J Korean Neurosurg Soc.
2022 Jan;65(1):84-95. 10.3340/jkns.2021.0147.
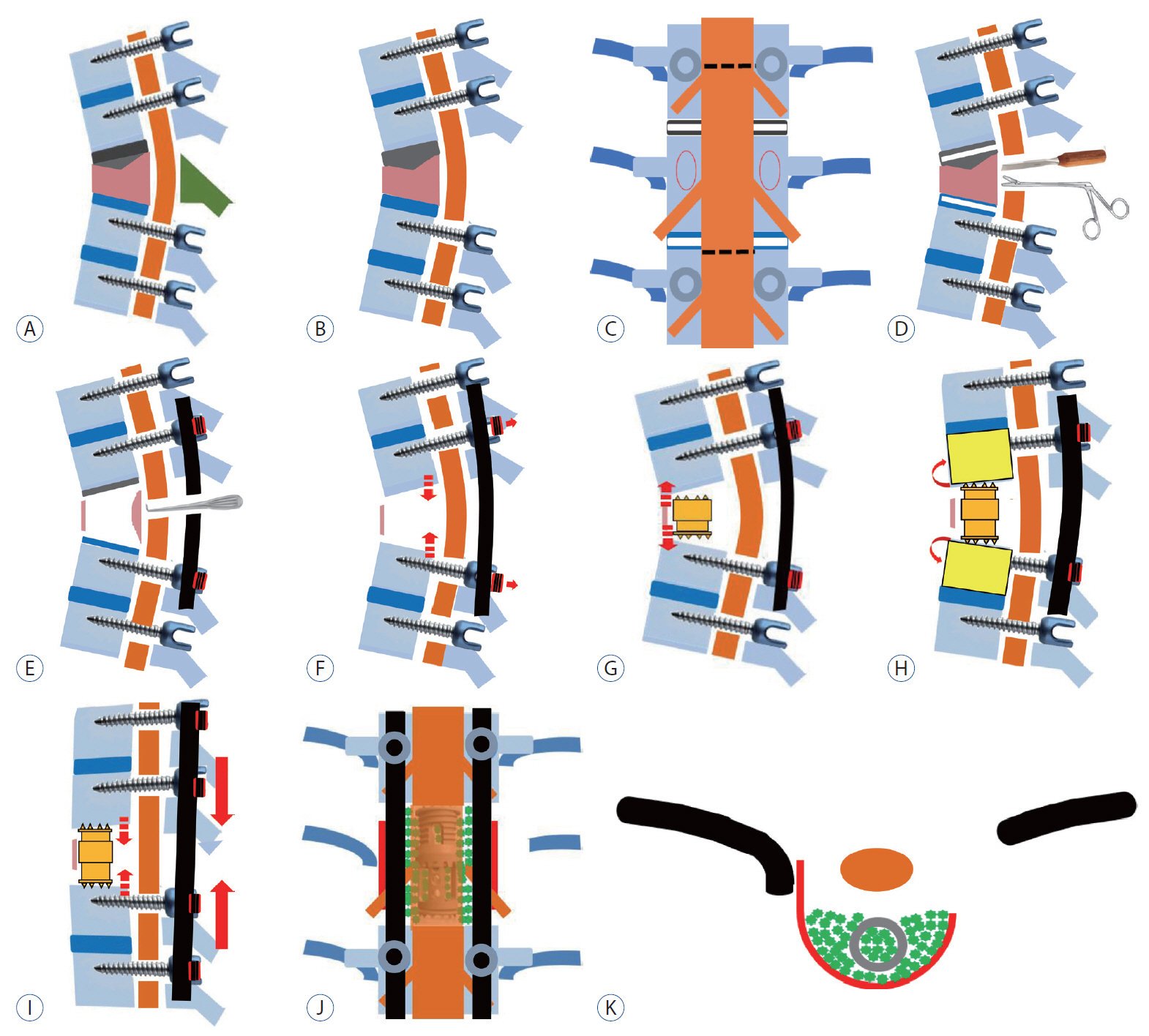
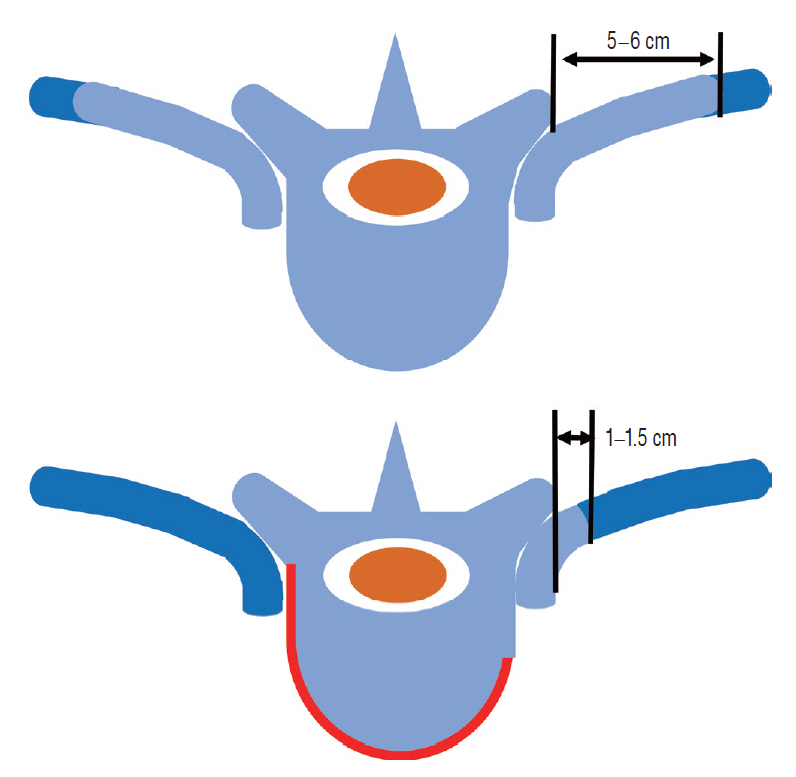
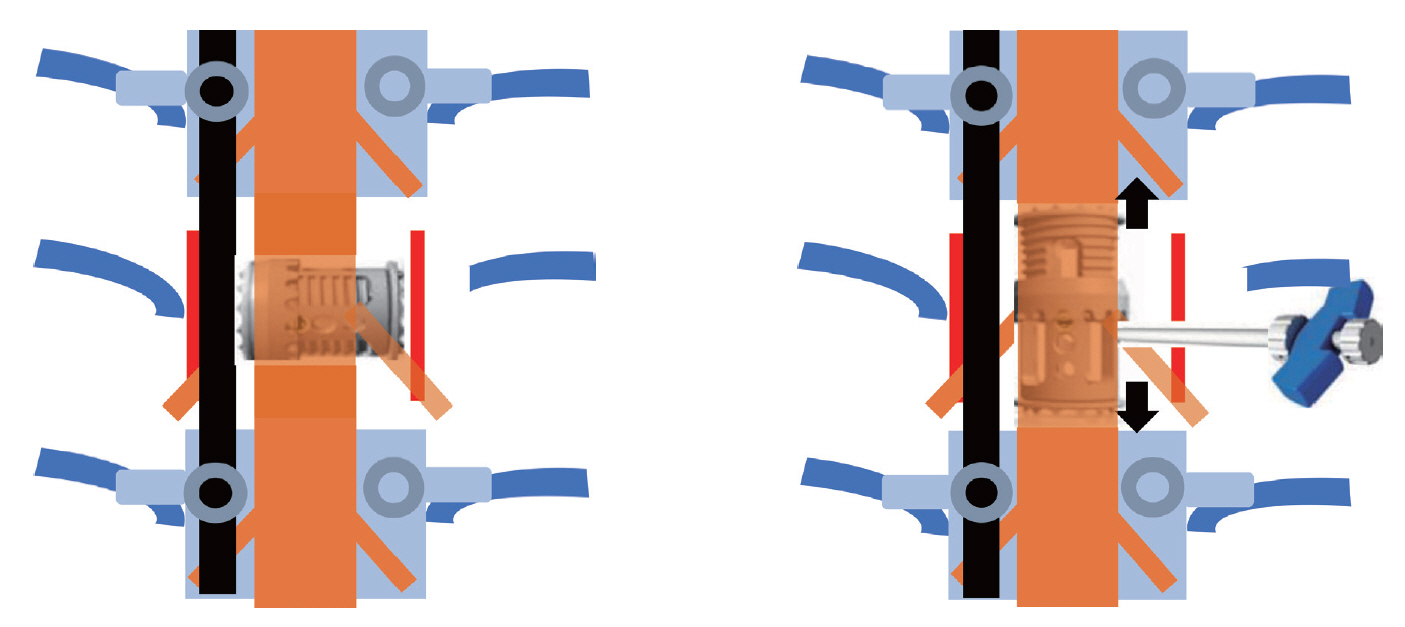
Clinical Efficacy and Safety of Controlled Distraction-Compression Technique Using Expandable Titanium Cage in Correction of Posttraumatic Kyphosis
- Affiliations
-
- 1Department of Neurosurgery, School of Medicine, Gyeongsang National University, Jinju, Korea
- 2Division of Orthopaedic Surgery, University Health Network, Toronto Western Hospital, Toronto, Canada
- KMID: 2523916
- DOI: http://doi.org/10.3340/jkns.2021.0147
Abstract
Objective
: To investigate the clinical efficacy and safety of the controlled distraction-compression technique using an expandable titanium cage (ETC) in posttraumatic kyphosis (PTK).
