J Korean Med Sci.
2022 Jan;37(3):e22. 10.3346/jkms.2022.37.e22.
Health and Mortality in Korean Healthcare Workers
- Affiliations
-
- 1Advanced Biomedical Research Institute, Ewha Womans University Seoul Hospital, Seoul, Korea
- 2College of Nursing, Ewha Womans University, Seoul, Korea
- 3Department of Preventive Medicine, College of Medicine, Ewha Womans University, Seoul, Korea
- 4Graduate Program in System Health Science and Engineering, Ewha Womans University, Seoul, Korea
- 5Clinical Trial Center, Mokdong Hospital, Ewha Womans University, Seoul, Korea
- 6Department of Preventive Medicine, Korea University College of Medicine, Seoul, Korea
- 7National Academy of Medicine of Korea (NAMOK)
- KMID: 2524891
- DOI: http://doi.org/10.3346/jkms.2022.37.e22
Abstract
- Background
To evaluate the health status of healthcare workers (doctors and nurses) compared to those in the general population based on the National Health Insurance Service database and the cause of death data from Statistics Korea.
Methods
The subjects of this study were 104,484 doctors and 220,310 nurses working in healthcare facilities from 2002 to 2017, and who had undergone at least one general medical examination. Based on the subject definition, the subject data were extracted from the National Health Insurance healthcare facility database and qualification database. We collected medical use details included in the research database, general medical examination results, medical history included in the health examination database, and additional data on the cause of death from the National Statistics database to analyze the main cause of death and mortality.
Results
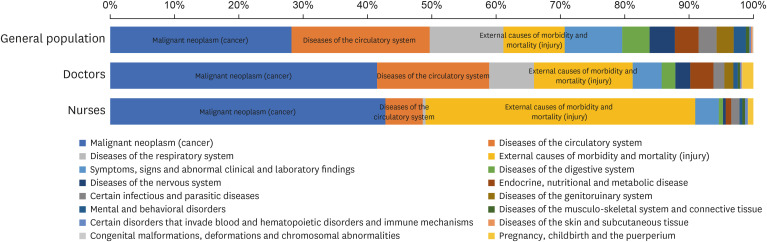
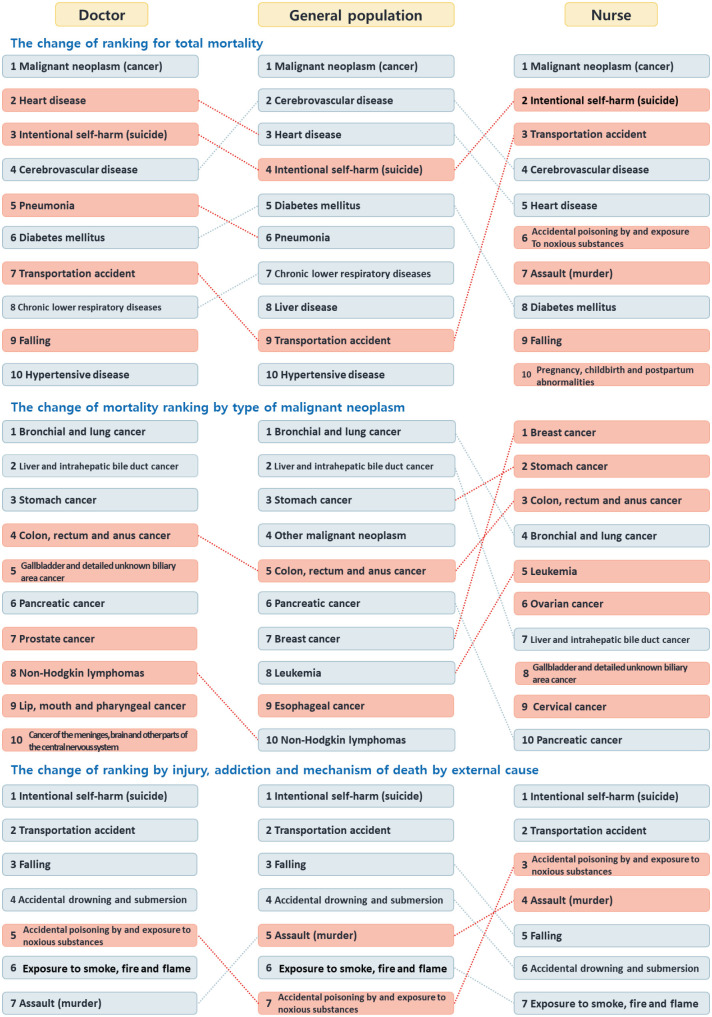
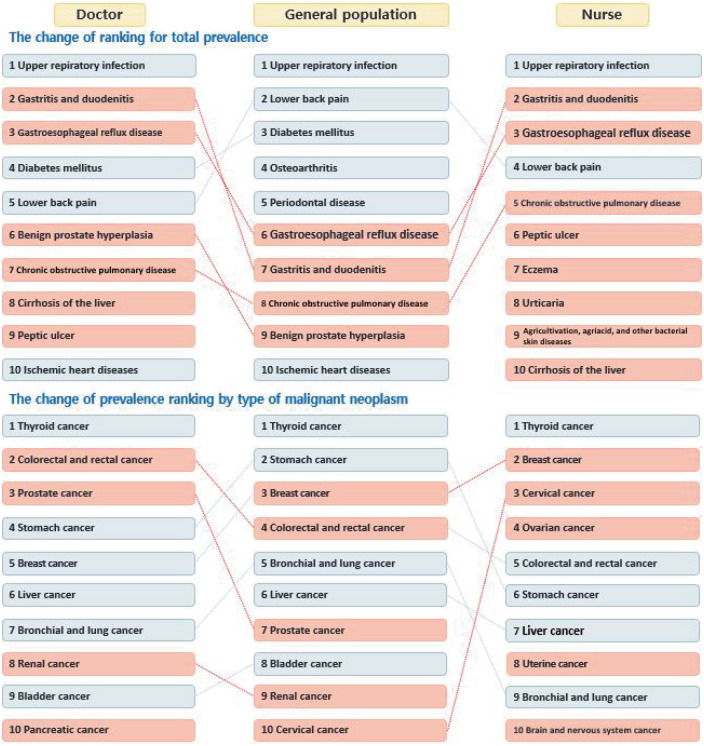
In terms of the major causes of death and mortality among healthcare workers, the mortality rate associated with intentional self-harm, injury, transportation accident, heart disease, addiction, and falling was significantly higher than that in the general population. Further, the prevalence of respiratory and gastrointestinal diseases was high. When analyzing the proportional mortality ratio (PMR) by cause of death for healthcare workers, the PMR values for death related to malignant neoplasm was the highest. In terms of diseases, both doctors and nurses had higher rates of infectious diseases such as maternal sepsis, rubella, and measles.
