Cancer Res Treat.
2022 Jan;54(1):245-252. 10.4143/crt.2021.023.
Effect of Waiting Time from Pathological Diagnosis to Definitive Concurrent Chemoradiation for Cervical Cancer on Overall Survival
- Affiliations
-
- 1Division of Gynecologic Oncology, Department of Obstetrics and Gynecology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 2Department of Radiation Oncology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2524605
- DOI: http://doi.org/10.4143/crt.2021.023
Abstract
- Purpose
This study aimed to evaluate the effect of waiting time, from diagnosis to initiation of definitive concurrent chemoradiation (CCRT), on overall survival in cervical cancer patients.
Materials and Methods
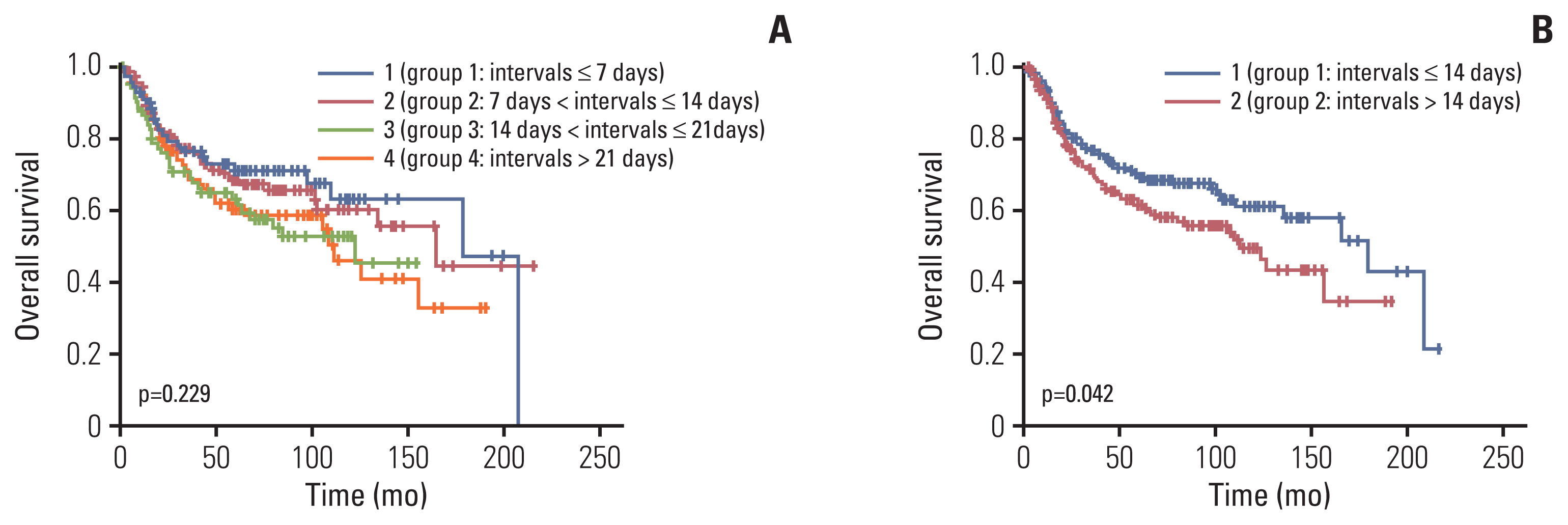
Patients with cervical cancer who were treated with definitive CCRT between 2000 and 2017 were retrospectively reviewed. Time from initial pathological diagnosis to definitive CCRT was analyzed both as a continuous variable (per day) and as a categorical variable in two groups (group 1 ≤ median, group 2 > median). Patients with a waiting time of more than 60 days were excluded.
Results
The median waiting time was 14 days (0-60). There were differences between group 1 and group 2 in age and chemotherapy regimens. However, no significant difference was found in the International Federation of Gynecology and Obstetrics stage, cell type, or the number of cycles of chemotherapy received during CCRT. A longer waiting time was associated with poorer overall survival on the Kaplan-Meier curve (group 1 vs. group 2, p=0.042). On multivariate analysis, intervals as either a continuous variable (hazard ratio [HR], 1.023; 95% confidence interval [CI], 1.006 to 1.040; p=0.007) or a categorical variable (HR, 1.513; 95% CI, 1.073 to 2.134; p=0.018), FIGO stage, cell type, and the number of cycles of chemotherapy received during CCRT were significant independent prognostic factors for overall survival.
