Cancer Res Treat.
2022 Jan;54(1):130-139. 10.4143/crt.2020.1106.
Occupational Exposure to Pesticides and Lung Cancer Risk: A Propensity Score Analyses
- Affiliations
-
- 1Division of Cancer Prevention and Early Detection, National Cancer Control Institute, National Cancer Center, Goyang, Korea
- 2Graduate School of Cancer Science and Policy and Division of Cancer Prevention, National Cancer Center, Goyang, Korea
- KMID: 2524594
- DOI: http://doi.org/10.4143/crt.2020.1106
Abstract
- Purpose
Occupational exposure to pesticides is thought to be associated with lung cancer, but studies have yielded conflicting results. We performed a propensity score (PS) based analyses to evaluate the relationship between occupational exposure to pesticides and lung cancer risk in the Korea National Cancer Center community-based cohort study (KNCCCS).
Materials and Methods
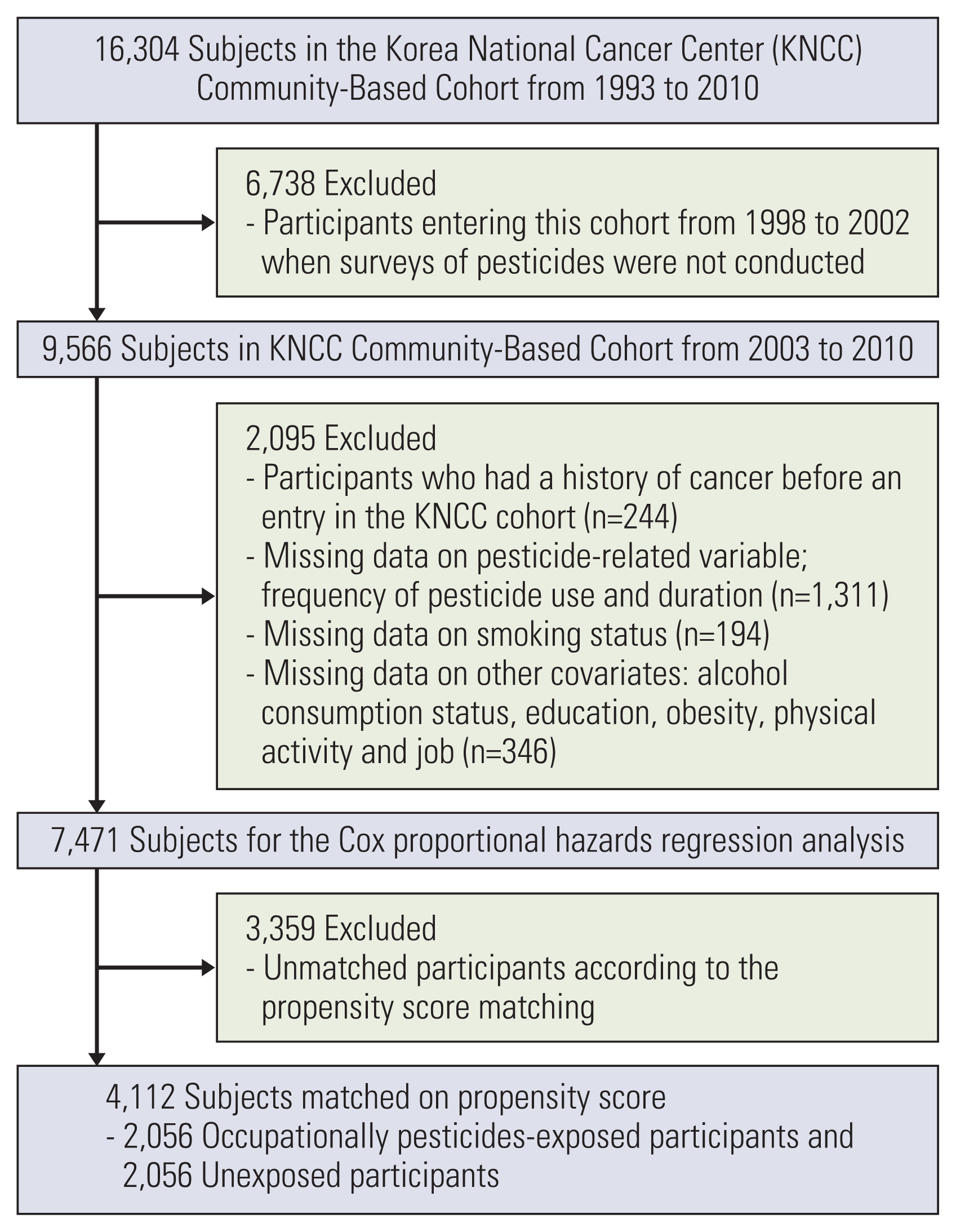
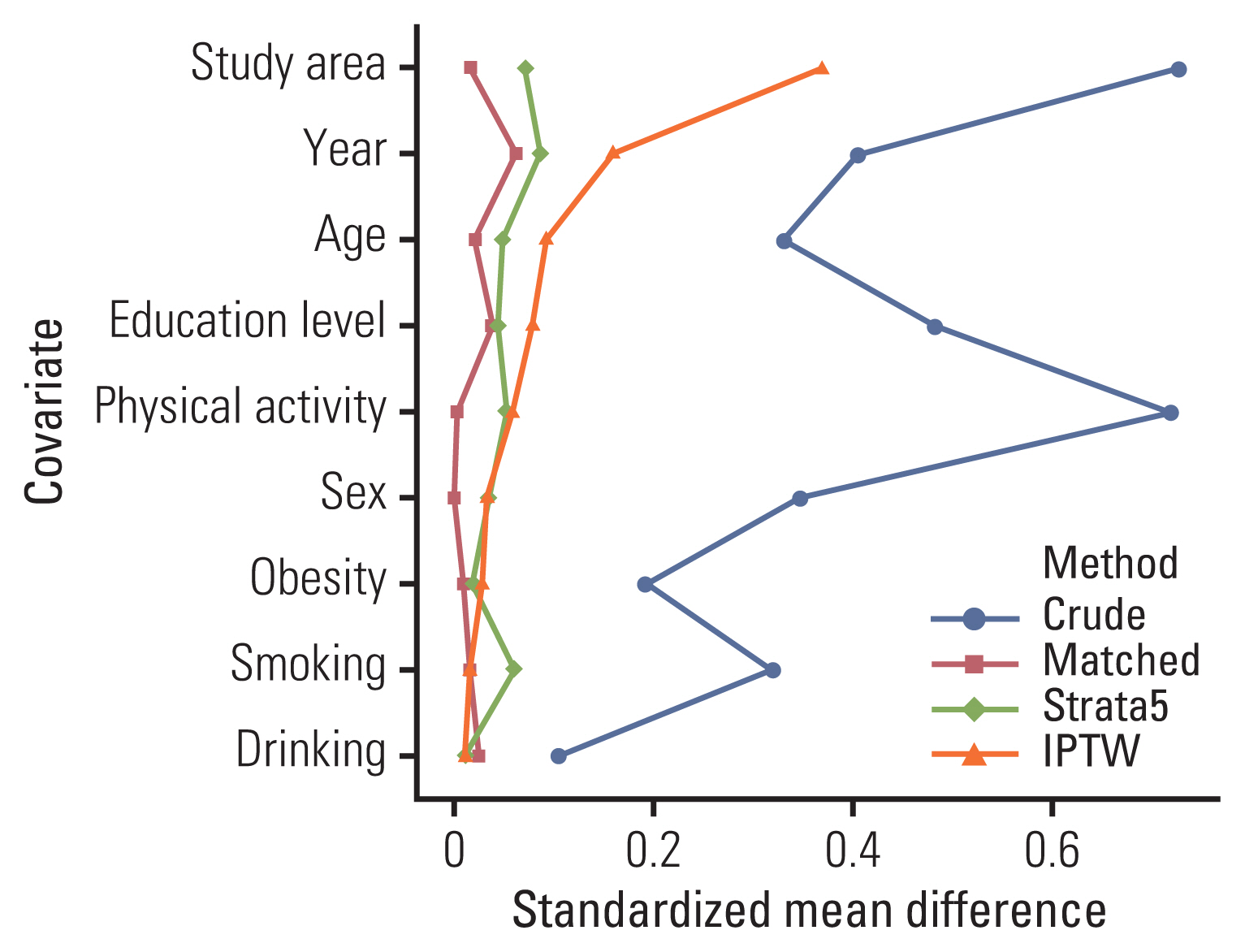
During the follow-up period, 123 incidental lung cancer cases were identified, of the 7,471 subjects in the final statistical analysis. Information about occupational exposure to pesticides and other factors was collected at enrollment (2003-2010). Cox proportional hazards regression analyses were conducted. Four PS-based approaches (i.e., matching, stratification, inverse probability-of-treatment weighting, and the use of the PS as a covariate) were adopted, and the results were compared. PS was obtained from the logistic regression model. Absolute standardized differences according to occupational exposure to pesticides were provided to evaluate the balance in baseline characteristics.
Results
In the Cox proportional hazards regression model, the hazard ratio (HR) for lung cancer according to occupational exposure to pesticides was 1.82 (95% confidence interval [CI], 1.11 to 2.98). With all the propensity score matching (PSM) methods, the HRs for lung cancer based on exposure to pesticides ranged from 1.65 (95% CI, 1.04 to 2.64) (continuous term with PSM) to 2.84 (95% CI, 1.81 to 4.46) (stratification by 5 strata of the PS). The results varied slightly based on the method used, but the direction and statistical significance remained the same.
Conclusion
Our results strengthen the evidence for an association between occupational exposure to pesticides and the risk of lung cancer.
Keyword
Figure
Reference
-
References
1. van der Plaat DA, de Jong K, de Vries M, van Diemen CC, Nedeljkovic I, Amin N, et al. Occupational exposure to pesticides is associated with differential DNA methylation. Occup Environ Med. 2018; 75:427–35.
Article2. Statistics Korea. Annual report on the cause of death statistics. Daejeon: Statistics Korea;2016.3. World Health Organization. WHO handbook on indoor radon: a public health perspective. Geneva: World Health Organization;2009.4. Barthel E. Increased risk of lung cancer in pesticide-exposed male agricultural workers. J Toxicol Environ Health. 1981; 8:1027–40.
Article5. Becher H, Flesch-Janys D, Kauppinen T, Kogevinas M, Steindorf K, Manz A, et al. Cancer mortality in German male workers exposed to phenoxy herbicides and dioxins. Cancer Causes Control. 1996; 7:312–21.
Article6. Blair A, Dosemeci M, Heineman EF. Cancer and other causes of death among male and female farmers from twenty-three states. Am J Ind Med. 1993; 23:729–42.
Article7. MacMahon B, Monson RR, Wang HH, Zheng TZ. A second follow-up of mortality in a cohort of pesticide applicators. J Occup Med. 1988; 30:429–32.
Article8. Pesatori AC, Sontag JM, Lubin JH, Consonni D, Blair A. Cohort mortality and nested case-control study of lung cancer among structural pest control workers in Florida (United States). Cancer Causes Control. 1994; 5:310–8.
Article9. Bonner MR, Freeman LE, Hoppin JA, Koutros S, Sandler DP, Lynch CF, et al. Occupational exposure to pesticides and the incidence of lung cancer in the agricultural health study. Environ Health Perspect. 2017; 125:544–51.
Article10. Alavanja MC, Dosemeci M, Samanic C, Lubin J, Lynch CF, Knott C, et al. Pesticides and lung cancer risk in the agricultural health study cohort. Am J Epidemiol. 2004; 160:876–85.
Article11. Boulanger M, Tual S, Lemarchand C, Guizard AV, Delafosse P, Marcotullio E, et al. Lung cancer risk and occupational exposures in crop farming: results from the AGRIculture and CANcer (AGRICAN) cohort. Occup Environ Med. 2018; 75:776–85.
Article12. Jones RR, Barone-Adesi F, Koutros S, Lerro CC, Blair A, Lubin J, et al. Incidence of solid tumours among pesticide applicators exposed to the organophosphate insecticide diazinon in the Agricultural Health Study: an updated analysis. Occup Environ Med. 2015; 72:496–503.
Article13. Silver SR, Bertke SJ, Hines CJ, Alavanja MC, Hoppin JA, Lubin JH, et al. Cancer incidence and metolachlor use in the Agricultural Health Study: an update. Int J Cancer. 2015; 137:2630–43.
Article14. US Environmental Protection Agency. Office of pesticide programs: list of chemicals evaluated for carcinogenic potential. Washington, DC: Environmental Protection Agency;2002.15. Elze MC, Gregson J, Baber U, Williamson E, Sartori S, Mehran R, et al. Comparison of propensity score methods and covariate adjustment: evaluation in 4 cardiovascular studies. J Am Coll Cardiol. 2017; 69:345–57.16. Heinze G, Juni P. An overview of the objectives of and the approaches to propensity score analyses. Eur Heart J. 2011; 32:1704–8.
Article17. Oh JK, Lim MK, Yun EH, Choi MH, Hong ST, Chang SH, et al. Cohort profile: community-based prospective cohort from the National Cancer Center, Korea. Int J Epidemiol. 2017; 46:e14.
Article18. Shin HR, Won YJ, Jung KW, Kong HJ, Yim SH, Lee JK, et al. Nationwide cancer incidence in Korea, 1999–2001: first result using the national cancer incidence database. Cancer Res Treat. 2005; 37:325–31.
Article19. Riaz SP, Horton M, Kang J, Mak V, Luchtenborg M, Moller H. Lung cancer incidence and survival in England: an analysis by socioeconomic deprivation and urbanization. J Thorac Oncol. 2011; 6:2005–10.
Article20. Yoshida K, Bartel A, Chipman JJ, Bohn J, McGowan LD, Barrett M, et al. Create ‘Table 1’ to describe baseline characteristics with or without propensity score weights [Internet]. Vienna: The Comprehensive R Archive Network;2020. [cited 2018 Apr 4]. Available from: https://cran.r-project.org/web/packages/tableone/tableone.pdf .21. Christensen CH, Platz EA, Andreotti G, Blair A, Hoppin JA, Koutros S, et al. Coumaphos exposure and incident cancer among male participants in the Agricultural Health Study (AHS). Environ Health Perspect. 2010; 118:92–6.
Article22. Freeman LE, Rusiecki JA, Hoppin JA, Lubin JH, Koutros S, Andreotti G, et al. Atrazine and cancer incidence among pesticide applicators in the agricultural health study (1994–2007). Environ Health Perspect. 2011; 119:1253–9.
Article23. Kang D, Park SK, Beane-Freeman L, Lynch CF, Knott CE, Sandler DP, et al. Cancer incidence among pesticide applicators exposed to trifluralin in the Agricultural Health Study. Environ Res. 2008; 107:271–6.
Article24. Greenburg DL, Rusiecki J, Koutros S, Dosemeci M, Patel R, Hines CJ, et al. Cancer incidence among pesticide applicators exposed to captan in the Agricultural Health Study. Cancer Causes Control. 2008; 19:1401–7.
Article25. Lynch SM, Mahajan R, Beane Freeman LE, Hoppin JA, Alavanja MC. Cancer incidence among pesticide applicators exposed to butylate in the Agricultural Health Study (AHS). Environ Res. 2009; 109:860–8.
Article26. Mahajan R, Blair A, Lynch CF, Schroeder P, Hoppin JA, Sandler DP, et al. Fonofos exposure and cancer incidence in the agricultural health study. Environ Health Perspect. 2006; 114:1838–42.
Article27. Rusiecki JA, Patel R, Koutros S, Beane-Freeman L, Landgren O, Bonner MR, et al. Cancer incidence among pesticide applicators exposed to permethrin in the Agricultural Health Study. Environ Health Perspect. 2009; 117:581–6.
Article28. Enomoto M, Tierney WJ, Nozaki K. Risk of human health by particulate matter as a source of air pollution: comparison with tobacco smoking. J Toxicol Sci. 2008; 33:251–67.
Article29. Samet JM, Eradze GR. Radon and lung cancer risk: taking stock at the millenium. Environ Health Perspect. 2000; 108(Suppl 4):635–41.
Article30. Yang P. Lung cancer in never smokers. Semin Respir Crit Care Med. 2011; 32:10–21.
Article31. Brennan P, Hainaut P, Boffetta P. Genetics of lung-cancer susceptibility. Lancet Oncol. 2011; 12:399–408.
Article32. Kogevinas M, Becher H, Benn T, Bertazzi PA, Boffetta P, Bueno-de-Mesquita HB, et al. Cancer mortality in workers exposed to phenoxy herbicides, chlorophenols, and dioxins. An expanded and updated international cohort study. Am J Epidemiol. 1997; 145:1061–75.
Article33. Walker NJ, Crockett PW, Nyska A, Brix AE, Jokinen MP, Sells DM, et al. Dose-additive carcinogenicity of a defined mixture of “dioxin-like compounds”. Environ Health Perspect. 2005; 113:43–8.
Article34. Boffetta P, Mundt KA, Adami HO, Cole P, Mandel JS. TCDD and cancer: a critical review of epidemiologic studies. Crit Rev Toxicol. 2011; 41:622–36.
Article35. Ojha A, Srivastava N. In vitro studies on organophosphate pesticides induced oxidative DNA damage in rat lymphocytes. Mutat Res Genet Toxicol Environ Mutagen. 2014; 761:10–7.
Article36. Zafiropoulos A, Tsarouhas K, Tsitsimpikou C, Fragkiadaki P, Germanakis I, Tsardi M, et al. Cardiotoxicity in rabbits after a low-level exposure to diazinon, propoxur, and chlorpyrifos. Hum Exp Toxicol. 2014; 33:1241–52.
Article37. Mladinic M, Zeljezic D, Shaposhnikov SA, Collins AR. The use of FISH-comet to detect c-Myc and TP 53 damage in extended-term lymphocyte cultures treated with terbuthylazine and carbofuran. Toxicol Lett. 2012; 211:62–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Parkinson's disease in a worker exposed to insecticides at a greenhouse
- Occupational Risk Factors for Prostate Cancer: A Meta-analysis
- Dermal Exposure Associated with Occupational End Use of Pesticides and the Role of Protective Measures
- Radon exposure and lung cancer: risk in nonsmokers among cohort studies
- Occupational factors affecting the decline in pulmonary function among male farmers using occupational pesticide in Gyeonggi-do, South Korea