J Stroke.
2022 Jan;24(1):118-127. 10.5853/jos.2021.02355.
Apixaban for Secondary Stroke Prevention: Coexistant Cerebral Atherosclerosis May Increase Recurrent Strokes
- Affiliations
-
- 1Department of Neurology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Neurology, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Department of Neurology, Chungbuk National University Hospital, Chungbuk National University College of Medicine, Cheongju, Korea
- 4Department of Neurology, Bundang Jesaeng General Hospital, Daejin Medical Center, Seongnam, Korea
- 5Department of Neurology, Chungnam National University Hospital, Chungnam National University College of Medicine, Daejeon, Korea
- 6Department of Neurology, Inje University Busan Paik Hospital, College of Medicine, Inje University, Busan, Korea
- 7Department of Neurology, Inje University Ilsan Paik Hospital, College of Medicine, Inje University, Goyang, Korea
- 8Bristol Myers Squibb Korea, Seoul, Korea
- KMID: 2525337
- DOI: http://doi.org/10.5853/jos.2021.02355
Abstract
- Background and Purpose
Oral anticoagulants are needed in stroke patients with atrial fibrillation (AF) for the prevention of recurrent stroke. However, the risk of major events or bleeding may be greater in stroke patients than in those without, because the presence of cerebral atherosclerosis or small vessel disease may increase these risks. This study aimed to investigate the outcomes of apixaban-treated stroke patients with AF and assess whether these factors are associated with the outcome.
Methods
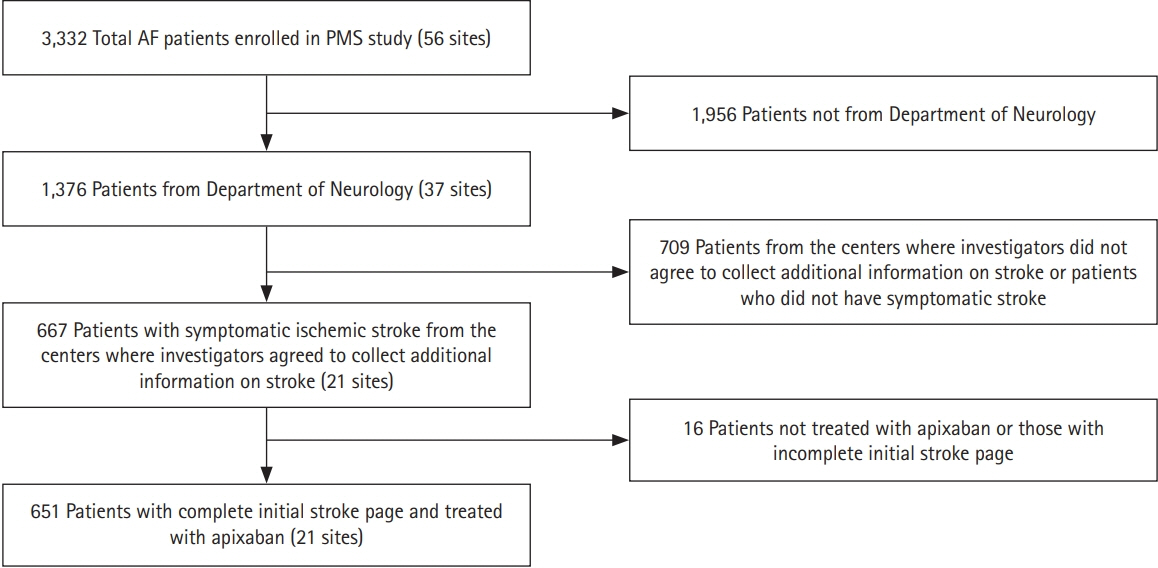
This was a sub-analysis of stroke patients with AF enrolled in a prospective, open-label, multicenter, post-marketing surveillance study in South Korea, who were treated with apixaban and underwent magnetic resonance imaging (MRI) (Clinical trial registration: NCT01885598).
Results
A total of 651 patients (mean age, 72.5±8.7 years) received apixaban for a mean duration of 82.7±37.4 weeks. Fifty-three bleeding events occurred in 39 patients (6.0%), and 10 (1.5%) experienced major bleeding. Seventeen patients (2.6%) had major events (stroke, n=15, 2.3%; all ischemic), systemic embolism (n=1, 0.2%), and death (n=3, 0.5%). MRI data showed no significant association between white matter ischemic changes and microbleeds, and major events or bleeding. Patients with cerebral atherosclerotic lesions had a higher rate of major events than those without (4.6% [n=10/219] vs. 1.7% [n=7/409], P=0.0357), which partly explains the increased prevalence of major outcomes in this group versus patients without stroke (0.7%, P=0.0002).
Conclusions
Apixaban is generally safe for patients with ischemic stroke. Increased primary outcomes in stroke patients may in part be attributed to the presence of cerebral atherosclerotic lesions, suggesting that further studies are needed to establish therapeutic strategies in this population.