Methods
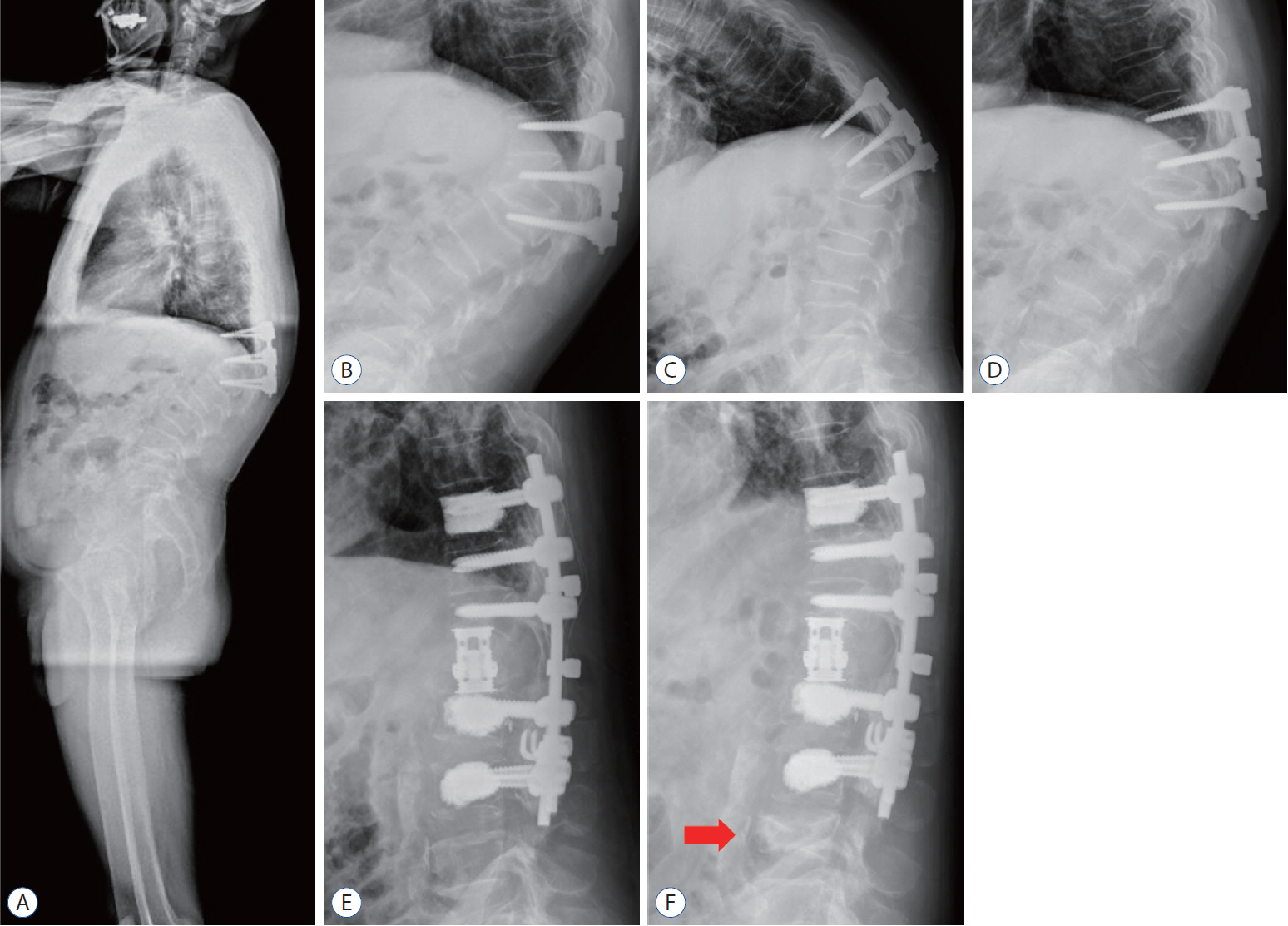
: We retrospectively studied and collected data on 20 patients with PTK. From January 2014 to December 2017, the controlled distraction-compression technique using ETC was consecutively performed in 20 patients with PTK of the thoracolumbar zone (range, 36–82 years). Among them, nine were males and 11 were females and the mean age was 61.5 years. The patients were followed regularly at 1, 3, 6, and 12 months, and the last follow-up was more than 2 years after surgery.
