Acute Crit Care.
2021 Nov;36(4):351-360. 10.4266/acc.2021.00283.
Outcomes of critically ill patients according to the perception of intensivists on the appropriateness of intensive care unit admission
- Affiliations
-
- 1Division of Pulmonary and Critical Care Medicine, Department of Internal Medicine, Inje University College of Medicine, Sanggye Paik Hospital, Seoul, Korea
- 2Medical Intensive Care Unit, Asan Medical Center, Seoul, Korea
- 3Department of Pulmonary and Critical Care Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2524318
- DOI: http://doi.org/10.4266/acc.2021.00283
Abstract
- Background
It is important for intensivists to determine which patient may benefit from intensive care unit (ICU) admission. We aimed to assess the outcomes of patients perceived as non-beneficially or beneficially admitted to the ICU and evaluate whether their prognosis was consistent with the intensivists’ perception.
Methods
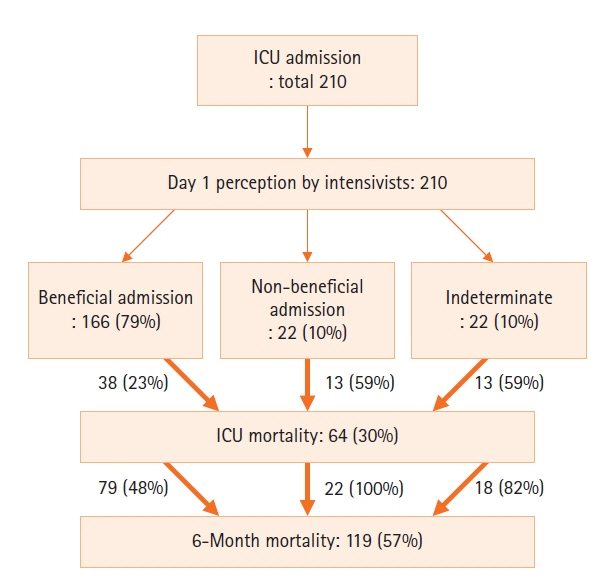
A prospective observational study was conducted on patients admitted to the medical ICU of a tertiary referral center between February and April 2014. The perceptions of four intensivists at admission (day 1) and on day 3 were investigated as non-beneficial admission, beneficial admission, or indeterminate state.
Results
A total of 210 patients were enrolled. On days 1 and 3, 22 (10%) and 23 (11%) patients were judged as having non-beneficial admission; 166 (79%) and 159 (79%), beneficial admission; and 22 (10%) and 21 (10%), indeterminate state, respectively. The ICU mortality rates of each group were 64%, 22%, and 57%, respectively; their 6-month mortality rates were 100%, 46%, and 81%, respectively. The perceptions of non-beneficial admission or indeterminate state were the significant predictors of ICU mortality (day 3, odds ratio [OR], 4.049; 95% confidence interval [CI], 1.892–8.664; P<0.001) and 6-month mortality (day 1: OR, 4.983; 95% CI, 1.260–19.703; P=0.022; day 3: OR, 4.459; 95% CI, 1.162–17.121; P=0.029).
Conclusions
The outcomes of patients perceived as having non-beneficial admission were extremely poor. The intensivists’ perception was important in predicting patients’ outcomes and was more consistent with long-term prognosis than with immediate outcomes. The intensivists’ role can be reflected in limited ICU resource utilization.
Keyword
Figure
Cited by 1 articles
-
Can the intensivists predict the outcomes of critically ill patients on the appropriateness of intensive care unit admission for limited intensive care unit resources ?
SeungYong Park
Acute Crit Care. 2021;36(4):388-389. doi: 10.4266/acc.2021.01641.
Reference
-
1. Huynh TN, Kleerup EC, Raj PP, Wenger NS. The opportunity cost of futile treatment in the ICU. Crit Care Med. 2014; 42:1977–82.
Article2. Carter HE, Winch S, Barnett AG, Parker M, Gallois C, Willmott L, et al. Incidence, duration and cost of futile treatment in end-of-life hospital admissions to three Australian public-sector tertiary hospitals: a retrospective multicentre cohort study. BMJ Open. 2017; 7:e017661.
Article3. Piers RD, Azoulay E, Ricou B, Dekeyser Ganz F, Decruyenaere J, Max A, et al. Perceptions of appropriateness of care among European and Israeli intensive care unit nurses and physicians. JAMA. 2011; 306:2694–703.
