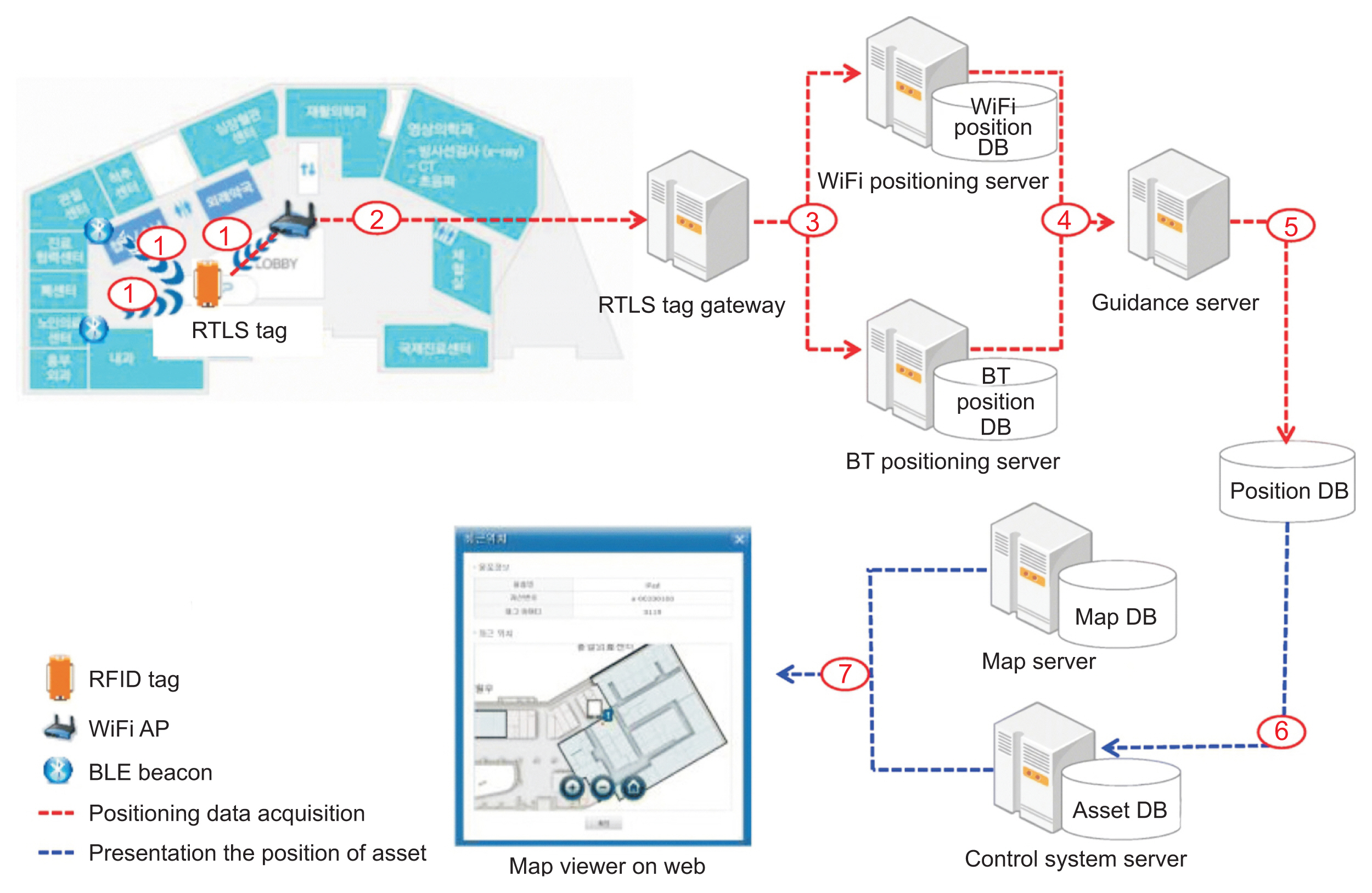
Smart hospital services can be classified into the following types: services based on location recognition and tracking technology that measures and monitors the location information of an object based on short-range communication technology; high-speed communication network-based services based on new wireless communication technology; Internet of Things-based services that connect objects embedded with sensors and communication functions to the internet; mobile health services such as mobile phones, tablets, and wearables; artificial intelligence-based services for the diagnosis and prediction of diseases; robot services provided on behalf of humans in various medical fields; extended reality services that apply hyper-realistic immersive technology to medical practice; and telehealth using ICT.