Results
: The mean follow-up period was 27.3±7.3 months (range, 14–48). The average operation time was 286.8±33.1 minutes (range, 225–365). The preoperative regional kyphotic angle (RKA) ranged from 35.6° to 70.6° with an average of 47.5°±8.1°. The immediate postoperative mean RKA was 5.9°±3.8° (86.2% correction rate, p=0.000), and at the last follow-up more than 2 years later, the mean RKA was 9.2°±4.9° (80.2% correction rate, p=0.000). The preoperative mean thoracolumbar kyphosis was 49.1°±9.2° and was corrected to an average of 8.8°±5.3° immediately after surgery (p=0.000). At the last follow-up, a correction of 11.9°±6.3° was obtained (p=0.000). The preoperative mean back visual analog scale (VAS) score was 7.9±0.8 and at the last follow-up, the VAS score was improved to a mean of 2.3±1.0 with a 70.9% correction rate (p=0.000). The preoperative mean Oswestry disability index (ODI) score was 32.3±6.9 (64.6%) and the last follow-up ODI score was improved to a mean of 6.85±2.9 (3.7%) with a 78.8% correction rate (p=0.000). The overall complication was 15%, with two of distal junctional fractures and one of proximal junctional kyphosis and screw loosening. However, there were no complications directly related to the operation.
Conclusion
: PVCR through the controlled distraction-compression technique using ETC showed safe and good results in terms of complications, and clinical and radiologic outcomes in PTK. However, to further evaluate the efficacy of this surgical procedure, more patients need long-term follow-up and there is a need to apply it to other diseases.
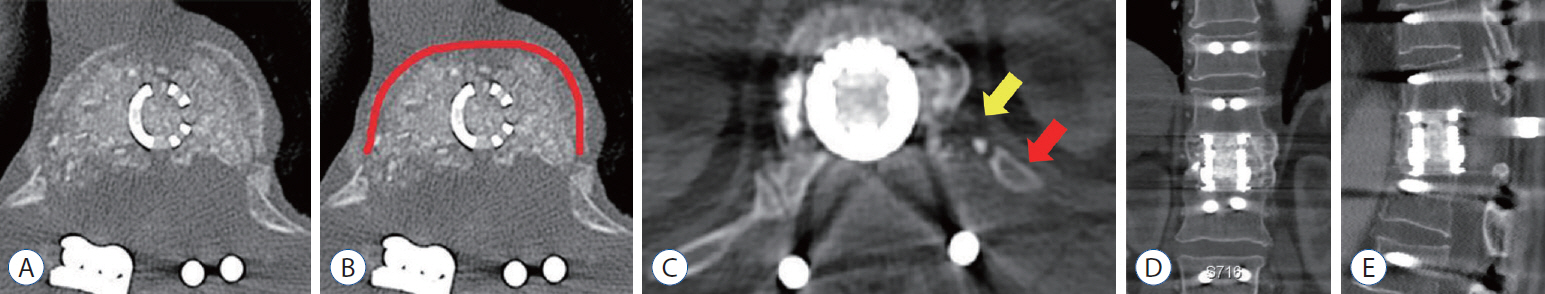
Figure
Reference
-
References
1. Auerbach JD, Lenke LG, Bridwell KH, Sehn JK, Milby AH, Bumpass D, et al. Major complications and comparison between 3-column osteotomy techniques in 105 consecutive spinal deformity procedures. Spine (Phila Pa 1976). 37:1198–1210. 2012.
Article2. Berven SH, Deviren V, Smith JA, Hu SH, Bradford DS. Management of fixed sagittal plane deformity: outcome of combined anterior and posterior surgery. Spine (Phila Pa 1976). 28:1710–1715. discussion 1716. 2003.