Article4. Schwarzkopf D, Rüddel H, Thomas-Rüddel DO, Felfe J, Poidinger B, Matthäus-Krämer CT, et al. Perceived nonbeneficial treatment of patients, burnout, and intention to leave the job among ICU nurses and junior and senior physicians. Crit Care Med. 2017; 45:e265–73.
Article5. Niederman MS, Berger JT. The delivery of futile care is harmful to other patients. Crit Care Med. 2010; 38(10 Suppl):S518–22.
Article6. Angus DC, Truog RD. Toward better ICU Use at the end of life. JAMA. 2016; 315:255–6.
Article7. Nates JL, Nunnally M, Kleinpell R, Blosser S, Goldner J, Birriel B, et al. ICU admission, discharge, and triage guidelines: a framework to enhance clinical operations, development of institutional policies, and further research. Crit Care Med. 2016; 44:1553–602.8. Kon AA, Shepard EK, Sederstrom NO, Swoboda SM, Marshall MF, Birriel B, et al. Defining futile and potentially inappropriate interventions: a policy statement from the Society of Critical Care Medicine Ethics Committee. Crit Care Med. 2016; 44:1769–74.9. Downar J, You JJ, Bagshaw SM, Golan E, Lamontagne F, Burns K, et al. Nonbeneficial treatment Canada: definitions, causes, and potential solutions from the perspective of healthcare practitioners. Crit Care Med. 2015; 43:270–81.10. Huynh TN, Kleerup EC, Wiley JF, Savitsky TD, Guse D, Garber BJ, et al. The frequency and cost of treatment perceived to be futile in critical care. JAMA Intern Med. 2013; 173:1887–94.
Article11. Palda VA, Bowman KW, McLean RF, Chapman MG. "Futile" care: do we provide it? Why? A semistructured, Canada-wide survey of intensive care unit doctors and nurses. J Crit Care. 2005; 20:207–13.
Article12. Afessa B, Keegan MT, Mohammad Z, Finkielman JD, Peters SG. Identifying potentially ineffective care in the sickest critically ill patients on the third ICU day. Chest. 2004; 126:1905–9.
Article13. Detsky ME, Harhay MO, Bayard DF, Delman AM, Buehler AE, Kent SA, et al. discriminative accuracy of physician and nurse predictions for mortality and functional outcomes 6 months after an ICU admission. JAMA. 2017; 317:2187–95.14. Herridge MS. Prognostication and intensive care unit outcome: the evolving role of scoring systems. Clin Chest Med. 2003; 24:751–62.
Article15. Vincent JL, Moreno R. Clinical review: scoring systems in the critically ill. Crit Care. 2010; 14:207.
Article16. Cooke CR. The siren song of simple tools that predict mortality. Respir Care. 2011; 56:533–5.
Article17. Sinuff T, Adhikari NK, Cook DJ, Schünemann HJ, Griffith LE, Rocker G, et al. Mortality predictions in the intensive care unit: comparing physicians with scoring systems. Crit Care Med. 2006; 34:878–85.
Article18. Dolgin M; New York Heart Association. Criteria Committee. Nomenclature and criteria for diagnosis of diseases of the heart and great vessels. 9th ed. Boston (MA): Little Brown & Co;1994.19. Fletcher CM. The clinical diagnosis of pulmonary emphysema; an experimental study. Proc R Soc Med. 1952; 45:577–84.20. Fletcher CM, Elmes PC, Fairbairn AS, Wood CH. The significance of respiratory symptoms and the diagnosis of chronic bronchitis in a working population. Br Med J. 1959; 2:257–66.21. McCaffery M, Beebe A. Pain: clinical manual for nursing practice. St. Louis (MO): Mosby;1989.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Can the intensivists predict the outcomes of critically ill patients on the appropriateness of intensive care unit admission for limited intensive care unit resources ?
- Intensivist as a Surgeon: The Role of a Surgeon in Critical Care Medicine
- Effect of a Clinical Nursing Practice Guideline of Enteral Nutrition Care on the Duration of Mechanical Ventilator for Critically Ill Patients
- Nutritional Support in Critically Ill Surgical Patients
- Incidence and Mortality Trends in Critically Ill Children: A Korean Population-Based Study