Conclusion
A shorter waiting time from pathological diagnosis to definitive CCRT showed benefit on overall survival. Our findings suggest that an effort to minimize waiting times should be recommended in cervical cancer patients who are candidates for CCRT.
Keyword
Figure
Reference
-
References
1. Arbyn M, Weiderpass E, Bruni L, de Sanjose S, Saraiya M, Ferlay J, et al. Estimates of incidence and mortality of cervical cancer in 2018: a worldwide analysis. Lancet Glob Health. 2020; 8:e191–203.
Article2. Keys HM, Bundy BN, Stehman FB, Muderspach LI, Chafe WE, Suggs CL 3rd, et al. Cisplatin, radiation, and adjuvant hysterectomy compared with radiation and adjuvant hysterectomy for bulky stage IB cervical carcinoma. N Engl J Med. 1999; 340:1154–61.
Article3. Peters WA 3rd, Liu PY, Barrett RJ 2nd, Stock RJ, Monk BJ, Berek JS, et al. Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. J Clin Oncol. 2000; 18:1606–13.
Article4. Whitney CW, Sause W, Bundy BN, Malfetano JH, Hannigan EV, Fowler WC Jr, et al. Randomized comparison of fluorouracil plus cisplatin versus hydroxyurea as an adjunct to radiation therapy in stage IIB–IVA carcinoma of the cervix with negative para-aortic lymph nodes: a Gynecologic Oncology Group and Southwest Oncology Group study. J Clin Oncol. 1999; 17:1339–48.
Article5. Morris M, Eifel PJ, Lu J, Grigsby PW, Levenback C, Stevens RE, et al. Pelvic radiation with concurrent chemotherapy compared with pelvic and para-aortic radiation for high-risk cervical cancer. N Engl J Med. 1999; 340:1137–43.
Article6. Rose PG, Bundy BN, Watkins EB, Thigpen JT, Deppe G, Maiman MA, et al. Concurrent cisplatin-based radiotherapy and chemotherapy for locally advanced cervical cancer. N Engl J Med. 1999; 340:1144–53.
Article7. Wyatt RM, Jones BJ, Dale RG. Radiotherapy treatment delays and their influence on tumour control achieved by various fractionation schedules. Br J Radiol. 2008; 81:549–63.
Article8. Mackillop WJ, Zhou Y, Quirt CF. A comparison of delays in the treatment of cancer with radiation in Canada and the United States. Int J Radiat Oncol Biol Phys. 1995; 32:531–9.
Article9. Ferreira da Silva I, Ferreira da Silva I, Koifman RJ. Cervical cancer treatment delays and associated factors in a cohort of women from a developing country. J Glob Oncol. 2019; 5:1–11.
Article10. Umezu T, Shibata K, Kajiyama H, Yamamoto E, Mizuno M, Kikkawa F. Prognostic factors in stage IA–IIA cervical cancer patients treated surgically: does the waiting time to the operation affect survival? Arch Gynecol Obstet. 2012; 285:493–7.
Article11. Choan E, Dahrouge S, Samant R, Mirzaei A, Price J. Radical radiotherapy for cervix cancer: the effect of waiting time on outcome. Int J Radiat Oncol Biol Phys. 2005; 61:1071–7.12. Benard VB, Howe W, Royalty J, Helsel W, Kammerer W, Richardson LC. Timeliness of cervical cancer diagnosis and initiation of treatment in the National Breast and Cervical Cancer Early Detection Program. J Womens Health (Larchmt). 2012; 21:776–82.
Article13. Choi CH, Ryu JY, Cho YJ, Jeon HK, Choi JJ, Ylaya K, et al. The anti-cancer effects of itraconazole in epithelial ovarian cancer. Sci Rep. 2017; 7:6552.
