Korean J Orthod.
2022 Jan;52(1):66-74. 10.4041/kjod.2022.52.1.66.
Comparison of one-jaw and two-jaw orthognathic surgery in patients with skeletal Class III malocclusion using data from 10 multi-centers in Korea: Part I. Demographic and skeletodental characteristics
- Affiliations
-
- 1Division of Orthodontics, Department of Dentistry, Hanyang University Hospital, Seoul, Korea
- 2Department of Statistics, College of Natural Sciences, Chonnam National University, Gwangju, Korea
- 3Department of Orthodontics, School of Dentistry, Kyungpook National University, Daegu, Korea
- 4Department of Orthodontics, School of Dentistry, Wonkwang University, Iksan, Korea
- 5Department of Orthodontics, College of Medicine, Ewha Womans University, Seoul, Korea
- 6Department of Orthodontics, Kyung Hee University School of Dentistry, Seoul, Korea
- 7Department of Orthodontics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 8Department of Orthodontics, Institute of Oral Health Science, Ajou University School of Medicine, Suwon, Korea
- 9Department of Orthodontics, College of Dentistry, Chosun University, Gwangju, Korea
- 10Department of Orthodontics, School of Dentistry, Dental Research Institute, Seoul National University, Seoul, Korea
- 11Department of Orthodontics, Chonnam National University School of Dentistry, Gwangju, Korea
- KMID: 2524903
- DOI: http://doi.org/10.4041/kjod.2022.52.1.66
Abstract
Objective
To investigate demographic and skeletodental characteristics of one-jaw (1J-OGS) and two-jaw orthognathic surgery (2J-OGS) in patients with skeletal Class III malocclusion.
Methods
750 skeletal Class III patients who underwent OGS at 10 university hospitals in Korea between 2015 and 2019 were investigated; after dividing them into the 1J-OGS (n = 186) and 2J-OGS groups (n = 564), demographic and skeletodental characteristics were statistically analyzed.
Results
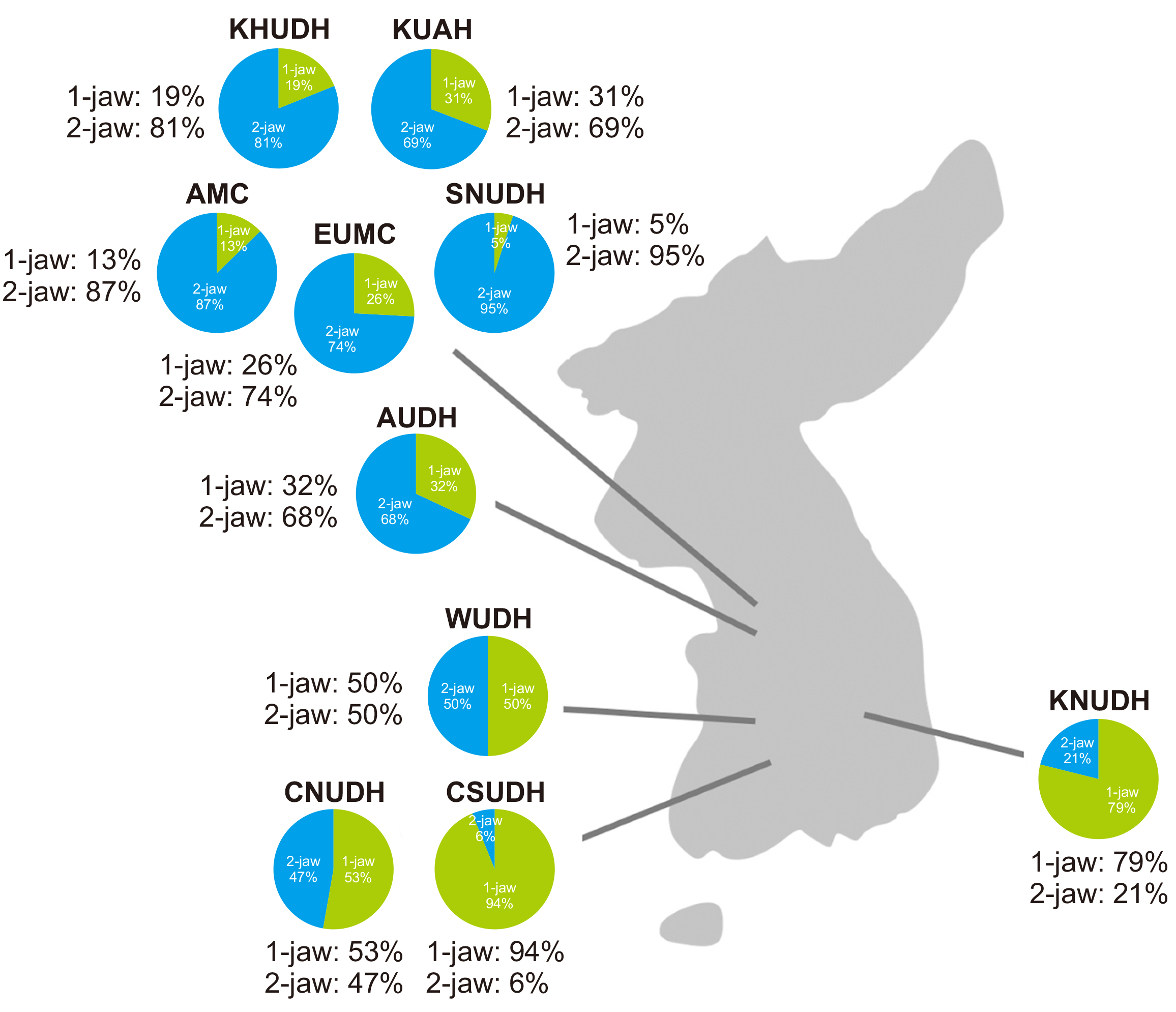
