Korean J Gastroenterol.
2022 Jan;79(1):12-21. 10.4166/kjg.2021.086.
Nutritional Impact of Percutaneous Endoscopic Gastrostomy: A Retrospective Single-center Study
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Daejeon Veterans Hospital, Daejeon, Korea
- 2Department of Internal Medicine, Chungnam National University School of Medicine, Daejeon, Korea
- 3Division of Gastroenterology, Department of Internal Medicine, Chungnam National University Hospital, Daejeon, Korea
- 4Division of Disaster Statistics, Department of Fire and Disaster Prevention, Daejeon University, Daejeon, Korea
- 5Division of Gastroenterology, Department of Internal Medicine, Chungnam National University Sejong Hospital, Sejong, Korea
- KMID: 2525518
- DOI: http://doi.org/10.4166/kjg.2021.086
Abstract
- Background/Aims
Several conditions may cause difficulties with oral feeding. Percutaneous endoscopic gastrostomy (PEG) is commonly performed on patients who require enteral feeding for >2-3 weeks. This study examined the nutritional state of patients who required enteral feeding and underwent PEG to quantify the benefits of the procedure.
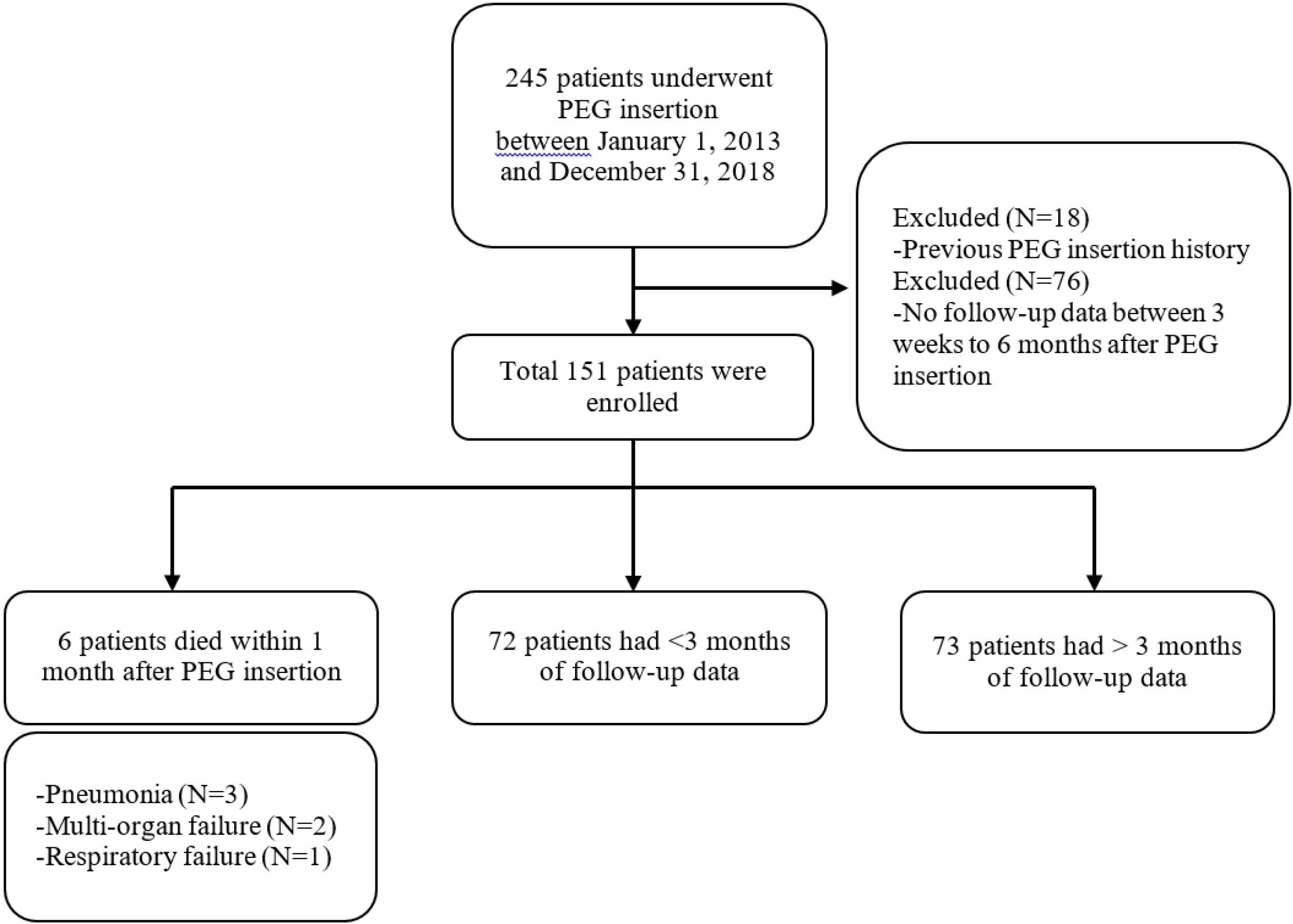
Methods
This retrospective study included patients who underwent PEG at the Chungnam National University Hospital between January 2013 and December 2018. A gastroenterologist performed all PEG procedures using the pull technique, and all patients were followed up for >3 weeks postoperatively. The BMI and lymphocyte count, along with the levels of hemoglobin, total protein, albumin, total cholesterol, BUN, and creatinine pre-PEG and between 3 weeks and 6 months post-PEG were evaluated.
Results
Overall, 151 patients (116 males; mean age 64.92 years) were evaluated. Of these patients, 112 (74.2%), 34 (22.5%), and five (3.3%) underwent PEG tube insertion because of neurological diseases, malignancy, and other conditions, respectively. The BMI and the hemoglobin, total protein, albumin, and total cholesterol levels were significantly higher post-PEG than pre-PEG.
Conclusions