Article14. Croke J, Fyles A, Barbera L, D’Souza D, Pearcey R, Stuckless T, et al. Radiation therapy quality-of-care indicators for locally advanced cervical cancer: a consensus guideline. Pract Radiat Oncol. 2016; 6:315–23.
Article15. Cionini L, Gardani G, Gabriele P, Magri S, Morosini PL, Rosi A, et al. Quality indicators in radiotherapy. Radiother Oncol. 2007; 82:191–200.
Article16. Nascimento MI, Silva GA. Waiting time for radiotherapy in women with cervical cancer. Rev Saude Publica. 2015; 49:92.
Article17. Lee YY, Park W, Huh SJ, Yoon A, Park JY, Choi CH, et al. Platinum-based combination chemotherapy vs. weekly cisplatin during adjuvant CCRT in early cervical cancer with pelvic LN metastasis. Anticancer Res. 2013; 33:4675–81.18. Perri T, Issakov G, Ben-Baruch G, Felder S, Beiner ME, Helpman L, et al. Effect of treatment delay on survival in patients with cervical cancer: a historical cohort study. Int J Gynecol Cancer. 2014; 24:1326–32.
Article19. Nanthamongkolkul K, Hanprasertpong J. Longer waiting times for early stage cervical cancer patients undergoing radical hysterectomy are associated with diminished long-term overall survival. J Gynecol Oncol. 2015; 26:262–9.
Article20. Chen CP, Kung PT, Wang YH, Tsai WC. Effect of time interval from diagnosis to treatment for cervical cancer on survival: a nationwide cohort study. PLoS One. 2019; 14:e0221946.
Article21. Paik ES, Shim M, Choi HJ, Lee YY, Kim TJ, Lee JW, et al. Impact of lymphadenectomy on survival after recurrence in patients with advanced ovarian cancer without suspected lymph node metastasis. Gynecol Oncol. 2016; 143:252–7.
Article22. Capelle L, Stevens W, Brooks S. Management pathway for patients with cervical cancer in the Auckland region 2003–2007. J Med Imaging Radiat Oncol. 2011; 55:337–43.
Article23. Shen SC, Hung YC, Kung PT, Yang WH, Wang YH, Tsai WC. Factors involved in the delay of treatment initiation for cervical cancer patients: a nationwide population-based study. Medicine (Baltimore). 2016; 95:e4568.24. Strohl AE, Feinglass JM, Shahabi S, Simon MA. Surgical wait time: a new health indicator in women with endometrial cancer. Gynecol Oncol. 2016; 141:511–5.
Article25. Elit LM, O’Leary EM, Pond GR, Seow HY. Impact of wait times on survival for women with uterine cancer. J Clin Oncol. 2014; 32:27–33.
Article26. Gyenwali D, Khanal G, Paudel R, Amatya A, Pariyar J, Onta SR. Estimates of delays in diagnosis of cervical cancer in Nepal. BMC Womens Health. 2014; 14:29.
Article27. Allgar VL, Neal RD. Delays in the diagnosis of six cancers: analysis of data from the National Survey of NHS Patients: cancer. Br J Cancer. 2005; 92:1959–70.
Article28. Hansen RP, Olesen F, Sorensen HT, Sokolowski I, Sondergaard J. Socioeconomic patient characteristics predict delay in cancer diagnosis: a Danish cohort study. BMC Health Serv Res. 2008; 8:49.
Article29. Ma S, Wang J, Han Y, Guo F, Chen C, Chen X, et al. Platinum single-agent vs. platinum-based doublet agent concurrent chemoradiotherapy for locally advanced cervical cancer: a meta-analysis of randomized controlled trials. Gynecol Oncol. 2019; 154:246–52.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Impact of hematologic toxicities during concurrent chemoradiation for cervical cancer
- Clinicopathologic Characteristics of Anal Cancer
- Long-Term Outcomes of Chemoradiation for Anal Cancer Patients
- Longer waiting times for early stage cervical cancer patients undergoing radical hysterectomy are associated with diminished long-term overall survival
- Patterns of definitive radiotherapy practice for cervical cancer in South Korea: a survey endorsed by the Korean Radiation Oncology Group (KROG 20-06)