Conclusion
The health status of healthcare workers differs from that of the general population. Thus, it is important to consider the occupational characteristics of healthcare personnel. This study is unique in that it was conducted based on medical use indicators rather than survey data.
Keyword
Figure
Reference
-
1. Amanullah S, Ramesh Shankar R. The impact of COVID-19 on physician burnout globally: a review. Healthcare (Basel). 2020; 8(4):421.
Article2. Long D, Long D, Turner W, Lambert CC, Creger T, Mugavero MJ, et al. LB-13. Economic and workload impact of COVID-19 pandemic on physicians in the United States: results of a national survey. Open Forum Infect Dis. 2020; 7(Suppl 1):S850.
Article3. Rotenstein LS, Torre M, Ramos MA, Rosales RC, Guille C, Sen S, et al. Prevalence of burnout among physicians: a systematic review. JAMA. 2018; 320(11):1131–1150. PMID: 30326495.4. Salvagioni DAJ, Melanda FN, Mesas AE, González AD, Gabani FL, Andrade SM. Physical, psychological and occupational consequences of job burnout: a systematic review of prospective studies. PLoS One. 2017; 12(10):e0185781. PMID: 28977041.
Article5. Woo T, Ho R, Tang A, Tam W. Global prevalence of burnout symptoms among nurses: a systematic review and meta-analysis. J Psychiatr Res. 2020; 123:9–20. PMID: 32007680.
Article6. Frank E, Biola H, Burnett CA. Mortality rates and causes among U.S. physicians. Am J Prev Med. 2000; 19(3):155–159. PMID: 11020591.
Article7. Chen YT, Huang CC, Weng SF, Hsu CC, Wang JJ, Lin HJ, et al. Acute myocardial infarction: a comparison of the risk between physicians and the general population. BioMed Res Int. 2015; 2015:904328. PMID: 25802869.
Article8. McFadden T, Simon C, Kobeissi B, Gerin-Lajoie C. Physicians' access to primary care: results from the Canadian Medical Association National Physician Health Survey. Can J Ophthalmol. 2020; 55(3):Suppl 1. 27–28. PMID: 32386785.
Article9. Cvejic E, Parker G, Harvey SB, Steel Z, Hadzi-Pavlovic D, Macnamara CL, et al. The health and well-being of Australia's future medical doctors: protocol for a 5-year observational cohort study of medical trainees. BMJ Open. 2017; 7(9):e016837.