2J-OGS was more frequently performed than 1J-OGS (75.2 vs. 24.8%), despite regional differences (capital area vs. provinces, 86.6 vs. 30.7%, p < 0.001). Males outnumbered females, and their mean operation age was older in both groups. Regarding dental patterns, the most frequent maxillary arch length discrepancy (ALD) was crowding in the 1J-OGS group (52.7%, p < 0.001) and spacing in the 2J-OGS group (40.4%, p < 0.001). However, the distribution of skeletal pattern was not significantly different between the two groups (all p > 0.05). The most prevalent skeletal patterns in both groups were hyper-divergent pattern (50.0 and 54.4%, respectively) and left-side chin point deviation (both 49.5%). Maxillary spacing (odds ratio [OR], 3.645; p < 0.001) increased the probability of 2J-OGS, while maxillary crowding (OR, 0.672; p < 0.05) and normo-divergent pattern (OR, 0.615; p < 0.05) decreased the probability of 2J-OGS.
Conclusions
In both groups, males outnumbered females, and their mean operation age was older. The most frequent ALD was crowding in the 1J-OGS group, and spacing in the 2J-OGS group, while skeletal characteristics were not significantly different between the two groups.
Figure
Reference
-
1. Zamboni R, de Moura FRR, Brew MC, Rivaldo EG, Braz MA, Grossmann E, et al. 2019; Impacts of orthognathic surgery on patient satisfaction, overall quality of life, and oral health-related quality of life: a systematic literature review. Int J Dent. 2019:2864216. DOI: 10.1155/2019/2864216. PMID: 31316563. PMCID: PMC6604419.
Article2. Athanasiou AE, Melsen B, Eriksen J. 1989; Concerns, motivation, and experience of orthognathic surgery patients: a retrospective study of 152 patients. Int J Adult Orthodon Orthognath Surg. 4:47–55. PMID: 2600491.3. Proffit WR, Jackson TH, Turvey TA. 2013; Changes in the pattern of patients receiving surgical-orthodontic treatment. Am J Orthod Dentofacial Orthop. 143:793–8. DOI: 10.1016/j.ajodo.2013.01.014. PMID: 23726329. PMCID: PMC4034071.
