Ann Surg Treat Res.
2022 Feb;102(2):83-89. 10.4174/astr.2022.102.2.83.
The effect of intraoperative neuromonitoring on the number of lymph nodes excised and recurrence when applied during neck dissection in cases of papillary thyroid cancer
- Affiliations
-
- 1Department of General Surgery, Ankara City Hospital, Ankara, Turkey
- KMID: 2525445
- DOI: http://doi.org/10.4174/astr.2022.102.2.83
Abstract
- Purpose
The aim of this study was to evaluate the effect of neuromonitoring on the number of lymph nodes (LNs) removed when applied during neck dissection.
Methods
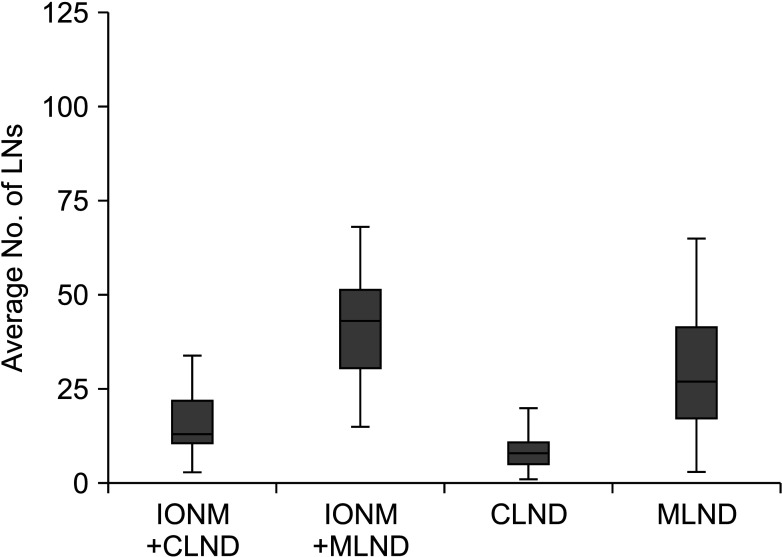
A total of 166 patients receiving neck dissection due to papillary thyroid cancer were separated into 2 groups (monitoring group, n = 76; non-monitoring group, n = 90).
Results
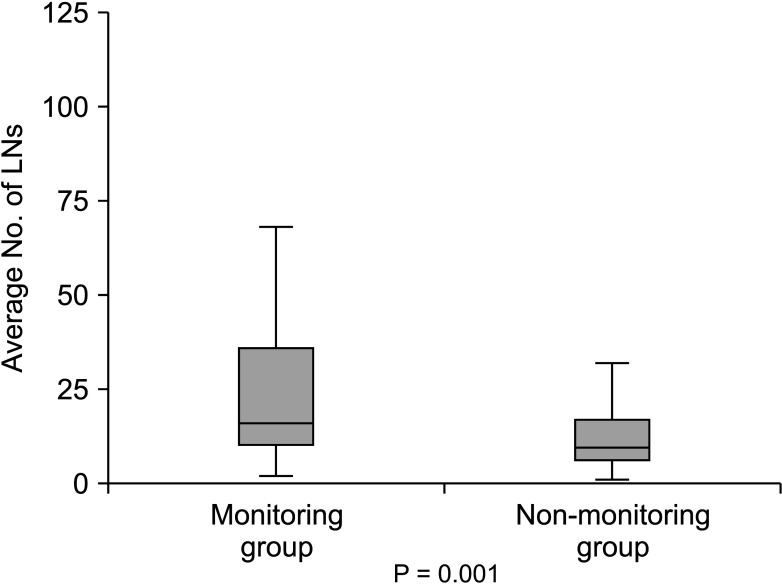
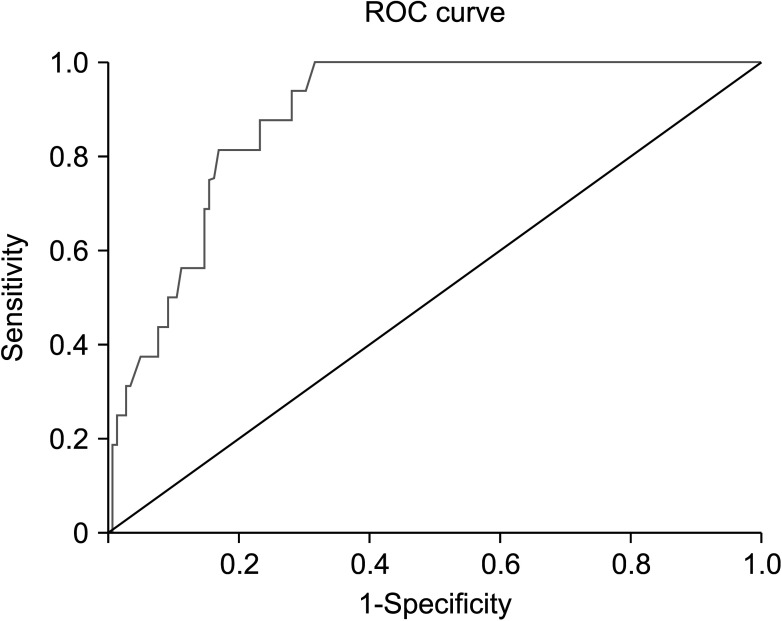
The number of LNs dissected was observed to be statistically significantly higher in the monitoring group (P = 0.001), and the difference between the groups in the number of positive LNs was significant (P = 0.031). There was seen to be a negative relationship between the number of positive LNs dissected and recurrence (r = –0.404, P = 0.005).
Conclusion
Intraoperative neuromonitoring during neck dissection makes a positive contribution to the prevention of the development of recurrence by increasing the number of LNs excised and the number of metastatic LNs.
Figure
Reference
-
1. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2018. CA Cancer J Clin. 2018; 68:7–30. PMID: 29313949.
Article2. Jeon MJ, Kim WG, Choi YM, Kwon H, Song DE, Lee YM, et al. Recent changes in the clinical outcome of papillary thyroid carcinoma with cervical lymph node metastasis. J Clin Endocrinol Metab. 2015; 100:3470–3477. PMID: 26120792.