These findings highlight the usefulness of PEG in the management of nutritionally poor patients with difficulties in feeding orally.
Keyword
Figure
Cited by 1 articles
-
Nationwide Survey for Pediatric Gastrostomy Tube Placement in Korea
Sangwoo Lee, Byung-Ho Choe, Ben Kang, Soon Chul Kim
J Korean Med Sci. 2022;37(40):e291. doi: 10.3346/jkms.2022.37.e291.
Reference
-
1. Deitch EA, Winterton J, Li M, Berg R. 1987; The gut as a portal of entry for bacteremia. Role of protein malnutrition. Ann Surg. 205:681–692. DOI: 10.1097/00000658-198706000-00010. PMID: 3592811. PMCID: PMC1493085.
Article2. Baeten C, Hoefnagels J. 1992; Feeding via nasogastric tube or percutaneous endoscopic gastrostomy. A comparison. Scand J Gastroenterol Suppl. 194:95–98. DOI: 10.3109/00365529209096035. PMID: 1298056.
Article3. Mekhail TM, Adelstein DJ, Rybicki LA, Larto MA, Saxton JP, Lavertu P. 2001; Enteral nutrition during the treatment of head and neck carcinoma: is a percutaneous endoscopic gastrostomy tube preferable to a nasogastric tube? Cancer. 91:1785–1790. DOI: 10.1002/1097-0142(20010501)91:9<1785::AID-CNCR1197>3.0.CO;2-1. PMID: 11335904.
Article4. Sim JS, Kim SY, Lee YJ, et al. 2017; Indication and clinical outcomes of percutaneous endoscopic gastrostomy: a single-center retrospective analysis. Korean J Helicobacter Up Gastrointest Res. 17:138–143. DOI: 10.7704/kjhugr.2017.17.3.138.
Article5. Masaki S, Kawamoto T. 2019; Comparison of long-term outcomes between enteral nutrition via gastrostomy and total parenteral nutrition in older persons with dysphagia: a propensity-matched cohort study. PLoS One. 14:e0217120. DOI: 10.1371/journal.pone.0217120. PMID: 31577813. PMCID: PMC6774498.
Article6. Meier R. 2009; Basics in clinical nutrition: endoscopic access (PEG and PEJ). E Spen Eur E J Clin Nutr Metab. 5:e216–e218. DOI: 10.1016/j.eclnm.2009.05.010.
Article7. Gauderer MW, Ponsky JL, Izant RJ Jr. 1980; Gastrostomy without laparotomy: a percutaneous endoscopic technique. J Pediatr Surg. 15:872–875. DOI: 10.1016/S0022-3468(80)80296-X. PMID: 6780678.