Article4. Proffit WR, Phillips C, Dann C 4th. 1990; Who seeks surgical-orthodontic treatment? Int J Adult Orthodon Orthognath Surg. 5:153–60. PMID: 2098450.5. Boeck EM, Lunardi N, Pinto Ados S, Pizzol KE, Boeck Neto RJ. 2011; Occurrence of skeletal malocclusions in Brazilian patients with dentofacial deformities. Braz Dent J. 22:340–5. DOI: 10.1590/S0103-64402011000400014. PMID: 21861036.
Article6. Castro V, do Prado CJ, Neto AI, Zanetta-Barbosa D. 2013; Assessment of the epidemiological profile of patients with dentofacial deformities who underwent orthognathic surgery. J Craniofac Surg. 24:e271–5. DOI: 10.1097/SCS.0b013e31828f28f3. PMID: 23714988.
Article7. Eslamipour F, Borzabadi-Farahani A, Le BT, Shahmoradi M. 2017; A retrospective analysis of dentofacial deformities and orthognathic surgeries. Ann Maxillofac Surg. 7:73–7. DOI: 10.4103/ams.ams_104_16. PMID: 28713739. PMCID: PMC5502519.8. Olkun HK, Borzabadi-Farahani A, Uçkan S. 2019; Orthognathic surgery treatment need in a Turkish adult population: a retrospective study. Int J Environ Res Public Health. 16:1881. DOI: 10.3390/ijerph16111881. PMID: 31141986. PMCID: PMC6603578.
Article9. Baik HS, Kim KH, Park Y. 1995; The distributions and trends in malocclusion patients- a 10 year study of 2155 patients from YDSH. Korean J Orthod. 25:87–100.10. Hwang MS, Yoon YJ, Kim KW. 2001; An epidemiologic study on the orthodontic patients who visited Department of Orthodontics, Chosun University Dental Hospital last 10 years (1990-1999). Korean J Orthod. 31:283–300.11. Im DH, Kim TW, Nahm DS, Chang YI. 2003; Current trends in orthodontic patients in Seoul National University Dental Hospital. Korean J Orthod. 33:63–72.12. Lee CH, Park HH, Seo BM, Lee SJ. 2017; Modern trends in Class III orthognathic treatment: a time series analysis. Angle Orthod. 87:269–78. DOI: 10.2319/043016-349.1. PMID: 27513030. PMCID: PMC8384372.
Article13. Lee HY, Ahn Y, Park LY, Soh BS, Jo SK, Ko SO, et al. 2004; A clinicostastical study of inpatients of orthognathic surgery between 1993-2002. J Korean Assoc Maxillofac Plast Reconstr Surg. 26:477–83.14. Lee SH, Park IS, Lee CH, Kwon TG, Yun M, Deng F. 2005; Clinicostatistical study on orthognathic surgery in our department. J Korean Assoc Oral Maxillofac Surg. 31:255–9.15. Piao Y, Kim SJ, Yu HS, Cha JY, Baik HS. 2016; Five-year investigation of a large orthodontic patient population at a dental hospital in South Korea. Korean J Orthod. 46:137–45. DOI: 10.4041/kjod.2016.46.3.137. PMID: 27226959. PMCID: PMC4879316.
Article16. Jung MH. 2012; Age, extraction rate and jaw surgery rate in Korean orthodontic clinics and small dental hospitals. Korean J Orthod. 42:80–6. DOI: 10.4041/kjod.2012.42.2.80. PMID: 23112936. PMCID: PMC3481968.
Article17. Lee SJ, Suhr CH. 1994; Recognition of malocclusion and orthodontic treatment need of 7-18 year-old Korean adolescent. Korean J Orthod. 24:367–94.18. Sato FR, Mannarino FS, Asprino L, de Moraes M. 2014; Prevalence and treatment of dentofacial deformities on a multiethnic population: a retrospective study. Oral Maxillofac Surg. 18:173–9. DOI: 10.1007/s10006-013-0396-3. PMID: 23408297.