Article3. Hu JQ, Wen D, Ma B, Zhang TT, Liao T, Shi X, et al. The extent of lymph node yield in central neck dissection can be affected by preoperative and intraoperative assessment and alter the prognosis of papillary thyroid carcinoma. Cancer Med. 2020; 9:1017–1024. PMID: 31854077.
Article4. Vas Nunes JH, Clark JR, Gao K, Chua E, Campbell P, Niles N, et al. Prognostic implications of lymph node yield and lymph node ratio in papillary thyroid carcinoma. Thyroid. 2013; 23:811–816. PMID: 23373961.
Article5. Lee YS, Nam KH, Chung WY, Chang HS, Park CS. Postoperative complications of thyroid cancer in a single center experience. J Korean Med Sci. 2010; 25:541–545. PMID: 20357995.
Article6. Araque KA, Gubbi S, Klubo-Gwiezdzinska J. Updates on the management of thyroid cancer. Horm Metab Res. 2020; 52:562–577. PMID: 32040962.
Article7. Ritter A, Ganly I, Wong RJ, Randolph GW, Shpitzer T, Bachar G, et al. Intraoperative nerve monitoring is used routinely by a significant majority of head and neck surgeons in thyroid surgery and impacts on extent of surgery: survey of the American Head and Neck Society. Head Neck. 2020; 42:1757–1764. PMID: 32026528.
Article8. Deniwar A, Kandil E, Randolph G. Electrophysiological neural monitoring of the laryngeal nerves in thyroid surgery: review of the current literature. Gland Surg. 2015; 4:368–375. PMID: 26425449.9. Dionigi G, Lombardi D, Lombardi CP, Carcoforo P, Boniardi M, Innaro N, et al. Intraoperative neuromonitoring in thyroid surgery: a point prevalence survey on utilization, management, and documentation in Italy. Updates Surg. 2014; 66:269–276. PMID: 25465057.