Article8. Deitel M, Bendago M, Spratt EH, Burul CJ, To TB. 1988; Percutaneous endoscopic gastrostomy by the "pull" and "introducer" methods. Can J Surg. 31:102–104. PMID: 3349370.9. Gauderer MW. 2001; Percutaneous endoscopic gastrostomy-20 years later: a historical perspective. J Pediatr Surg. 36:217–219. DOI: 10.1053/jpsu.2001.20058. PMID: 11150469.
Article10. Nunes G, Santos CA, Santos C, Fonseca J. 2016; Percutaneous endoscopic gastrostomy for nutritional support in dementia patients. Aging Clin Exp Res. 28:983–989. DOI: 10.1007/s40520-015-0485-2. PMID: 26582081.
Article11. Park RH, Allison MC, Lang J, et al. 1992; Randomised comparison of percutaneous endoscopic gastrostomy and nasogastric tube feeding in patients with persisting neurological dysphagia. BMJ. 304:1406–1409. DOI: 10.1136/bmj.304.6839.1406. PMID: 1628013. PMCID: PMC1882203.
Article12. Silander E, Nyman J, Bove M, Johansson L, Larsson S, Hammerlid E. 2012; Impact of prophylactic percutaneous endoscopic gastrostomy on malnutrition and quality of life in patients with head and neck cancer: a randomized study. Head Neck. 34:1–9. DOI: 10.1002/hed.21700. PMID: 21374756.
Article13. Löser C, Aschl G, Hébuterne X, et al. 2005; ESPEN guidelines on artificial enteral nutrition--percutaneous endoscopic gastrostomy (PEG). Clin Nutr. 24:848–861. DOI: 10.1016/j.clnu.2005.06.013. PMID: 16261664.14. Fortunato JE, Troy AL, Cuffari C, et al. 2010; Outcome after percutaneous endoscopic gastrostomy in children and young adults. J Pediatr Gastroenterol Nutr. 50:390–393. DOI: 10.1097/MPG.0b013e3181aed6f1. PMID: 20179645.
Article15. Rondanelli M, Talluri J, Peroni G, et al. 2018; Beyond body mass index. Is the Body Cell Mass Index (BCMI) a useful prognostic factor to describe nutritional, inflammation and muscle mass status in hospitalized elderly?: Body Cell Mass Index links in elderly. Clin Nutr. 37:934–939. DOI: 10.1016/j.clnu.2017.03.021. PMID: 28408051.
Article16. Trevisan C, Crippa A, Ek S, et al. 2019; Nutritional status, body mass index, and the risk of falls in community-dwelling older adults: a systematic review and meta-analysis. J Am Med Dir Assoc. 20:569–582.e7. DOI: 10.1016/j.jamda.2018.10.027. PMID: 30554987.
Article17. Perna S, Guido D, Grassi M, Rondanelli M. 2015; Association between muscle mass and adipo-metabolic profile: a cross-sectional study in older subjects. Clin Interv Aging. 10:499–504. DOI: 10.2147/CIA.S67872. PMID: 25759569. PMCID: PMC4345994.18. Araújo JP, Friões F, Azevedo A, et al. 2008; Cholesterol--a marker of nutritional status in mild to moderate heart failure. Int J Cardiol. 129:65–68. DOI: 10.1016/j.ijcard.2007.05.026. PMID: 17643521.
Article19. Xu SS, Li S, Xu HX, et al. 2020; Haemoglobin, albumin, lymphocyte and platelet predicts postoperative survival in pancreatic cancer. World J Gastroenterol. 26:828–838. DOI: 10.3748/wjg.v26.i8.828. PMID: 32148380. PMCID: PMC7052532.
Article20. O'Daly BJ, Walsh JC, Quinlan JF, et al. 2010; Serum albumin and total lymphocyte count as predictors of outcome in hip fractures. Clin Nutr. 29:89–93. DOI: 10.1016/j.clnu.2009.07.007. PMID: 19674819.21. Fletcher JP, Little JM, Guest PK. 1987; A comparison of serum transferrin and serum prealbumin as nutritional parameters. JPEN J Parenter Enteral Nutr. 11:144–147. DOI: 10.1177/0148607187011002144. PMID: 3108533.
