Acute Crit Care.
2021 Nov;36(4):369-373. 10.4266/acc.2021.00801.
Safety and feasibility of hybrid tracheostomy
- Affiliations
-
- 1Division of Pulmonology, Department of Internal Medicine, Konyang University Hospital, Daejeon, Korea
- 2Department of Thoracic and Cardiovascular Surgery, Konyang University Hospital, Daejeon, Korea
- KMID: 2524320
- DOI: http://doi.org/10.4266/acc.2021.00801
Abstract
- Background
Percutaneous dilatational tracheostomy (PDT) is widely used in intensive care units, but this conventional method has some disadvantages, such as requirement of a lot of equipment and experts at the site. Especially, in situations where the patient is isolated due to an infectious disease, difficulties in using the equipment may occur, and the number of exposed persons may increase. In this paper, we introduce hybrid tracheostomy that combines the advantages of surgical tracheostomy and PDT and describe our experiences.
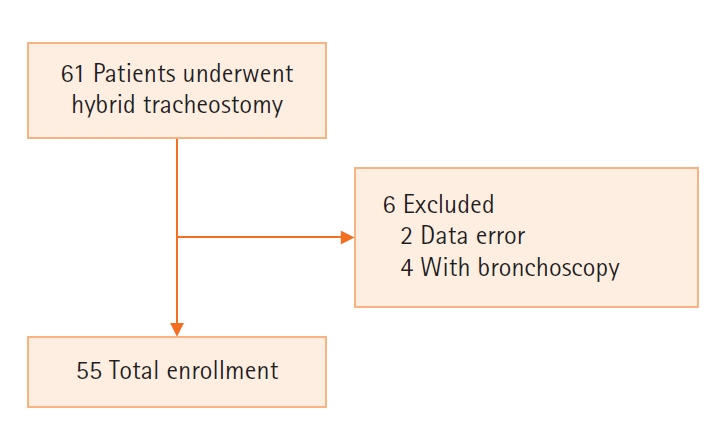
Methods
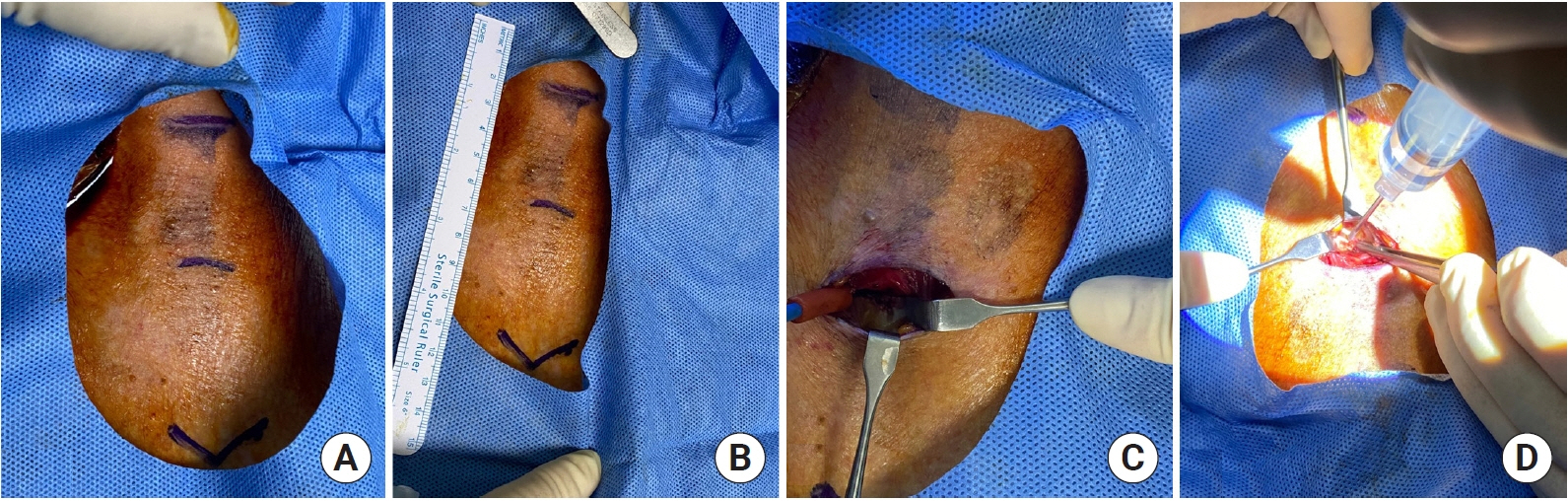
Data from 55 patients who received hybrid tracheostomy without bronchoscopy from January 2020 to February 2021 were collected and reviewed retrospectively. Hybrid tracheostomy was performed at the bedside by a single thoracic surgeon. The hybrid tracheostomy method was as follows: after the skin was incised and the trachea was exposed, only the extent of the endotracheal tube that could not be removed was withdrawn, and then tracheostomy was performed by the Seldinger method using a PDT kit.