Conclusions
Smart hospitals can influence health and medical policies and create new medical value by defining and quantitatively measuring detailed indicators based on data collected from existing hospitals. Simultaneously, appropriate government incentives, consolidated interdisciplinary research, and active participation by industry are required to foster and facilitate smart hospitals.
Keyword
Figure
Reference
-
References
1. Korea Health Industry Statistics. Analysis of the background and characteristics of smart hospitals. Global Health Ind Trends. 2019; 325:1–4.2. Seoul Asan Hospital Innovation Design Center. We make human-centered hospitals. Seoul, Korea: Cloud-Nine Publisher;2020.3. Korea Digital Hospital Export Agency. Overview of digital hospitals [Internet]. Seoul, Korea: Korea Digital Hospital Export Agency;c2012. [cited at 2022 Feb 3]. Available from: http://kor.kohea.co.kr/hospital_over-view/ .4. Cho NW. Sung Sang-cheol, President of Seoul National University Bundang Hospital, which is about to open next June [Internet]. Seoul, Korea: Financial News;2002. [cited at 2022 Feb 3]. Available from: http://news.naver.com/main/read.nhn?mode=LPOD&mid=etc&oid=014&aid=0000026478 .5. Indeed Editorial Team. SMART goals: definition and examples [Internet]. Austin (TX): Indeed;c2022. [cited at 2022 Feb 3]. Available from: https://www.indeed.com/career-advice/career-development/smart-goals .6. Wikipedia. SMART [Internet]. [place unknown]: Wikipedia;2022. [cited at 2022 Feb 3]. Available from: https://en.wikipedia.org/wiki/SMART_criteria .7. Frisch P. What is an intelligent hospital?: a place where technology and design converge to enhance patient care. IEEE Pulse. 2014; 5(6):10–5.
Article8. Intelligent Health Association. Welcome to your association [Internet]. Media (PA): Intelligent Health Association;2020. [cited at 2022 Feb 3]. Available from: http://ihassociation.org .9. Frost & Sullivan. Smart hospitals to invest over €9.61 billion in cloud computing and data analytics, says Frost & Sullivan [Internet]. San Antonio (TX): Frost & Sullivan;2017. [cited at 2022 Feb 3]. Available from: https://www.frost.com/news/press-releases/smart-hospitals-invest-over-11-billion-cloud-computing-and-dataanalytics-says-frost-sullivan/ .10. Taylor K. Smart hospitals: how technology is redefining future healthcare [Internet]. London, UK: Deloitte UK Centre for Health Solutions;2017. [cited at 2022 Feb 3]. Available from: https://blogs.deloitte.co.uk/health/2017/06/smart-hospitals-how-technology-isredefining-future-healthcare.html .11. European Union Agency for Network and Information Security. Smart hospitals: security and resilience for smart health service and infrastructures [Internet]. Heraklion, Greece: European Union Agency for Network and Information Security;2016. [cited at 2022 Feb 3]. Available from: https://www.enisa.europa.eu/publications/cyber-security-and-resilience-for-smart-hospitals/at_download/fullReport .12. Yoon YD. Smart hospital-related technology status and prospects. KESSIA Issue Rep. 2018; (2):1–9.13. Ministry of Culture, Sports and Tourism. The smart hospital, opening a foundation for medical service innovation in the era of the 4th industrial revolution [Internet]. Sejong, Korea: Ministry of Culture, Sports and Tourism;2020. [cited at 2022 Feb 3]. Available from: https://www.korea.kr/news/pressReleaseView.do?newsId=156408065 .14. INNOPOLIS Foundation. Real-time location tracking systems market [Internet]. Daejeon, Korea: INNOPOLIS Foundation;2018. [cited at 2020 Feb 3]. Available from: https://www.innopolis.or.kr/board/view?linkId=44007&menuId=MENU00999 .15. Yoo S, Kim S, Kim E, Jung E, Lee KH, Hwang H. Real-time location system-based asset tracking in the healthcare field: lessons learned from a feasibility study. BMC Med Inform Decis Mak. 2018; 18(1):80.
Article16. Yamashita K, Oyama S, Otani T, Yamashita S, Furukawa T, Kobayashi D, et al. Smart hospital infrastructure: geomagnetic in-hospital medical worker tracking. J Am Med Inform Assoc. 2021; 28(3):477–86.