Article19. Sato S. 1994; Case report: developmental characterization of skeletal Class III malocclusion. Angle Orthod. 64:105–11. discussion 111–2. DOI: 10.1043/0003-3219(1994)064<0105:CRDCOS>2.0.CO;2. PMID: 8010518.20. Haraguchi S, Takada K, Yasuda Y. 2002; Facial asymmetry in subjects with skeletal Class III deformity. Angle Orthod. 72:28–35. DOI: 10.1043/0003-3219(2002)072<0028:FAISWS>2.0.CO;2. PMID: 11843270.21. Arad I, Jandu J, Bassett P, Fleming PS. 2011; Influence of single-jaw surgery vs bimaxillary surgery on the outcome and duration of combined orthodontic-surgical treatment. Angle Orthod. 81:983–7. DOI: 10.2319/030211-150.1. PMID: 21615211.
Article22. Bailey LJ, Duong HL, Proffit WR. 1998; Surgical Class III treatment: long-term stability and patient perceptions of treatment outcome. Int J Adult Orthodon Orthognath Surg. 13:35–44. PMID: 9558534.23. Bailey LT, Proffit WR, White RP Jr. 1995; Trends in surgical treatment of Class III skeletal relationships. Int J Adult Orthodon Orthognath Surg. 10:108–18. PMID: 9081996.24. Wolford LM. 2000; The sagittal split ramus osteotomy as the preferred treatment for mandibular prognathism. J Oral Maxillofac Surg. 58:310–2. DOI: 10.1016/S0278-2391(00)90062-4. PMID: 10716114.
Article25. Kim DK, Baek SH. 2013; Change in maxillary incisor inclination during surgical-orthodontic treatment of skeletal Class III malocclusion: comparison of extraction and nonextraction of the maxillary first premolars. Am J Orthod Dentofacial Orthop. 143:324–35. DOI: 10.1016/j.ajodo.2012.10.014. PMID: 23452966.
Article26. Xu B, Qin K. 2012; The effect of extraction and non-extraction decompensation to bimaxillary orthognathic surgery in skeletal class III malocclusion. Hua Xi Kou Qiang Yi Xue Za Zhi. 30:143–7. Chinese. PMID: 22594229.27. Bang SM, Kwon YD, Kim SJ, Lee BS, Choi BJ, Ohe JY, et al. 2012; Postoperative stability of 2-jaw surgery with clockwise rotation of the occlusal plane. J Craniofac Surg. 23:486–90. DOI: 10.1097/SCS.0b013e3182413f6b. PMID: 22421845.
Article28. Lee UL, Nam JH, Choi WC, Kim HW, Kim HJ, Choi YJ. 2019; Comparison of lip line cant change after 1-jaw and 2-jaw surgery. J Craniofac Surg. 30:1820–4. DOI: 10.1097/SCS.0000000000005556. PMID: 31033678.
Article29. Wasserstein RL, Lazar NA. 2016; The ASA statement on p-values: context, process, and purpose. Am Stat. 70:129–33. DOI: 10.1080/00031305.2016.1154108.
Article30. Kim MS, Lim SH, Jeong SR, Park JH. 2020; Maxillary molar intrusion and transverse decompensation to enable mandibular single-jaw surgery with rotational setback and transverse shift for a patient with mandibular prognathism and asymmetry. Am J Orthod Dentofacial Orthop. 157:818–31. DOI: 10.1016/j.ajodo.2019.02.022. PMID: 32487312.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A comparative study of soft tissue changes with mandibular one jaw surgery and double jaw surgery in Class III malocclusion
- Factors affecting postsurgical stability in skeletal Class III malocclusion patients
- A comparative study on the degree of relapse following one jaw surgery and two jaw surgery in skeletal Class III patients
- Soft Tissue Changes after Jaw Surgery in Class III Malocclusion Patients
- A Comparison of pre and post-surgical characteristics in skeletal Class III malocclusion patients using counterpart analysis