J Korean Med Sci.
2022 Jan;37(2):e15. 10.3346/jkms.2022.37.e15.
Rhinovirus Incidence Rates Indicate We Are Tired of Non-pharmacological Interventions Against Coronavirus Disease 2019
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, Chung-Ang University Hospital, ChungAng University College of Medicine, Seoul, Korea
- 2Department of Internal Medicine, Chung-Ang Medical Health Care System Hyundae Hospital, Namyangju, Korea
- KMID: 2524287
- DOI: http://doi.org/10.3346/jkms.2022.37.e15
Abstract
- Background
During the coronavirus disease 2019 (COVID-19) pandemic, the incidence of rhinovirus (RV) is inversely related to the intensity of non-pharmacological interventions (NPIs), such as universal mask wearing and physical distancing.
Methods
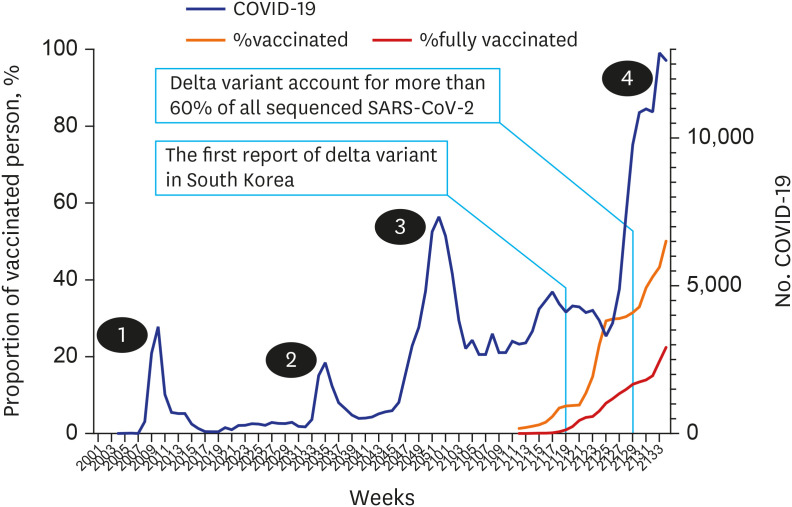
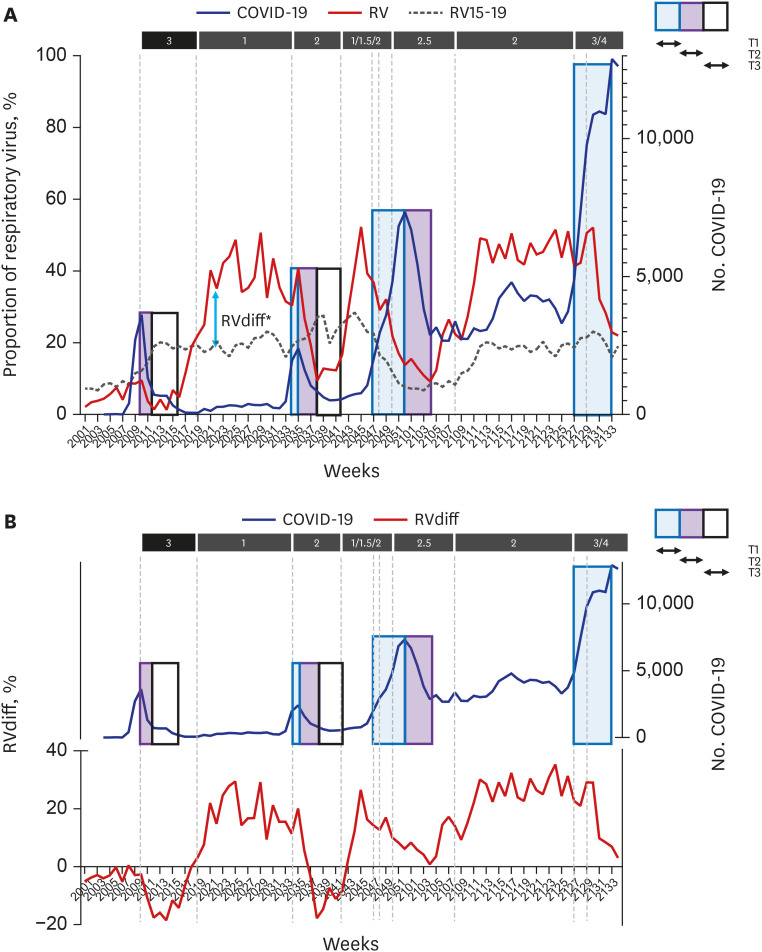
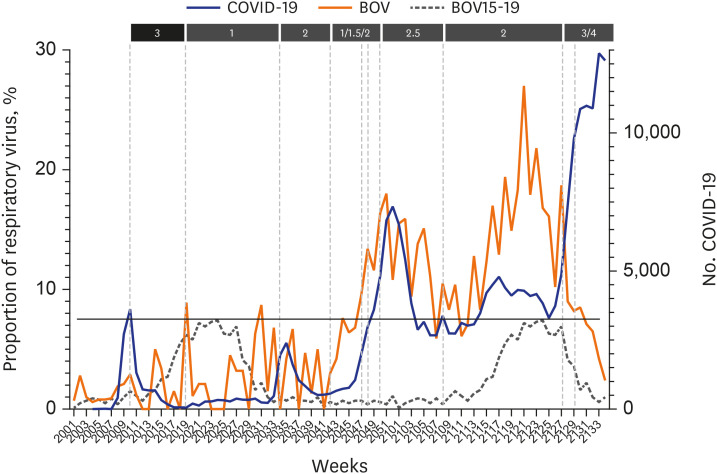
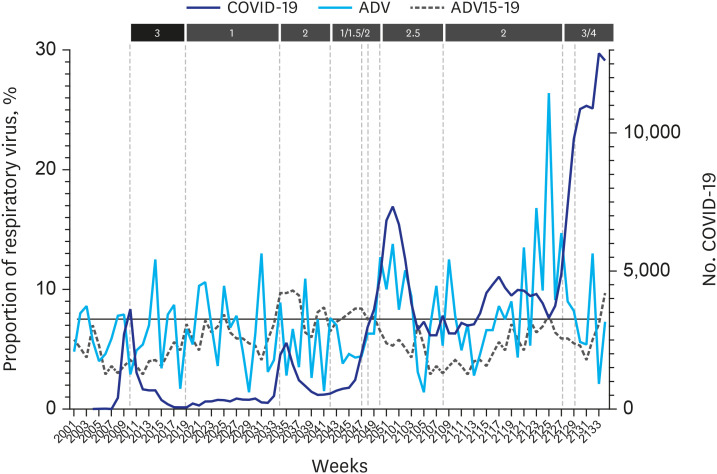
Using RV surveillance data, changes in the effect of NPIs were investigated in South Korea during the pandemic. The time to the first visible effect of NPIs after the onset of NPIs (T1), time to the maximum effect (T2), and duration of the maximum effect (T3) were measured for each surge. For each week, the RVdiff [(RV incidence during the pandemic) − (RV incidence within 5 years before the pandemic)] was calculated, and number of weeks for RVdiff to be below zero after NPIs (time to RVdiff ≤ 0) and number of weeks RVdiff remains below zero after NPIs (duration of RVdiff ≤ 0) were measured for each surge.
Results