Article3. Bourghli A, Boissière L, Vital JM, Bourghli MA, Almusrea K, Khoury G, et al. Modified closing-opening wedge osteotomy for the treatment of sagittal malalignment in thoracolumbar fractures malunion. Spine J. 15:2574–2582. 2015.
Article4. Buchowski JM, Kuhns CA, Bridwell KH, Lenke LG. Surgical management of posttraumatic thoracolumbar kyphosis. Spine J. 8:666–677. 2008.
Article5. Busscher I, Ploegmakers JJ, Verkerke GJ, Veldhuizen AG. Comparative anatomical dimensions of the complete human and porcine spine. Eur Spine J. 19:1104–1114. 2010.
Article6. Chang KW. Oligosegmental correction of post-traumatic thoracolumbar angular kyphosis. Spine (Phila Pa 1976). 18:1909–1915. 1993.
Article7. Chang KW, Cheng CW, Chen HC, Chang KI, Chen TC. Closing-opening wedge osteotomy for the treatment of sagittal imbalance. Spine (Phila Pa 1976). 33:1470–1477. 2008.
Article8. Chikhale C, Swar A, Khurjekar K. Modified vertebral column resection technique for correcting congenital rigid angular kyphosis and its effect on functional outcomes. J Clin Diagn Res. 10:RC17–RC22. 2016.9. Cho KJ, Bridwell KH, Lenke LG, Berra A, Baldus C. Comparison of smith-petersen versus pedicle subtraction osteotomy for the correction of fixed sagittal imbalance. Spine (Phila Pa 1976). 30:2030–2037. discussion 2038. 2005.
Article10. El-Sharkawi MM, Koptan WM, El-Miligui YH, Said GZ. Comparison between pedicle subtraction osteotomy and anterior corpectomy and plating for correcting post-traumatic kyphosis: a multicenter study. Eur Spine J. 20:1434–1440. 2011.
Article11. Glassman SD, Bridwell K, Dimar JR, Horton W, Berven S, Schwab F. The impact of positive sagittal balance in adult spinal deformity. Spine (Phila Pa 1976). 30:2024–2029. 2005.
Article12. Hao CK, Li WS, Chen ZQ. The height of the osteotomy and the correction of the kyphotic angle in thoracolumbar kyphosis. Chin Med J (Engl). 121:1906–1910. 2008.
Article13. Hong JY, Suh SW, Lee SH, Park JH, Park SY, Rhyu IJ, et al. Continuous distraction-induced delayed spinal cord injury on motor-evoked potentials and histological changes of spinal cord in a porcine model. Spinal Cord. 54:649–655. 2016.
Article14. Hyun SJ, Rhim SC. Clinical outcomes and complications after pedicle subtraction osteotomy for fixed sagittal imbalance patients : a long-term follow-up data. J Korean Neurosurg Soc. 47:95–101. 2010.
Article15. Ji L, Dang XQ, Lan BS, Wang KZ, Huang YJ, Wen B, et al. Study on the safe range of shortening of the spinal cord in canine models. Spinal Cord. 51:134–138. 2013.
Article16. Kawahara N, Tomita K, Baba H, Kobayashi T, Fujita T, Murakami H. Closing-opening wedge osteotomy to correct angular kyphotic deformity by a single posterior approach. Spine (Phila Pa 1976). 26:391–402. 2001.
Article17. Kawahara N, Tomita K, Kobayashi T, Abdel-Wanis ME, Murakami H, Akamaru T. Influence of acute shortening on the spinal cord: an experimental study. Spine (Phila Pa 1976). 30:613–620. 2005.
Article18. Kim SS, Cho BC, Kim JH, Lim DJ, Park JY, Lee BJ, et al. Complications of posterior vertebral resection for spinal deformity. Asian Spine J. 6:257–265. 2012.
Article19. Kostuik JP, Matsusaki H. Anterior stabilization, instrumentation, and decompression for post-traumatic kyphosis. Spine (Phila Pa 1976). 14:379–386. 1989.
Article20. Lafage V, Schwab F, Vira S, Patel A, Ungar B, Farcy JP. Spino-pelvic parameters after surgery can be predicted: a preliminary formula and validation of standing alignment. Spine (Phila Pa 1976). 36:1037–1045. 2011.21. Lazennec JY, Neves N, Rousseau MA, Boyer P, Pascal-Mousselard H, Saillant G. Wedge osteotomy for treating post-traumatic kyphosis at thoracolumbar and lumbar levels. J Spinal Disord Tech. 19:487–494. 2006.