Results
The average age was 66.5 years, and the proportion of men was 69.1%. Among the patients, 21.8% were taking antiplatelet drugs and 14.5% were taking anticoagulants. The average duration of the procedure was 13.3 minutes. There was no major bleeding, and there was one case of paratracheal placement of the tracheostomy tube.
Conclusions
In most patients, the procedure can be safely performed without any major complications. However, patients with a short neck, a neck burn or patients who have received radiation therapy to the neck should be treated with conventional methods.
Figure
Reference
-
1. Ciaglia P, Firsching R, Syniec C. Elective percutaneous dilatational tracheostomy: a new simple bedside procedure; preliminary report. Chest. 1985; 87:715–9.2. Iftikhar IH, Teng S, Schimmel M, Duran C, Sardi A, Islam S. A network comparative meta-analysis of percutaneous dilatational tracheostomies using anatomic landmarks, bronchoscopic, and ultrasound guidance versus open surgical tracheostomy. Lung. 2019; 197:267–75.
Article3. Barba CA, Angood PB, Kauder DR, Latenser B, Martin K, McGonigal MD, et al. Bronchoscopic guidance makes percutaneous tracheostomy a safe, cost-effective, and easy-to-teach procedure. Surgery. 1995; 118:879–83.
Article4. Klotz R, Probst P, Deininger M, Klaiber U, Grummich K, Diener MK, et al. Percutaneous versus surgical strategy for tracheostomy: a systematic review and meta-analysis of perioperative and postoperative complications. Langenbecks Arch Surg. 2018; 403:137–49.
Article5. Angel LF, Simpson CB. Comparison of surgical and percutaneous dilational tracheostomy. Clin Chest Med. 2003; 24:423–9.
Article6. Addas BM, Howes WJ, Hung OR. Light-guided tracheal puncture for percutaneous tracheostomy. Can J Anaesth. 2000; 47:919–22.
Article7. Baek JK, Lee JS, Kang M, Choi NJ, Hong SK. Feasibility of percutaneous dilatational tracheostomy with a light source in the surgical intensive care unit. Acute Crit Care. 2018; 33:89–94.
Article8. Freeman BD. Tracheostomy update: when and how. Crit Care Clin. 2017; 33:311–22.9. Dempsey GA, Morton B, Hammell C, Williams LT, Tudur Smith C, Jones T. Long-term outcome following tracheostomy in critical care: a systematic review. Crit Care Med. 2016; 44:617–28.10. Silvester W, Goldsmith D, Uchino S, Bellomo R, Knight S, Seevanayagam S, et al. Percutaneous versus surgical tracheostomy: a randomized controlled study with long-term follow-up. Crit Care Med. 2006; 34:2145–52.
Article11. Freeman BD. Back to the present-does tracheostomy technique affect long-term complications? Crit Care Med. 2016; 44:648–9.
Article12. Petros S, Engelmann L. Percutaneous dilatational tracheostomy in a medical ICU. Intensive Care Med. 1997; 23:630–4.13. Kluge S, Baumann HJ, Maier C, Klose H, Meyer A, Nierhaus A, et al. Tracheostomy in the intensive care unit: a nationwide survey. Anesth Analg. 2008; 107:1639–43.
Article14. McGrath BA, Brenner MJ, Warrillow SJ, Pandian V, Arora A, Cameron TS, et al. Tracheostomy in the COVID-19 era: global and multidisciplinary guidance. Lancet Respir Med. 2020; 8:717–25.
Article15. Takhar A, Walker A, Tricklebank S, Wyncoll D, Hart N, Jacob T, et al. Recommendation of a practical guideline for safe tracheostomy during the COVID-19 pandemic. Eur Arch Otorhinolaryngol. 2020; 277:2173–84.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Characteristics of Hybrid Modified Percutaneous Dilatational Tracheostomy in Patients With COVID-19: A Single Institutional Experience Over 1 Year
- Safety and Feasibility of Percutaneous Tracheostomy Performed by Medical Intensivists
- Safety and Feasibility of Percutaneous Dilatational Tracheostomy Performed by a Neurointensivist Compared with Conventional Surgical Tracheostomy in Neurosurgery Intensive Care Unit
- Safety and Feasibility of Percutaneous Dilatational Tracheostomy Performed by Intensive Care Trainee
- Assessing Clinical Feasibility and Safety of Percutaneous Dilatational Tracheostomy During Extracorporeal Membrane Oxygenation Support in the Intensive Care Unit