J Korean Med Sci.
2022 Jan;37(1):e1. 10.3346/jkms.2022.37.e1.
Prevalence and Premature Mortality Statistics of Autism Spectrum Disorder Among Children in Korea: A Nationwide Population-Based Birth Cohort Study
- Affiliations
-
- 1Graduate School of Public Health, Korea University, Seoul, Korea
- 2Department of Preventive Medicine and Public Health, Ajou University School of Medicine, Suwon, Korea
- 3Graduate School of Public Health, Seoul National University, Seoul, Korea
- 4Department of Nursing Science, Shinsung University, Dangjin, Korea
- 5Department of Pharmaceutical Engineering, Cheongju University, Cheongju, Korea
- 6Public Healthcare Center, Seoul National University Hospital, Seoul, Korea
- 7Department of Health Policy and Management, Seoul National University College of Medicine, Seoul, Korea
- 8HIRA Research Institute, Health Insurance Review and Assessment Service, Wonju, Korea
- KMID: 2524179
- DOI: http://doi.org/10.3346/jkms.2022.37.e1
Abstract
- Background
The aim of this study was to estimate the 8-year prevalence and mortality statistics of autism spectrum disorder (ASD) according to birth year (2002–2012).
Methods
We used the National Health Insurance Service database with 4,989,351 children born from 2002 to 2012 including 35,529 children diagnosed with ASD until 8 years of age. The 8-year cumulative prevalence of ASD was calculated annually (2010–2020) with 8 years of follow-up. The 8-year mortality was estimated using Cox models adjusted for sex, household income, area of residence, and year of birth.
Results
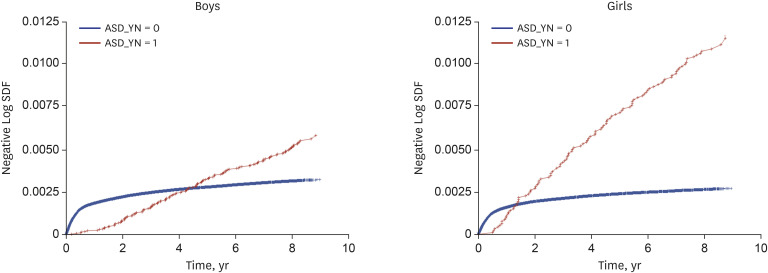
Of the 473,494 children born in 2002, 2,467 (5.2 per 1,000 births) were diagnosed with ASD until 2010. The ASD prevalence was 2.6 times higher among boys (1,839; 7.4 per 1,000 boy births) than girls (628; 2.8 per 1,000 girl births). Of the 467,360 children born in 2012, 4,378 (9.4 per 1,000 births) were diagnosed with ASD until 2020. The ASD prevalence was 2.7 times higher among boys (3,246; 13.5 per 1,000 boy births) than girls (1,132; 5.0 per 1,000 girl births). The risk of all-cause mortality was higher among children with ASD than those without (hazard ratio [HR], 2.340; 95% confidence interval [CI], 2.063–2.654), which is substantially higher among girls (HR, 4.223; 95% CI, 3.472–5.135) than boys (HR, 1.774; 95% CI, 1.505–2.090).
Conclusion
The present study demonstrated that national-level prevalence and mortality statistics of ASD can be estimated effectively using claims data comprising newborns born each year and followed up for to the age of interest. Because this information is essential to establish evidence-based policies, health authorities need to consider producing epidemiological information of ASD continuously using the same methodology.
Figure
Reference
-
1. Lee JY, Yun J. What else is needed in the Korean government’s master plan for people with developmental disabilities? J Prev Med Public Health. 2019; 52(3):200–204. PMID: 31163956.
Article2. Yun J. The necessity of comprehensive service institution for people with autism: Lessons from the North Carolina TEACCH program in United States. Public Health Affairs. 2019; 3(1):147–154.
Article3. Yun J, Lee JY. Implications for the US Medicaid role expansion for people with autistic spectrum disorder. Glob Soc Secur Rev. 2019; 9:59–67.4. Lee JY, Yun JE, Jang WM. Barriers to estimation of number of adults with autism spectrum disorders. J Rehab Res. 2019; 23(2):1–14.
Article5. Yun J, Kim HJ. Trend analysis of medical care utilization among people with autistic spectrum disorder using national health insurance data. J Digit Converg. 2018; 16(11):411–418.6. Maenner MJ, Shaw KA, Baio J, Washington A, Patrick M, DiRienzo M, EdS1; PhD-7, et al. Prevalence of autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network, 11 sites, United States, 2016. MMWR Surveill Summ. 2020; 69(4):1–12.7. Autism and Developmental Disabilities Monitoring Network Surveillance Year 2006 Principal Investigators. Centers for Disease Control and Prevention (CDC). Prevalence of autism spectrum disorders - Autism and Developmental Disabilities Monitoring Network, United States, 2006. MMWR Surveill Summ. 2009; 58(10):1–20.8. Kim YS, Leventhal BL, Koh YJ, Fombonne E, Laska E, Lim EC, et al. Prevalence of autism spectrum disorders in a total population sample. Am J Psychiatry. 2011; 168(9):904–912. PMID: 21558103.
Article9. Hong M, Lee SM, Park S, Yoon SJ, Kim YE, Oh IH. Prevalence and economic burden of autism spectrum disorder in South Korea using national health insurance data from 2008 to 2015. J Autism Dev Disord. 2020; 50(1):333–339. PMID: 31630294.