During the study period, four surges of COVID-19 were reported. As the pandemic progressed, T1 and T2 increased, but T3 decreased. Additionally, the “time to RVdiff of ≤ 0” increased and “duration of RVdiff of ≤ 0” decreased. These changes became more pronounced during the third surge (mid-November 2020), before the introduction of the COVID-19 vaccine, and from the emergence of the delta variant.
Conclusion
The effect of NPIs appears slower, the duration of the effect becomes shorter, and the intensity also decreases less than a year after the onset of the pandemic owing to people’s exhaustion in implementing NPIs. These findings suggest that the COVID-19 response strategy must be completely overhauled
Figure
Reference
-
1. Yoo JH. The fight against the 2019-nCoV outbreak: an arduous march has just begun. J Korean Med Sci. 2020; 35(4):e56. PMID: 31997618.
Article2. Kim MN. What type of face mask is appropriate for everyone-mask-wearing policy amidst COVID-19 pandemic? J Korean Med Sci. 2020; 35(20):e186. PMID: 32449327.
Article3. Jang WM, Jang DH, Lee JY. Social distancing and transmission-reducing practices during the 2019 coronavirus disease and 2015 middle east respiratory syndrome coronavirus outbreaks in Korea. J Korean Med Sci. 2020; 35(23):e220. PMID: 32537955.
Article4. Bae S, Lee YW, Lim SY, Lee JH, Lim JS, Lee S, et al. Adverse reactions following the first dose of ChAdOx1 nCoV-19 vaccine and BNT162b2 vaccine for healthcare workers in South Korea. J Korean Med Sci. 2021; 36(17):e115. PMID: 33942579.