Article17. Zebra. University Health System: Passive smart pump management is more productive, reliable and cost-effective [Internet]. Lincolnshire (IL): Zebra Technologies Corporation;[cited at 2022 Feb 3]. Available from: https://hpaust.com/wp-content/uploads/2020/09/Success-Story-University-Health-System.pdf .18. Islam A. Benefits of Wi-Fi 6 for healthcare providers [Internet]. Crawley, UK: Spirent Communications;2020. [cited at 2022 Feb 3]. Available from: https://www.spi-rent.kr/blogs/benefits-of-wi-fi-6-for-healthcare-providers .19. White J. Wi-Fi 6 and healthcare [Internet]. Austin (TX): Wi-Fi Alliance;2019. [cited at 2022 Feb 3]. Available from: http://www.wi-fi.org/beacon/jay-white/wi-fi-6-and-healthcare .20. Chen M, Yang J, Zhou J, Hao Y, Zhang J, Youn CH. 5G-smart diabetes: toward personalized diabetes diagnosis with healthcare big data clouds. IEEE Commun Mag. 2018; 56(4):16–23.
Article21. Kumar A, Bhargav A, Karthikeyan A, Rajagopal K, Srinivasan AK, Tsegay AN. Low computational artificial intelligence genetic algorithm assisted SLM PAPR reduction technique for upcoming 5G based smart hospital. Malik H, Iqbal A, Joshi P, Agrawal S, Bakhsh FI, editors. Metaheuristic and evolutionary computation: algorithms and applications. Singapore: Springer;2021. p. 555–67.
Article22. Oracle. What is IoT? [Internet]. Austin (TX): Oracle;c2022. [cited at 2022 Feb 3]. Available from: https://www.oracle.com/internet-of-things/what-is-iot/ .23. Wikipedia. Internet of Things [Internet]. [place unknown]: Wikipedia;c2021. [cited at 2022 Feb 3]. Available from: https://ko.wikipedia.org/wiki/%EC%82%AC%EB%AC%BC%EC%9D%B8%ED%84%B0%EB%84%B7 .24. Uslu BC, Okay E, Dursun E. Analysis of factors affecting IoT-based smart hospital design. J Cloud Comput (Heidelb). 2020; 9(1):67.
Article25. Korea Health Industry Development Institute. A study on smart hospital developing plans for medical service innovation in the digital era. Osong, Korea: Korea Health Industry Development Institute;2020.26. Darshan KR, Anandakumar KR. A comprehensive review on usage of Internet of Things (IoT) in healthcare system. In : Proceedings of 2015 International Conference on Emerging Research in Electronics, Computer Science and Technology (ICERECT); 2015 Dec 17–19; Mandya, India.
Article27. Omar O. Intelligent building, definitions, factors and evaluation criteria of selection. Alex Eng J. 2018; 57(4):2903–10.
Article28. Wu B, Liu Z, George R, Shujaee KA. eWellness: building a smart hospital by leveraging RFID networks. In : Proceedings of the 27th Annual International Conference of the IEEE Engineering in Medicine and Biology Society; 20156 Jan 17–18; Shanghai, China.
Article29. Guinard PF. Building a smart hospital using RFID technologies. In : Proceedings of European Conference on eHealth; 2006 Oct 12–13; Fribourg, Switzerland.30. Park JH, Seol JA, Oh YH. Design and implementation of an effective mobile healthcare system using mobile and RFID technology. In : Proceedings of 7th International Workshop on Enterprise Networking and Computing in Healthcare Industry; 2005 Jun 23–25; Busan, Korea.
Article31. Jung KY, Kim T, Jung J, Lee J, Choi JS, Mira K, et al. The effectiveness of near-field communication integrated with a mobile electronic medical record system: emergency department simulation study. JMIR Mhealth Uhealth. 2018; 6(9):e11187.
Article32. Essink HM, Knops A, Liqui Lung AM, van der Meulen CN, Wouters NL, van der Molen AJ, et al. Real-time person identification in a hospital setting: a systematic review. Sensors (Basel). 2020; 20(14):3937.
Article33. Pickham D, Berte N, Pihulic M, Valdez A, Mayer B, Desai M. Effect of a wearable patient sensor on care delivery for preventing pressure injuries in acutely ill adults: a pragmatic randomized clinical trial (LS-HAPI study). Int J Nurs Stud. 2018; 80:12–9.
Article34. Abdulkareem KH, Mohammed MA, Salim A, Arif M, Geman O, Gupta D, et al. Realizing an effective COVID-19 diagnosis system based on machine learning and IOT in smart hospital environment. IEEE IoTJ. 2021; 8(21):15919–28.
Article35. Burrington-Brown J, Fishel J, Fox L, Friedman B, Giannangelo K, Jacobs E, et al. Defining the personal health record: AHIMA releases definition, attributes of consumer health record. J AHIMA. 2005; 76(6):24–5.36. Lee K. Personal health record (PHR) [Internet]. Newton (MA): SearchHealthIT;2017. [cited at 2022 Feb 3]. Available from: https://searchhealthit.techtarget.com/definition/personal-health-record-PHR .37. Kim SM, Kim T, Cha WC, Lee JH, Kwon IH, Choi Y, et al. User experience of mobile personal health records for the emergency department: mixed methods study. JMIR Mhealth Uhealth. 2020; 8(12):e24326.