Keyword
Figure
Cited by 1 articles
-
Occurrence of Ischemic Stroke in Patients With Atrial Fibrillation Receiving Non-Vitamin K Oral Anticoagulants: Causes and Prevention Strategies
Oh Young Bang, Kyoung-Min Park, Dong Seop Jeong
J Stroke. 2023;25(2):199-213. doi: 10.5853/jos.2022.03552.
Reference
-
References
1. Steffel J, Verhamme P, Potpara TS, Albaladejo P, Antz M, Desteghe L, et al. The 2018 European Heart Rhythm Association practical guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Eur Heart J. 2018; 39:1330–1393.
Article2. Joung B, Lee JM, Lee KH, Kim TH, Choi EK, Lim WH, et al. 2018 Korean guideline of atrial fibrillation management. Korean Circ J. 2018; 48:1033–1080.
Article3. Granger CB, Alexander JH, McMurray JJ, Lopes RD, Hylek EM, Hanna M, et al. Apixaban versus warfarin in patients with atrial fibrillation. N Engl J Med. 2011; 365:981–992.4. Goto S, Zhu J, Liu L, Oh BH, Wojdyla DM, Aylward P, et al. Efficacy and safety of apixaban compared with warfarin for stroke prevention in patients with atrial fibrillation from East Asia: a subanalysis of the Apixaban for Reduction in Stroke and Other Thromboembolic Events in Atrial Fibrillation (ARISTOTLE) Trial. Am Heart J. 2014; 168:303–309.
Article5. Kirchhof P, Benussi S, Kotecha D, Ahlsson A, Atar D, Casadei B, et al. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur J Cardiothorac Surg. 2016; 50:e1–e88.
Article6. Park J, Lee SR, Choi EK, Kwon S, Jung JH, Han KD, et al. Effectiveness and safety of direct oral anticoagulant for secondary prevention in Asians with atrial fibrillation. J Clin Med. 2019; 8:2228.
Article7. Yasaka M, Umeyama M, Kataoka H, Inoue H. Secondary stroke prevention with apixaban in nonvalvular atrial fibrillation: a subgroup analysis of the STANDARD study. J Stroke Cerebrovasc Dis. 2020; 29:105034.
Article8. Das AS, Regenhardt RW, Vernooij MW, Blacker D, Charidimou A, Viswanathan A. Asymptomatic cerebral small vessel disease: insights from population-based studies. J Stroke. 2019; 21:121–138.
Article9. Fazekas F, Chawluk JB, Alavi A, Hurtig HI, Zimmerman RA. MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am J Roentgenol. 1987; 149:351–356.
Article10. Inoue H, Umeyama M, Yamada T, Hashimoto H, Komoto A, Yasaka M. Safety and effectiveness of apixaban in Japanese patients with nonvalvular atrial fibrillation in clinical practice: a regulatory postmarketing surveillance, the STANDARD study. J Arrhythm. 2019; 35:506–514.11. Kim BS, Chung PW, Park KY, Won HH, Bang OY, Chung CS, et al. Burden of intracranial atherosclerosis is associated with long-term vascular outcome in patients with ischemic stroke. Stroke. 2017; 48:2819–2826.
Article12. Park JH, Chung JW, Bang OY, Kim GM, Choi KH, Park MS, et al. Atherosclerotic burden and vascular risk in stroke patients with atrial fibrillation. Stroke. 2021; 52:1662–1672.
Article13. Kim YD, Cha MJ, Kim J, Lee DH, Lee HS, Nam CM, et al. In- creases in cerebral atherosclerosis according to CHADS2 scores in patients with stroke with nonvalvular atrial fibrillation. Stroke. 2011; 42:930–934.14. Kim BJ, Lee SH. Prognostic impact of cerebral small vessel disease on stroke outcome. J Stroke. 2015; 17:101–110.
Article15. Du H, Wilson D, Ambler G, Banerjee G, Shakeshaft C, Cohen H, et al. Small vessel disease and ischemic stroke risk during anticoagulation for atrial fibrillation after cerebral ischemia. Stroke. 2021; 52:91–99.16. Steinberg BA, Shrader P, Thomas L, Ansell J, Fonarow GC, Gersh BJ, et al. Off-label dosing of non-vitamin K antagonist oral anticoagulants and adverse outcomes: the ORBIT-AF II Registry. J Am Coll Cardiol. 2016; 68:2597–2604.17. Bassand JP, Virdone S, Badoz M, Verheugt F, Camm AJ, Cools F, et al. Bleeding and related mortality with NOACs and VKAs in newly diagnosed atrial fibrillation: results from the GARFIELD-AF registry. Blood Adv. 2021; 5:1081–1091.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Secondary Prevention as Integral Part of Stroke Rehabilitation
- Epidemiology and Characteristics of Recurrent Stroke: The Occurrence Type of Restroke is Similar as Previous Stroke
- Pharmacological Secondary Prevention of Ischemic Stroke
- Mechanisms of Recurrence in Subtypes of Ischemic Stroke: A Hospital-based Follow-up Study
- Dyslipidemia Treatment and Cerebrovascular Disease: Evidence Regarding the Mechanism of Stroke