Article22. Lee JH, Oh HS, Choi JG. Comparison of the posterior vertebral column resection with the expandable cage versus the nonexpandable cage in thoracolumbar angular kyphosis. Clin Spine Surg. 30:E398–E406. 2017.
Article23. Lenke LG, Newton PO, Sucato DJ, Shufflebarger HL, Emans JB, Sponseller PD, et al. Complications after 147 consecutive vertebral column resections for severe pediatric spinal deformity: a multicenter analysis. Spine (Phila Pa 1976). 38:119–132. 2013.
Article24. Liu X, Yuan S, Tian Y, Wang L, Zheng Y, Li J. Expanded eggshell procedure combined with closing-opening technique (a modified vertebral column resection) for the treatment of thoracic and thoracolumbar angular kyphosis. J Neurosurg Spine. 23:42–48. 2015.
Article25. Modi HN, Suh SW, Hong JY, Yang JH. The effects of spinal cord injury induced by shortening on motor evoked potentials and spinal cord blood flow: an experimental study in Swine. J Bone Joint Surg Am. 93:1781–1789. 2011.
Article26. Oda I, Cunningham BW, Buckley RA, Goebel MJ, Haggerty CJ, Orbegoso CM, et al. Does spinal kyphotic deformity influence the biomechanical characteristics of the adjacent motion segments? An in vivo animal model. Spine (Phila Pa 1976). 24:2139–2146. 1999.
Article27. Ozturk C, Alanay A, Ganiyusufoglu K, Karadereler S, Ulusoy L, Hamzaoglu A. Short-term X-ray results of posterior vertebral column resection in severe congenital kyphosis, scoliosis, and kyphoscoliosis. Spine (Phila Pa 1976). 37:1054–1057. 2012.
Article28. Papadopoulos EC, Boachie-Adjei O, Hess WF, Sanchez Perez-Grueso FJ, Pellisé F, Gupta M, et al. Early outcomes and complications of posterior vertebral column resection. Spine J. 15:983–991. 2015.
Article29. Roberson JR, Whitesides TE Jr. Surgical reconstruction of late posttraumatic thoracolumbar kyphosis. Spine (Phila Pa 1976). 10:307–312. 1985.
Article30. Wang H, Zhang D, Sun YP, Ma L, Ding WY, Shen Y, et al. Unilateral posterior vertebral column resection for severe thoracolumbar kyphotic deformity caused by old compressive vertebrae fracture: a technical improvement. Int J Clin Exp Med. 8:3579–3584. 2015.31. Wang Y, Zhang Y, Zhang X, Huang P, Xiao S, Wang Z, et al. A single posterior approach for multilevel modified vertebral column resection in adults with severe rigid congenital kyphoscoliosis: a retrospective study of 13 cases. Eur Spine J. 17:361–372. 2008.
Article32. Wu J, Xue J, Huang R, Zheng C, Cui Y, Rao S. A rabbit model of lumbar distraction spinal cord injury. Spine J. 16:643–658. 2016.
Article33. Xie J, Wang Y, Zhao Z, Zhang Y, Si Y, Li T, et al. Posterior vertebral column resection for correction of rigid spinal deformity curves greater than 100°. J Neurosurg Spine. 17:540–551. 2012.
Article34. Yang JH, Suh SW, Modi HN, Ramani ET, Hong JY, Hwang JH, et al. Effects of vertebral column distraction on transcranial electrical stimulation-motor evoked potential and histology of the spinal cord in a porcine model. J Bone Joint Surg Am. 95:835–842. S1-S2. 2013.
Article35. Zeng Y, Chen Z, Sun C, Li W, Qi Q, Guo Z, et al. Posterior surgical correction of posttraumatic kyphosis of the thoracolumbar segment. J Spinal Disord Tech. 26:37–41. 2013.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Safety and Efficacy of Cadaveric Allografts and Titanium Cage as a Fusion Substitutes in Pyogenic Osteomyelitis
- Comparison of Clinical and Radiologic Results between Expandable Cages and Titanium Mesh Cages for Thoracolumbar Burst Fracture
- The Use of Dual Direction Expandable Titanium Cage With Biportal Endoscopic Transforaminal Lumbar Interbody Fusion: A Technical Consideration With Preliminary Results
- Thoracoscopic Correction of Post-traumatic Kyphosis with an Expandable Cage: Radiologic and Patient-Reported Outcomes
- Surgical Treatment in Delayed Posttraumatic Thoracolumbar Kyphosis