Article38. Dameff C, Clay B, Longhurst CA. Personal health records: more promising in the smartphone era? JAMA. 2019; 321(4):339–40.39. Niazkhani Z, Toni E, Cheshmekaboodi M, Georgiou A, Pirnejad H. Barriers to patient, provider, and caregiver adoption and use of electronic personal health records in chronic care: a systematic review. BMC Med Inform Decis Mak. 2020; 20(1):153.
Article40. Lee JH. Smartwatch detects “COVID-19 early detected 7 days before symptoms” [Internet]. Seoul, Korea: GDnet Korea;2021. [cited at 2022 Feb 3]. Available from: https://zdnet.co.kr/view/?no=20210119105410 .41. NHS. About the NHS App [Internet]. Bethesda (MD): NHS;2021. [cited at 2022 Feb 3]. Available from: https://www.nhs.uk/nhs-services/online-services/nhs-app/about-the-nhs-app .42. Kim S, Ku S, Kim T, Cha WC, Jung KY. Effective use of mobile electronic medical records by medical interns in real clinical settings: mixed methods study. JMIR Mhealth Uhealth. 2020; 8(12):e23622.
Article43. IssueQuest. Development status and market prospects for medical and healthcare artificial intelligence (AI) and service robot technology. Seoul, Korea: IssueQuest;2020.44. Korea Intellectual Property Strategy Agency Future Technology Team. Patent megatrend analysis report (biology). Seoul, Korea: Korea Intellectual Property Strategy Agency;2019.45. Johns Hopkins Medicine. The Johns Hopkins Hospital launches capacity command center to enhance hospital operations [Internet]. Baltimore (MD): The Johns Hopkins Medicine;2016. [cited at 2022 Feb 3]. Available from: http://www.hopkinsmedicine.org/news/media/releases/the_johns_hopkins_hospital_launches_capacity_command_center_to_enhance_hospital_operations .46. VUNO. Our history [Internet]. Seoul, Korea: VUNO Inc.;c2021. [cited at 2022 Feb 3]. Available from: https://www.vuno.co/ .47. Gurak R. Can smart speakers improve the patient experience at hospitals? [Internet]. [place unknown]: The Dice Group;2020. [cited at 2022 Feb 3]. Available from: http://medium.com/dice-group/can-smart-speakers-improve-the-patient-experience-at-hospitals-69241a849937 .48. Cedars-Sinai. Cedars-Sinai Taps Alexa for smart hospital room pilot [Internet]. Los Angeles (CA): Cedars-Sinai;2019. [cited at 2022 Feb 3]. Available from: http://www.cedars-sinai.org/newsroom/cedars-sinai-taps-alexa-for-smart-hospital-room-pilot .49. Martinez DA, Kane EM, Jalalpour M, Scheulen J, Rupani H, Toteja R, et al. An electronic dashboard to monitor patient flow at the Johns Hopkins Hospital: communication of key performance indicators using the Donabedian model. J Med Syst. 2018; 42(8):133.
Article50. Kasten JE. Big data applications in healthcare administration. Int J Big Data Anal Healthc. 2020; 5(2):12–37.
Article51. Jang SM, Lee K, Hong YJ, Kim J, Kim S. Economic evaluation of robot-based telemedicine consultation services. Telemed J E Health. 2020; 26(9):1134–40.
Article52. Lee HS, Kim J. Scenario-based assessment of user needs for point-of-care robots. Healthc Inform Res. 2018; 24(1):12–21.
Article53. Petersen S, Houston S, Qin H, Tague C, Studley J. The utilization of robotic pets in dementia care. J Alzheimers Dis. 2017; 55(2):569–74.
Article54. Logan DE, Breazeal C, Goodwin MS, Jeong S, O’Connell B, Smith-Freedman D, et al. Social robots for hospitalized children. Pediatrics. 2019; 144(1):e20181511.
Article55. Siao CY, Chien TH, Chang RG. Robot scheduling for assistance and guidance in hospitals. Appl Sci. 2022; 12(1):337.
Article56. Holland J, Kingston L, McCarthy C, Armstrong E, O’Dwyer P, Merz F, et al. Service robots in the healthcare sector. Robotics. 2021; 10(1):47.