Article10. Tam HP, Lin HJ, Weng SF, Hsu CC, Wang JJ, Su SB, et al. The risk of stroke in physicians: a population-based cohort study in Taiwan. Epidemiology. 2017; 28(Suppl 1):S48–S53. PMID: 29028675.11. Shin YC, Kang JH, Kim CH. Mortality among medical doctors based on the registered cause of death in Korea 1992–2002. J Prev Med Public Health. 2005; 38(1):38–44. PMID: 16312908.12. Yoon JH, Lee KH, Hahn KY, Chang SJ, Cha BS, Min SH, et al. Suicide trend of standardized mortality ratio and age standardized proportion mortality ratio according to occupational groups in Korea: 1993–2007. Korean J Occup Environ Med. 2011; 23(2):173–182.13. Kim HL, Park HJ, Sim YH, Choi EY, Shim KW, Lee SW, et al. Cancer prevalence among physicians in Korea: a single center study. Korean J Fam Med. 2016; 37(2):91–96. PMID: 27073607.
Article14. Yoon J, Lee K, Hahn K, Chang SJ, Cha BS, Min SH, et al. Suicide trend of standardized mortality ratio and age standardized proportion mortality ratio according to occupational groups in Korea: 1993–2007. Korean J Occup Environ Med. 2011; 23(2):173–182.15. Kim YE, Park H, Jo MW, Oh IH, Go DS, Jung J, et al. Trends and patterns of burden of disease and injuries in Korea using disability-adjusted life years. J Korean Med Sci. 2019; 34(Suppl 1):e75. PMID: 30923488.
Article16. Yoon J, Yoon SJ. Quantifying burden of disease to measure population health in Korea. J Korean Med Sci. 2016; 31(Suppl 2):S101–S107. PMID: 27775246.
Article17. Hawton K, Agerbo E, Simkin S, Platt B, Mellanby RJ. Risk of suicide in medical and related occupational groups: a national study based on Danish case population-based registers. J Affect Disord. 2011; 134(1-3):320–326. PMID: 21676470.
Article18. Gagné P, Moamai J, Bourget D. Psychopathology and suicide among Quebec physicians: a nested case control study. Depress Res Treat. 2011; 2011:936327. PMID: 21822488.
Article19. Lin CM, Yang CH, Sung FC, Li CY. Risks and causes of hospitalizations among physicians in Taiwan. Health Serv Res. 2008; 43(2):675–692. PMID: 18370973.
Article20. Lee YS, Hsu CC, Weng SF, Lin HJ, Wang JJ, Su SB, et al. Cancer incidence in physicians: a Taiwan national population-based cohort study. Medicine (Baltimore). 2015; 94(47):e2079. PMID: 26632715.21. Kao LT, Chiu YL, Lin HC, Lee HC, Chung SD. Prevalence of chronic diseases among physicians in Taiwan: a population-based cross-sectional study. BMJ Open. 2016; 6(3):e009954.
Article22. Kuo WY, Huang CC, Weng SF, Lin HJ, Su SB, Wang JJ, et al. Higher migraine risk in healthcare professionals than in general population: a nationwide population-based cohort study in Taiwan. J Headache Pain. 2015; 16(1):102. PMID: 26631235.
Article23. Vaz K, McGrowder D, Crawford T, Alexander-Lindo RL, Irving R. Prevalence of injuries and reporting of accidents among health care workers at the University Hospital of the West Indies. Int J Occup Med Environ Health. 2010; 23(2):133–143. PMID: 20630834.
Article24. Prüss-Ustün A, Rapiti E, Hutin Y. Estimation of the global burden of disease attributable to contaminated sharps injuries among health-care workers. Am J Ind Med. 2005; 48(6):482–490. PMID: 16299710.25. The Physicians Foundation. 2018 Survey of America's Physicians: Practice Patterns & Perspectives. Boston, MA, USA: The Physicians Foundation;2018.26. Lin LY, Warren-Gash C, Smeeth L, Chen PC. Data resource profile: the national health insurance research database (NHIRD). Epidemiol Health. 2018; 40:e2018062. PMID: 30727703.
Article27. Hsieh CY, Su CC, Shao SC, Sung SF, Lin SJ, Kao Yang YH, et al. Taiwan's national health insurance research database: past and future. Clin Epidemiol. 2019; 11:349–358. PMID: 31118821.28. Lee JC. 2016 National medical survey. Med Policy Forum. 2018; 16(1):64–69.29. Kim O, Ahn Y, Lee HY, Jang HJ, Kim S, Lee JE, et al. The Korea Nurses' health study: a prospective cohort study. J Womens Health (Larchmt). 2017; 26(8):892–899. PMID: 28771383.
Article30. Chan LJ. With the importance of the national survey of physicians (KPS). Med Policy Forum. 2020; 18(2):62–66.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- COVID-19 and MERS Infections in Healthcare Workers in Korea
- Interventions on Well-being, Occupational Health, and Aging of Healthcare Workers: A Scoping Review of Systematic Reviews
- nalysis of Case Characteristics of Occupational Diseases and Epidemiological Investigation of Healthcare Workers
- Hepatitis B vaccination coverage and the determinants of vaccination among health care workers in selected health facilities in Lusaka district, Zambia: an exploratory study
- Occupational inequalities in mortality in Korea: an analysis using nationally representative mortality follow-up data from the late 2000s and after