Article5. Korea Disease Control and Prevention Agency. Coronavirus disease 2019 (COVID-19). Updated 2021. Accessed September 2, 2021. http://ncov.mohw.go.kr .6. Rodgers L, Sheppard M, Smith A, Dietz S, Jayanthi P, Yuan Y, et al. Changes in seasonal respiratory illnesses in the United States during the coronavirus disease 2019 (COVID-19) pandemic. Clin Infect Dis. 2021; 73(Suppl 1):S110–S117. PMID: 33912902.
Article7. Redlberger-Fritz M, Kundi M, Aberle SW, Puchhammer-Stöckl E. Significant impact of nationwide SARS-CoV-2 lockdown measures on the circulation of other respiratory virus infections in Austria. J Clin Virol. 2021; 137:104795. PMID: 33761423.
Article8. Park KY, Seo S, Han J, Park JY. Respiratory virus surveillance in Canada during the COVID-19 pandemic: an epidemiological analysis of the effectiveness of pandemic-related public health measures in reducing seasonal respiratory virus test positivity. PLoS One. 2021; 16(6):e0253451. PMID: 34143839.9. Chen APL, Chu IYH, Yeh ML, Chen YY, Lee CL, Lin HH, et al. Differentiating impacts of non-pharmaceutical interventions on non-coronavirus disease-2019 respiratory viral infections: Hospital-based retrospective observational study in Taiwan. Influenza Other Respir Viruses. 2021; 15(4):478–487. PMID: 33825310.
Article10. Park S, Michelow IC, Choe JY. Shifting patterns of respiratory virus activity following social distancing measures for coronavirus disease 2019 in South Korea. J Infect Dis. 2021; 224(11):1900–1906. PMID: 34009376.
Article11. Haapanen M, Renko M, Artama M, Kuitunen I. The impact of the lockdown and the re-opening of schools and day cares on the epidemiology of SARS-CoV-2 and other respiratory infections in children – a nationwide register study in Finland. EClinicalMedicine. 2021; 34:100807. PMID: 33817612.
Article12. Sullivan GS, Carlson S, Cheng AC, Chilver MB, Dwyer DE, Irwin M, et al. Where has all the influenza gone? The impact of COVID-19 on the circulation of influenza and other respiratory viruses, Australia, March to September 2020. Euro Surveill. 2020; 25(47):2001847.
Article13. Nawrocki J, Olin K, Holdrege MC, Hartsell J, Meyers L, Cox C, et al. The effects of social distancing policies on non-SARS-CoV-2 respiratory pathogens. Open Forum Infect Dis. 2021; 8(7):ofab133. PMID: 34322558.
Article14. Kim MC, Kweon OJ, Lim YK, Choi SH, Chung JW, Lee MK. Impact of social distancing on the spread of common respiratory viruses during the coronavirus disease outbreak. PLoS One. 2021; 16(6):e0252963. PMID: 34125839.
Article15. Kitanovski S, Horemheb-Rubio G, Adams O, Gärtner B, Lengauer T, Hoffmann D, et al. Rhinovirus prevalence as indicator for efficacy of measures against SARS-CoV-2. BMC Public Health. 2021; 21(1):1178. PMID: 34154549.
Article16. Poole S, Brendish NJ, Tanner AR, Clark TW. Physical distancing in schools for SARS-CoV-2 and the resurgence of rhinovirus. Lancet Respir Med. 2020; 8(12):e92–e93. PMID: 33289636.
Article17. Our world in Data. Coronavirus (COVID-19) vaccinations. Updated 2021. Accessed September 2, 2021. https://ourworldindata.org/covid-vaccinations?country=KOR .18. Luo CH, Morris PC, Sachithanandham J, Amadi A, Gastron D, Li M, et al. Infection with the SARS-CoV-2 delta variant is associated with higher infectious virus loads compared to the alpha variant in both unvaccinated and vaccinated individuals. medRxiv. DOI: 10.1101/2021.08.15.21262077. August 20, 2021.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Role of Respiratory Viral Infections in Exacerbation of Asthma and Chronic Obstructive Pulmonary Disease (COPD)
- Impact of the coronavirus disease 2019 pandemic on the incidence of other infectious diseases in the hematology hospital in Korea
- Clinical and Epidemiological Characteristics of Coronavirus Disease 2019 in the Early Stage of Outbreak
- Recommendations of Pharmacological Treatment inChildhood and Adolescents Obesity
- The Characteristics of Middle Eastern Respiratory Syndrome Coronavirus Transmission Dynamics in South Korea