Article10. Duque CS, Dueñas JP, Marulanda M, Pérez D, Londoňo A, Roy S, et al. Phrenic nerve stimulation during neck dissection for advanced thyroid cancer involving level IV: is it worth doing it? Updates Surg. 2017; 69:83–87. PMID: 28194664.
Article11. Birinci Y, Genc A, Ecevit MC, Erdag TK, Guneri EA, Oztura I, et al. Spinal accessory nerve monitoring and clinical outcome results of nerve-sparing neck dissections. Otolaryngol Head Neck Surg. 2014; 151:253–259. PMID: 24748586.
Article12. Ryu YJ, Cho JS, Park MH, Yoon JH. Identifying risk factors of recurrence for clinically node negative papillary thyroid carcinoma with pathologic N1a. BMC Surg. 2019; 19:78. PMID: 31277631.
Article13. Calò PG, Medas F, Erdas E, Pit tau MR, Demontis R, Pisano G, et al. Role of intraoperative neuromonitoring of recurrent laryngeal nerves in the outcomes of surgery for thyroid cancer. Int J Surg. 2014; 12 Suppl 1:S213–S217. PMID: 24862668.
Article14. Loch-Wilkinson TJ, Stalberg PL, Sidhu SB, Sywak MS, Wilkinson JF, Delbridge LW. Nerve stimulation in thyroid surgery: is it really useful? ANZ J Surg. 2007; 77:377–380. PMID: 17497981.
Article15. Pisanu A, Porceddu G, Podda M, Cois A, Uccheddu A. Systematic review with meta-analysis of studies comparing intraoperative neuromonitoring of recurrent laryngeal nerves versus visualization alone during thyroidectomy. J Surg Res. 2014; 188:152–161. PMID: 24433869.
Article16. Chan WF, Lang BH, Lo CY. The role of intraoperative neuromonitoring of recurrent laryngeal nerve during thyroidectomy: a comparative study on 1000 nerves at risk. Surgery. 2006; 140:866–873. PMID: 17188132.
Article17. Thomusch O, Sekulla C, Machens A, Neumann HJ, Timmermann W, Dralle H. Validity of intra-operative neuromonitoring signals in thyroid surgery. Langenbecks Arch Surg. 2004; 389:499–503. PMID: 14722777.
Article18. Thomusch O, Sekul la C, Wal ls G, Machens A, Dralle H. Intraoperative neuromonitoring of surgery for benign goiter. Am J Surg. 2002; 183:673–678. PMID: 12095600.
Article19. Atallah I, Dupret A, Carpentier AS, Weingertner AS, Volkmar PP, Rodier JF. Role of intraoperative neuromonitoring of the recurrent laryngeal nerve in high-risk thyroid surgery. J Otolaryngol Head Neck Surg. 2009; 38:613–618. PMID: 19958722.20. Chen HC, Pei YC, Fang TJ. Risk factors for thyroid surgery-related unilateral vocal fold paralysis. Laryngoscope. 2019; 129:275–283. PMID: 30284255.
Article21. Ahn D, Sohn JH, Park JY. Surgical complications and recurrence after central neck dissection in cN0 papillary thyroid carcinoma. Auris Nasus Larynx. 2014; 41:63–68. PMID: 23886706.
Article22. Liu X, Zhang D, Zhang G, Zhao L, Zhou L, Fu Y, et al. Laryngeal nerve morbidity in 1.273 central node dissections for thyroid cancer. Surg Oncol. 2018; 27:A21–A25. PMID: 29525322.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Regional Lymph Node Metastasis in Papillary Thyroid Cancer
- The Patterns of Lateral Neck Node Involvement in Papillary Thyroid Carcinoma
- Comparative Results of Modified Radical Neck Dissection and Level I Preserving Selective Neck Dissection for Metastatic Papillary Carcinoma of the Thyroid
- Central Neck Lymph Node Metastasis from Papillary Thyroid Cancers
- A Clinical Review of Lymph Node Metastases for Papillary Thyroid Cancer