J Yeungnam Med Sci.
2022 Jan;39(1):77-80. 10.12701/yujm.2021.01053.
Stent graft treatment of an ilioenteric fistula secondary to radiotherapy: a case report
- Affiliations
-
- 1Department of Radiology, Pusan National University Yangsan Hospital, Pusan National University College of Medicine, Busan, Korea
- KMID: 2525033
- DOI: http://doi.org/10.12701/yujm.2021.01053
Abstract
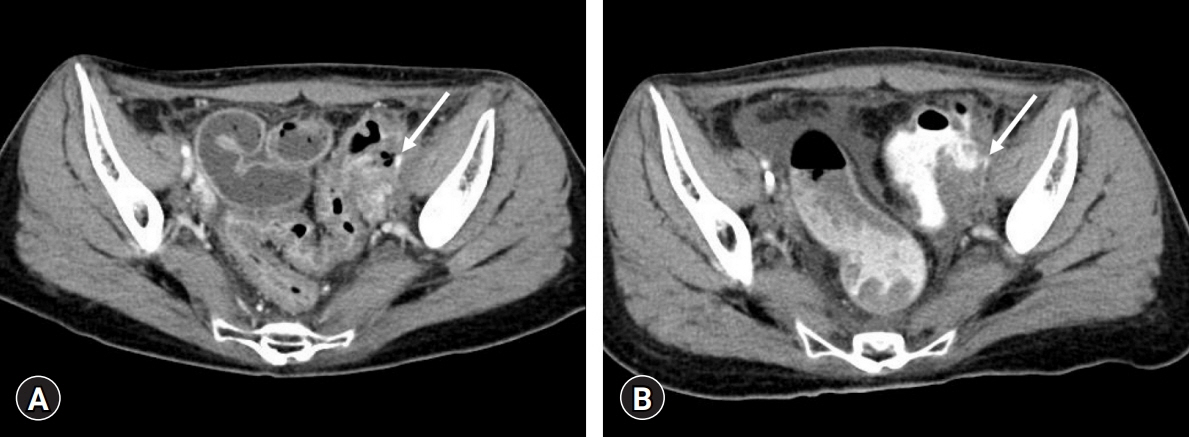
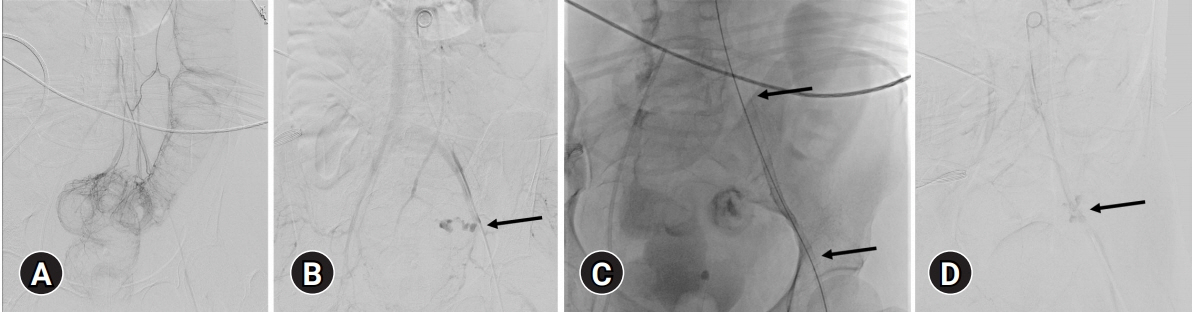
- Fistulas between the arteries and the gastrointestinal tract are rare but can be fatal. We present a case of an ilioenteric fistula between the left external iliac artery and sigmoid colon caused by radiotherapy for cervical cancer, which was treated with endovascular management using a stent graft. A 38-year-old woman underwent concurrent chemoradiotherapy for cervical cancer recurrence. Approximately 9 months later, the patient suddenly developed hematochezia. On her first visit to the emergency room of our hospital, computed tomography (CT) images did not reveal extravasation of contrast media. However, 8 hours later, she revisited the emergency room because of massive hematochezia with a blood pressure of 40/20 mmHg and a heart rate of 150 beats per minute. At that time, CT images showed the presence of contrast media in almost the entire colon. The patient was referred to the angiography room at our hospital for emergency angiography. Inferior mesenteric arteriography did not reveal any source of bleeding. Pelvic arteriography showed contrast media extravasation from the left external iliac artery to the sigmoid colon; this was diagnosed as an ilioenteric fistula and treated with a stent graft. When the bleeding focus is not detected on visceral angiography despite massive arterial bleeding, pelvic arteriography is recommended, especially in patients with a history of pelvic surgery or radiotherapy.
Keyword
Figure
Reference
-
References
1. Leonhardt H, Mellander S, Snygg J, Lönn L. Endovascular management of acute bleeding arterioenteric fistulas. Cardiovasc Intervent Radiol. 2008; 31:542–9.2. Hicks TD, Kedora JC, Shutze WP. Treatment of an ilioenteric fistula with an Amplatzer Vascular Plug. J Vasc Surg. 2011; 54:1495–7.3. Voorhoeve R, Moll FL, de Letter JA, Bast TJ, Wester JP, Slee PH. Primary aortoenteric fistula: report of eight new cases and review of the literature. Ann Vasc Surg. 1996; 10:40–8.4. Saers SJ, Scheltinga MR. Primary aortoenteric fistula. Br J Surg. 2005; 92:143–52.5. Vu QD, Menias CO, Bhalla S, Peterson C, Wang LL, Balfe DM. Aortoenteric fistulas: CT features and potential mimics. Radiographics. 2009; 29:197–209.6. Armstrong PA, Back MR, Wilson JS, Shames ML, Johnson BL, Bandyk DF. Improved outcomes in the recent management of secondary aortoenteric fistula. J Vasc Surg. 2005; 42:660–6.7. Champion MC, Sullivan SN, Coles JC, Goldbach M, Watson WC. Aortoenteric fistula. Incidence, presentation recognition, and management. Ann Surg. 1982; 195:314–7.8. Antoniou GA, Koutsias S, Antoniou SA, Georgiakakis A, Lazarides MK, Giannoukas AD. Outcome after endovascular stent graft repair of aortoenteric fistula: a systematic review. J Vasc Surg. 2009; 49:782–9.9. Hirakata R, Hasuo K, Yasumori K, Yoshida K, Masuda K. Arterioenteric fistulae: diagnosis and treatment by angiography. Clin Radiol. 1991; 43:328–30.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of High-Flow Carotid Cavernous Fistula Using a Graft Stent: Case Report
- Infection of the Aortic Stent Graft to Treat Arterioureteral Fistula
- Successful Treatment of an Iatrogenic Hepatic Arteriobiliary Fistula with an Endobiliary Covered Stent Graft: A Case Report
- Endovascular Treatment of Arteriovenous Fistula with Pseudoaneurysm at Popliteal Fossa Using a PTFE Stent-graft: A Case Report
- Endovascular Stent-Graft Treatment of a Traumatic Vertebral Artery Pseudoaneurysm and Vertebrojugular Fistula