Article57. Kim SB. Health industry 4th industrial revolution series: medical augmented reality (AR)/virtual reality (VR) market trend analysis. KHIDI Brief. 2017; 251:1–15.58. Aziz HA. Virtual reality programs applications in healthcare. J Health Med Inform. 2018; 9(1):305.
Article59. Schmidt MW, Koppinger KF, Fan C, Kowalewski KF, Schmidt LP, Vey J, et al. Virtual reality simulation in robot-assisted surgery: meta-analysis of skill transfer and predictability of skill. BJS Open. 2021; 5(2):zraa066.
Article60. Pratt P, Ives M, Lawton G, Simmons J, Radev N, Spyropoulou L, et al. Through the HoloLens™ looking glass: augmented reality for extremity reconstruction surgery using 3D vascular models with perforating vessels. Eur Radiol Exp. 2018; 2(1):2.
Article61. The Medical Futurist. Augmented reality in healthcare: 9 examples [Internet]. Budapest, Hungary: The Medical Futurist;2021. [cited at 2022 Feb 3]. Available from: http://medicalfuturist.com/augmented-reality-in-healthcare-will-be-revolutionary/ .62. Treskunov A. Virtual Iraq for post traumatic stress disorder treatment [Internet]. [place: publisher unknown]. 2010. [cited at 2022 Feb 3]. Available from: http://anton.treskunov.net/projects/ptsd .63. Mozgai S, Hartholt A, Rizzo A. Iterative participatory design for VRET domain transfer: from combat exposure to military sexual trauma. In : Proceedings of Extended Abstracts of the 2020 CHI Conference on Human Factors in Computing Systems; 2020 Apr 25–30; Honolulu, HI.
Article64. Choi SR. Shionogi’s ADHD treatment app received approval from the US FDA [Internet]. Seoul, Korea: Yakup.com;2020. [cited at 2022 Feb 3]. Available from: http://m.yakup.com/?m=n&mode=view&nid=245990 .65. Yoo JH. Games, apps, and VR instead of drugs… The world of ‘digital therapy’ opens up [Internet]. Seoul, Korea: chosun.com;2020. [cited at 2022 Feb 3]. Available from: http://www.chosun.com/site/data/html_dir/2020/06/21/2020062102171.html .66. Wosik J, Fudim M, Cameron B, Gellad ZF, Cho A, Phinney D, et al. Telehealth transformation: COVID-19 and the rise of virtual care. J Am Med Inform Assoc. 2020; 27(6):957–62.
Article67. Kumar S, Merchant S, Reynolds R. Tele-ICU: efficacy and cost-effectiveness approach of remotely managing the critical care. Open Med Inform J. 2013; 7:24–9.
Article68. Rosenfeld BA, Dorman T, Breslow MJ, Pronovost P, Jenckes M, Zhang N, et al. Intensive care unit telemedicine: alternate paradigm for providing continuous intensivist care. Crit Care Med. 2000; 28(12):3925–31.
Article69. Zawada ET Jr, Herr P, Larson D, Fromm R, Kapaska D, Erickson D. Impact of an intensive care unit telemedicine program on a rural health care system. Postgrad Med. 2009; 121(3):160–70.
Article70. Morrison JL, Cai Q, Davis N, Yan Y, Berbaum ML, Ries M, et al. Clinical and economic outcomes of the electronic intensive care unit: results from two community hospitals. Crit Care Med. 2010; 38(1):2–8.
Article71. Lilly CM, Cody S, Zhao H, Landry K, Baker SP, Mc-Ilwaine J, et al. Hospital mortality, length of stay, and preventable complications among critically ill patients before and after tele-ICU reengineering of critical care processes. JAMA. 2011; 305(21):2175–83.
Article72. Young LB, Chan PS, Lu X, Nallamothu BK, Sasson C, Cram PM. Impact of telemedicine intensive care unit coverage on patient outcomes: a systematic review and meta-analysis. Arch Intern Med. 2011; 171(6):498–506.
Article73. Kim HJ. Professor Jinhyeong Kang “Digital healthcare will break the existing system” [Internet]. Seoul, Korea: HITnews;2021. [cited at 2022 Feb 3]. Available from: http://www.hitnews.co.kr/news/articleView.html?idxno=32291 .
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Recent Patient Health Monitoring Platforms Incorporating Internet of Things-Enabled Smart Devices
- Scoping Review of the Literature on Smart Healthcare for Older Adults
- The Prospect of the Fourth Industrial Revolution and Home Healthcare in Super-Aged Society
- Ubiquitous Health in Korea: Progress, Barriers, and Prospects
- Integration of information and communication technology in emergency medical services: The Chungbuk Smart Emergency Service Project