Brain Tumor Res Treat.
2022 Jan;10(1):22-28. 10.14791/btrt.2022.10.e30.
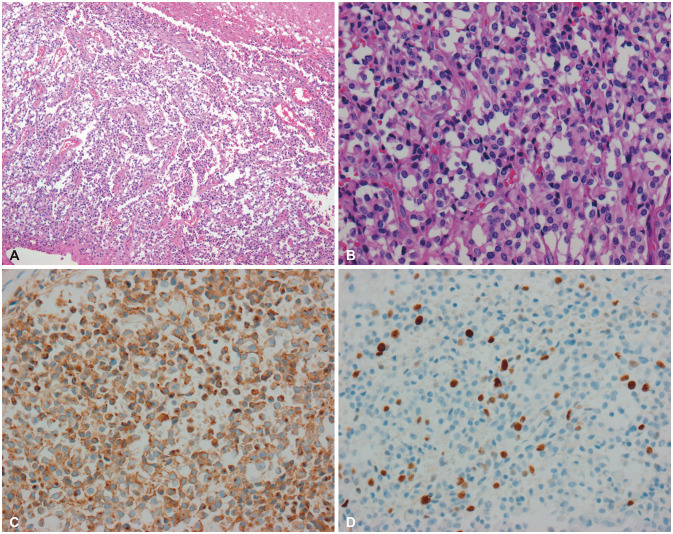
Extraventricular Neurocytoma: Clinical Investigation of Heterogenous Prognosis
- Affiliations
-
- 1Department of Neurological Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2525298
- DOI: http://doi.org/10.14791/btrt.2022.10.e30
Abstract
- Background
Extraventricular neurocytoma (EVN) is an extremely rare neuronal neoplasm that arises outside the ventricle. The clinical implication of the heterogenous prognosis of this rare tumor has not yet been clarified. Herein, we analyzed our institutional series of EVN.
Methods
A total of eight consecutive cases were enrolled and investigated. The prognosis of EVN was analyzed and compared to that of central neurocytoma (CN).
Results
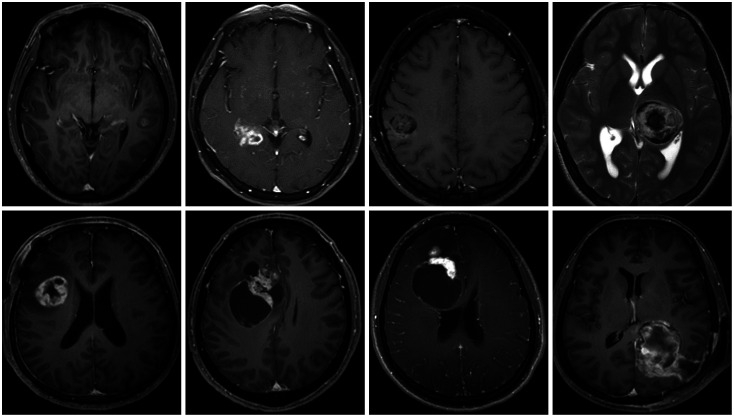
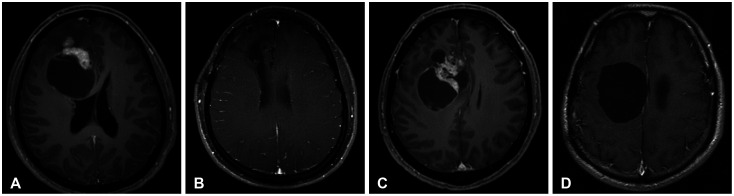
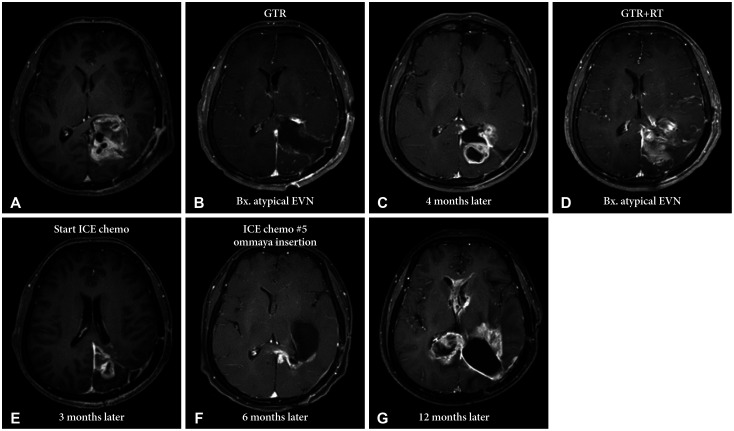
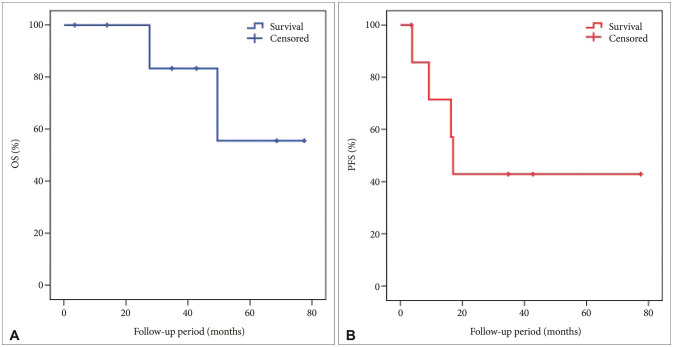
There were two male and six female patients, and the median age was 36.5 years. The median tumor size was 38 mm, and the most common location of the tumor was the frontal lobe (3, 37.5%), followed by the parietal and temporal lobes. In brain imaging, four (50%) tumors showed peritumoral edema and three (37.5%) tumors showed calcification. All patients underwent gross total resection, and two (25%) underwent adjuvant radiotherapy. The 5-year overall survival (OS) was 55.6%, and the 2-year progression-free survival (PFS) was 42.9%. The OS and PFS of EVN were poor compared to those of CN. Although EVN is a single disease entity, individual patients showed varying prognosis. One patient showed no recurrence during the 7-year follow-up period; however, another patient had a recurrence 4 months after surgery and died 2 years later.
Conclusion
EVN may be a heterogenous disease entity. Additional cases with long-term followup are needed to develop optimal management protocols.
Keyword
Figure
Reference
-
1. Hassoun J, Gambarelli D, Grisoli F, Pellet W, Salamon G, Pellissier JF, et al. Central neurocytoma. An electron-microscopic study of two cases. Acta Neuropathol. 1982; 56:151–156. PMID: 7064664.2. Patil AS, Menon G, Easwer HV, Nair S. Extraventricular neurocytoma, a comprehensive review. Acta Neurochir (Wien). 2014; 156:349–354. PMID: 24357019.
Article3. Yang GF, Wu SY, Zhang LJ, Lu GM, Tian W, Shah K. Imaging findings of extraventricular neurocytoma: report of 3 cases and review of the literature. AJNR Am J Neuroradiol. 2009; 30:581–585. PMID: 18842767.
Article4. Kane AJ, Sughrue ME, Rutkowski MJ, Aranda D, Mills SA, Lehil M, et al. Atypia predicting prognosis for intracranial extraventricular neurocytomas. J Neurosurg. 2012; 116:349–354. PMID: 22054208.
Article5. Söylemezoglu F, Scheithauer BW, Esteve J, Kleihues P. Atypical central neurocytoma. J Neuropathol Exp Neurol. 1997; 56:551–556. PMID: 9143268.
Article6. Xu L, Ouyang Z, Wang J, Liu Z, Fang J, Du J, et al. A clinicopathologic study of extraventricular neurocytoma. J Neurooncol. 2017; 132:75–82. PMID: 27864704.
Article7. Liu K, Wen G, Lv XF, Deng YJ, Deng YJ, Hou GQ, et al. MR imaging of cerebral extraventricular neurocytoma: a report of 9 cases. AJNR Am J Neuroradiol. 2013; 34:541–546. PMID: 23042917.
Article8. Louis DN, Ohgaki H, Wiestler OD, Cavenee WK, Burger PC, Jouvet A, et al. The 2007 WHO classification of tumours of the central nervous system. Acta Neuropathol. 2007; 114:97–109. PMID: 17618441.
Article9. Louis DN, Perry A, Reifenberger G, von Deimling A, Figarella-Branger D, Cavenee WK, et al. The 2016 World Health Organization classification of tumors of the central nervous system: a summary. Acta Neuropathol. 2016; 131:803–820. PMID: 27157931.
Article10. Möller-Hartmann W, Krings T, Brunn A, Korinth M, Thron A. Proton magnetic resonance spectroscopy of neurocytoma outside the ventricular region--case report and review of the literature. Neuroradiology. 2014; 44:230–234.
Article11. Brown DM, Karlovits S, Lee LH, Kim K, Rothfus WE, Brown HG. Management of neurocytomas: case report and review of the literature. Am J Clin Oncol. 2001; 24:272–278. PMID: 11404499.12. Choi H, Park SH, Kim DG, Paek SH. Atypical extraventricular neurocytoma. J Korean Neurosurg Soc. 2011; 50:381–384. PMID: 22200023.
Article13. Louis DN, Perry A, Wesseling P, Brat DJ, Cree IA, Figarella-Branger D, et al. The 2021 WHO classification of tumors of the central nervous system: a summary. Neuro Oncol. 2021; 23:1231–1251. PMID: 34185076.
Article14. Brat DJ, Scheithauer BW, Eberhart CG, Burger PC. Extraventricular neurocytomas: pathologic features and clinical outcome. Am J Surg Pathol. 2001; 25:1252–1260. PMID: 11688459.15. Byun J, Hong SH, Yoon MJ, Kwon SM, Cho YH, Kim JH, et al. Prognosis and treatment outcomes of central neurocytomas: clinical interrogation based on a single center experience. J Neurooncol. 2018; 140:669–677. PMID: 30225773.
Article16. Rades D, Schild SE, Fehlauer F. Defining the best available treatment for neurocytomas in children. Cancer. 2004; 101:2629–2632. PMID: 15494975.
Article17. Rades D, Fehlauer F, Schild SE. Treatment of atypical neurocytomas. Cancer. 2004; 100:814–817. PMID: 14770439.
Article18. Jeon C, Cho KR, Choi JW, Kong DS, Seol HJ, Nam DH, et al. Gamma Knife radiosurgery as a primary treatment for central neurocytoma. J Neurosurg. 2021; 134:1459–1465.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Extraventricular Cystic Neurocytoma
- 5-Aminolevulinic Acid Fluorescence Discriminates the Histological Grade of Extraventricular Neurocytoma
- Atypical Extraventricular Neurocytoma
- Recurrent Extraventricular Neurocytoma with Malignant Glial Differentiation
- Central Neurocytoma Originated from Atrium with Malignant Trans formation: A Case Report