Article22. Beck FK, Rosenthal TC. 2002; Prealbumin: a marker for nutritional evaluation. Am Fam Physician. 65:1575–1578. PMID: 11989633.23. Sjoquist KM, Renfro LA, Simes RJ, et al. 2018; Personalizing survival predictions in advanced colorectal cancer: the ARCAD nomogram project. J Natl Cancer Inst. 110:638–648. DOI: 10.1093/jnci/djx253. PMID: 29267900. PMCID: PMC6005015.
Article24. de Almeida JP, Vincent JL, Galas FR, et al. 2015; Transfusion requirements in surgical oncology patients: a prospective, randomized controlled trial. Anesthesiology. 122:29–38. DOI: 10.1097/ALN.0000000000000511. PMID: 25401417.25. hindi B, Hermanns T, Wei Y, et al. 2016; Identification of the best complete blood count-based predictors for bladder cancer outcomes in patients undergoing radical cystectomy. Br J Cancer. 114:207–212. DOI: 10.1038/bjc.2015.432. PMID: 26657651. PMCID: PMC4815810.
Article26. McGrane JM, Humes DJ, Acheson AG, Minear F, Wheeler JMD, Walter CJ. 2017; Significance of anemia in outcomes after neoadjuvant chemoradiotherapy for locally advanced rectal cancer. Clin Colorectal Cancer. 16:381–385. DOI: 10.1016/j.clcc.2017.03.016. PMID: 28456481.
Article27. Thongprayoon C, Cheungpasitporn W, Chewcharat A, Mao MA, Thirunavukkarasu S, Kashani KB. 2020; Risk of acute respiratory failure among hospitalized patients with various admission serum albumin levels: a cohort study. Medicine (Baltimore). 99:e19352. DOI: 10.1097/MD.0000000000019352. PMID: 32118775. PMCID: PMC7478795.28. Sergi G, Coin A, Enzi G, et al. 2006; Role of visceral proteins in detecting malnutrition in the elderly. Eur J Clin Nutr. 60:203–209. DOI: 10.1038/sj.ejcn.1602289. PMID: 16234837.
Article29. Vlassopoulos A, Combet E, Lean ME. 2014; Changing distributions of body size and adiposity with age. Int J Obes (Lond). 38:857–864. DOI: 10.1038/ijo.2013.216. PMID: 24247373.
Article30. Budzyński J, Tojek K, Wustrau B, et al. 2018; The "cholesterol paradox" among inpatients - retrospective analysis of medical documentation. Arch Med Sci Atheroscler Dis. 3:e46–e57. DOI: 10.5114/amsad.2018.74736. PMID: 30775589. PMCID: PMC6374572.
Article31. Reddy VS, Bui QT, Jacobs JR, et al. 2015; Relationship between serum low-density lipoprotein cholesterol and in-hospital mortality following acute myocardial infarction (the lipid paradox). Am J Cardiol. 115:557–562. DOI: 10.1016/j.amjcard.2014.12.006. PMID: 25727079.
Article32. Kuzuya M, Kanda S, Koike T, Suzuki Y, Iguchi A. 2005; Lack of correlation between total lymphocyte count and nutritional status in the elderly. Clin Nutr. 24:427–432. DOI: 10.1016/j.clnu.2005.01.003. PMID: 15896430.
Article33. Rahnemai-Azar AA, Rahnemaiazar AA, Naghshizadian R, Kurtz A, Farkas DT. 2014; Percutaneous endoscopic gastrostomy: indications, technique, complications and management. World J Gastroenterol. 20:7739–7751. DOI: 10.3748/wjg.v20.i24.7739. PMID: 24976711. PMCID: PMC4069302.
Article34. Pih GY, Na HK, Ahn JY, et al. 2018; Risk factors for complications and mortality of percutaneous endoscopic gastrostomy insertion. BMC Gastroenterol. 18:101. DOI: 10.1186/s12876-018-0825-8. PMID: 29954339. PMCID: PMC6025834.
Article35. Kähler G, Götz M, Senninger N. 2016. Therapeutic endoscopy in the Gastrointestinal Tract. 1st ed. Springer;New York: