Child Kidney Dis.
2021 Dec;25(2):112-116. 10.3339/jkspn.2021.25.2.112.
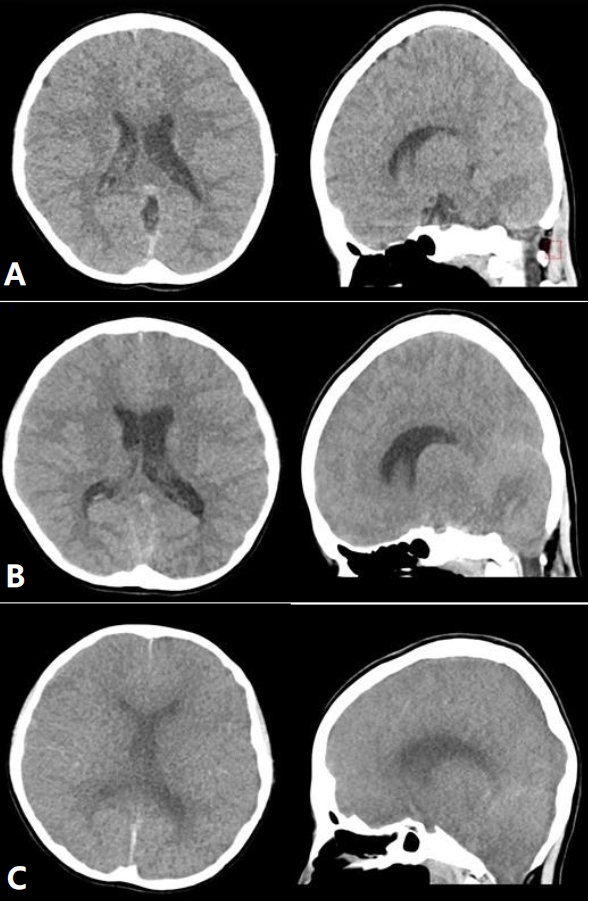
A Case of Severe Hyperammonemic Encephalopathy Caused by Urinary Tract Infection in Obstructive Uropathy
- Affiliations
-
- 1Department of Pediatrics, Asan Medical Center Children’s Hospital, University of Ulsan College of Medicine, Seoul, Republic of Korea
- KMID: 2524512
- DOI: http://doi.org/10.3339/jkspn.2021.25.2.112
Abstract
- Hyperammonemia is mainly caused by diseases related to liver failure. However, there are also non-hepatic causes of hyperammonemia, such as urinary tract infection (UTI) due to urease-producing organisms. Urease production by these bacteria induces a hydrolysis of urinary urea into ammonia that can cross the urothelial cell membrane and diffuse into blood vessels, leading to hyperammonemia. Delayed diagnosis and treatment of hyperammonemia can lead to lethal encephalopathy that can cause brain damage and life-threatening conditions. In the presence of obstructive uropathy, UTI by urease-producing bacteria can lead to more severe hyperammonemia due to enhanced resorption of ammonia into the systemic circulation. In this report, we present a case of acute severe hyperammonemic encephalopathy leading to brain death due to accumulation of ammonia in blood caused by Morganella morganii UTI in a 10-year-old girl with cloacal anomaly, causing obstructive uropathy even after multiple corrections.
Keyword
Figure
Reference
-
References
1. Burton BK. Urea cycle disorders. Clin Liver Dis. 2000; 4:815–30.
Article2. Savy N, Brossier D, Brunel-Guitton C, Ducharme-Crevier L, Du Pont-Thibodeau G, Jouvet P. Acute pediatric hyperammonemia: current diagnosis and management strategies. Hepatic Med Evid Res. 2018; 10:105–15.
Article3. Kaveggia FF, Thompson JS, Schafer EC, Fischer JL, Taylor RJ. Hyperammonemic encephalopathy in urinary diversion with urea-splitting urinary tract infection. Arch Intern Med. 1990; 150:2389–92.
Article4. Warne S, Chitty LS, Wilcox DT. Prenatal diagnosis of cloacal anomalies. BJU Int. 2002; 89:78–81.
Article5. Ozanne B, Nelson J, Cousineau J, Lambert M, Phan V, Mitchell G, et al. Threshold for toxicity from hyperammonemia in critically ill children. J Hepatol. 2012; 56:123–8.
Article6. Siemienski J. Role of bacterial urease in experimental pyelonephritis. J Bacteriol. 1960; 80:171–9.
Article7. Kiyokawa H, Igawa Y, Nishizawa O. Hyperammonaemic encephalopathy associated with retention of urine in multiple large diverticula. BJU Int. 2001; 88:122–3.
Article8. Goda T, Watanabe K, Kobayashi J, Nagai Y, Ohara N, Takahashi D. A case of hyperammonemia with obstructive urinary tract infection by urease-producing bacteria. Rinsho Shinkeigaku (Clin Neurol). 2017; 57:130–3.
Article9. Emura M, Tsuchihashi K, Shimizu Y, Kanamaru S, Matoba S, Ito N. A Case of Hyperammonemia Caused by Urinary Tract Infection Due to Urease-Producing Bacteria. Hinyokika Kiyo. Acta Urologica Japonica. 2016; 62:421–5.10. McEwan P, Simpson D, Kirk JM, Barr DG, McKenzie KJ. Short report: Hyperammonaemia in critically ill septic infants. Arch Dis Child. 2001; 84:512–3.11. Sinha B, Gonzalez R. Hyperammonemia in a boy with obstructive ureterocele and proteus infection. J Urol. 1984; 131:330–1.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Urinary-Tract-Infection Induced Noncirrhotic Hyperammonemic Encephalopathy Mimicking Nonconvulsive Status Epilepticus
- Acute Hyperammonemic Encephalopathy with Features on Diffusion-Weighted Images: Report of Two Cases
- Non-cirrhotic Hyperammonemic Encephalopathy with Portosystemic Shunt
- A Case of Obstructive Uropathy Accompanied with Severe Hypernatremia
- Reversible Burst-suppression Pattern of Acute Hyperammonemic Encephalopathy