Article10. Yoo HJ. Recent increase in autism and ADHD: true or inflated? J Korean Med Sci. 2013; 28(7):974–975. PMID: 23853476.
Article11. National Health Insurance. Updated 2020. Accessed April 5, 2021. https://www.nhis.or.kr/nhis/policy/wbhada01700m01.do .12. Hwang YI, Srasuebkul P, Foley KR, Arnold S, Trollor JN. Mortality and cause of death of Australians on the autism spectrum. Autism Res. 2019; 12(5):806–815. PMID: 30802364.
Article13. Bachmann CJ, Gerste B, Hoffmann F. Diagnoses of autism spectrum disorders in Germany: time trends in administrative prevalence and diagnostic stability. Autism. 2018; 22(3):283–290. PMID: 29671642.
Article14. Developmental Disabilities Monitoring Network Surveillance Year 2010 Principal Investigators. Centers for Disease Control and Prevention (CDC). Prevalence of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2010. MMWR Surveill Summ. 2014; 63(2):1–21.15. Guan J, Li G. Injury mortality in individuals with autism. Am J Public Health. 2017; 107(5):791–793. PMID: 28323463.
Article16. Özerk K, Cardinal D. Prevalence of autism/ASD among preschool and school-age children in Norway. Contemp Sch Psychol. 2020; 24(4):419–428.
Article17. Chiarotti F, Venerosi A. Epidemiology of autism spectrum disorders: a review of worldwide prevalence estimates since 2014. Brain Sci. 2020; 10(5):274.
Article18. Christensen DL, Braun KV, Baio J, Bilder D, Charles J, Constantino JN, et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years—autism and developmental disabilities monitoring network, 11 sites, United States, 2012. MMWR Surveill Summ. 2018; 65(13):1–23. PMID: 30439868.19. Ofner M, Coles A, Decou ML, Do MT, Bienek A, Snider J, et al. Autism Spectrum Disorder among Children and Youth in Canada 2018. Ottawa, ON: Public Health Agency of Canada;2018.20. Schendel DE, Overgaard M, Christensen J, Hjort L, Jørgensen M, Vestergaard M, et al. Association of psychiatric and neurologic comorbidity with mortality among persons with autism spectrum disorder in a Danish population. JAMA Pediatr. 2016; 170(3):243–250. PMID: 26752506.
Article21. Rah SS, Hong SB, Yoon JY. Prevalence and incidence of developmental disorders in Korea: a nationwide population-based study. J Autism Dev Disord. 2020; 50(12):4504–4511. PMID: 32347466.
Article22. Shaw KA, Maenner MJ, Baio J, Washington A, Christensen DL, Wiggins LD, et al. EdS1. Early identification of autism spectrum disorder among children aged 4 years—Early Autism and Developmental Disabilities Monitoring Network, six sites, United States, 2016. MMWR Surveill Summ. 2020; 69(3):1–11.23. Zuckerman KE, Broder-Fingert S, Sheldrick RC. To reduce the average age of autism diagnosis, screen preschoolers in primary care. Autism. 2021; 25(2):593–596. PMID: 33126817.
Article24. Gillberg C, Billstedt E, Sundh V, Gillberg IC. Mortality in autism: a prospective longitudinal community-based study. J Autism Dev Disord. 2010; 40(3):352–357. PMID: 19838782.
Article25. Mouridsen SE, Brønnum-Hansen H, Rich B, Isager T. Mortality and causes of death in autism spectrum disorders: an update. Autism. 2008; 12(4):403–414. PMID: 18579647.26. Woolfenden S, Sarkozy V, Ridley G, Coory M, Williams K. A systematic review of two outcomes in autism spectrum disorder - epilepsy and mortality. Dev Med Child Neurol. 2012; 54(4):306–312. PMID: 22348343.
Article27. Bilder D, Botts EL, Smith KR, Pimentel R, Farley M, Viskochil J, et al. Excess mortality and causes of death in autism spectrum disorders: a follow up of the 1980s Utah/UCLA autism epidemiologic study. J Autism Dev Disord. 2013; 43(5):1196–1204. PMID: 23008058.
Article28. Hirvikoski T, Mittendorfer-Rutz E, Boman M, Larsson H, Lichtenstein P, Bölte S. Premature mortality in autism spectrum disorder. Br J Psychiatry. 2016; 208(3):232–238. PMID: 26541693.
Article29. Durkin MS, Maenner MJ, Meaney FJ, Levy SE, DiGuiseppi C, Nicholas JS, et al. Socioeconomic inequality in the prevalence of autism spectrum disorder: evidence from a U.S. cross-sectional study. PLoS One. 2010; 5(7):e11551. PMID: 20634960.
Article30. King MD, Bearman PS. Socioeconomic status and the increased prevalence of autism in California. Am Sociol Rev. 2011; 76(2):320–346. PMID: 21547238.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prevalence of Pediatric Autism Spectrum Disorder in Korea Using National Statistics Including the COVID-19 Pandemic, 2011 to 2021
- Overweight & Obesity in Children & Adolescents with Autism Spectrum Disorders: Retrospective Chart Review
- Comparison of the Autism Diagnostic Observation Schedule and Childhood Autism Rating Scale in the Diagnosis of Autism Spectrum Disorder: A Preliminary Study
- Mortality of Children with Autism Spectrum Disorder Using Data from a Large-Scale Korean National Cohort
- Psychosocial Treatments for Children with Autism Spectrum Disorder