J Korean Neurosurg Soc.
2022 Jan;65(1):30-39. 10.3340/jkns.2021.0116.
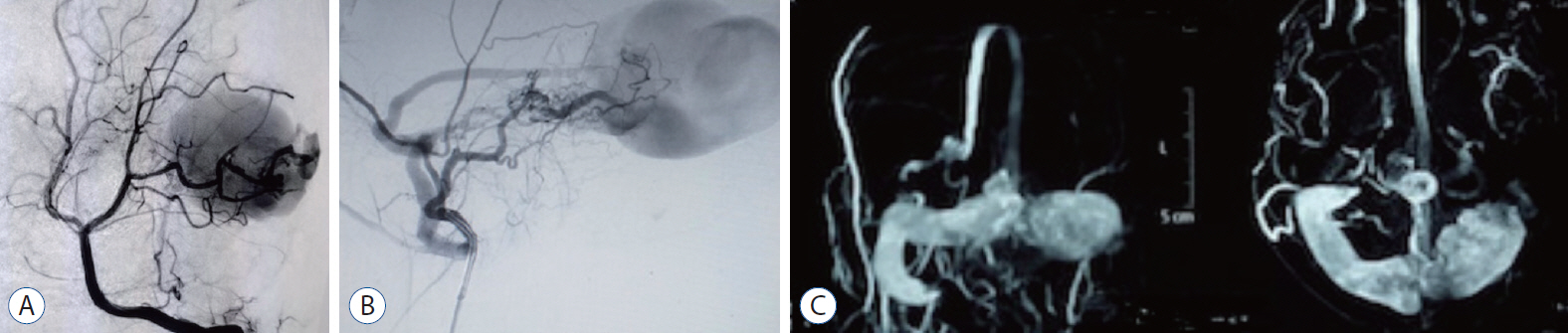
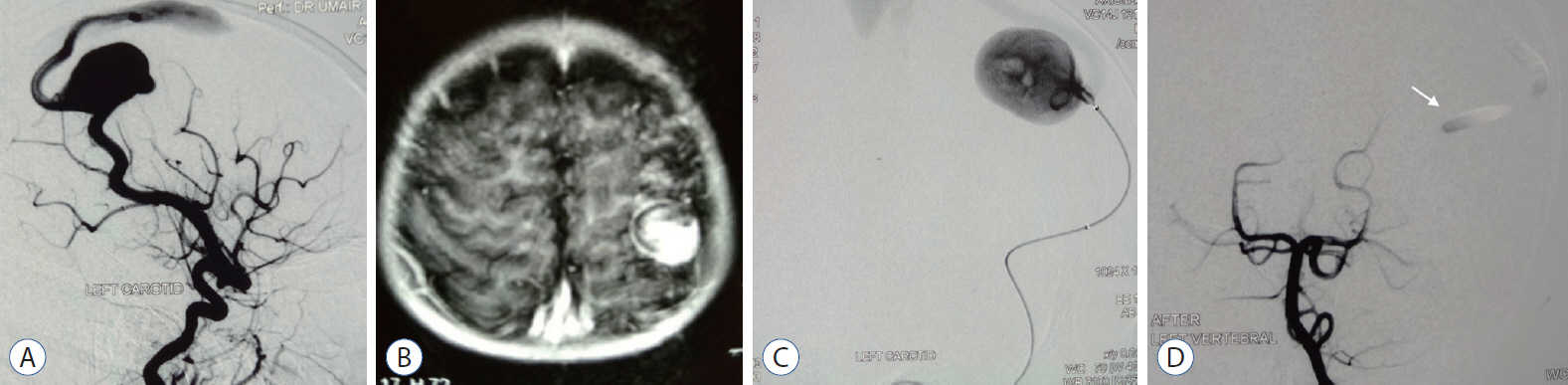
Transarterial Embolization of Intracranial Arteriovenous Fistulas with Large Venous Pouches in the Form of Venous Outlet Ectasia and Large Venous Varix or Aneurysm : Two Centers Experience
- Affiliations
-
- 1Department of Neurosurgery, Mansoura University Hospitals, Mansoura University, Mansoura, Egypt
- 2Department of Diagnostic and Interventional Neuroradiology, Lahore General Hospital, Post Graduate Medical Institute, Ameer-ud-Din Medical College, Lahore, Pakistan
- KMID: 2523911
- DOI: http://doi.org/10.3340/jkns.2021.0116
Abstract
Objective
: There are different types of cerebral vascular malformations. Pial arteriovenous fistulas (PAVFs) and dural arteriovenous fistulas (DAVFs) are two entities; they consist of one or more arterial connections to a single venous outlet without a true intervening nidus. The high turbulent flow of PAVFs and aggressive DAVFs with cortical venous reflux can result in venous outflow varix and aneurysmal dilatation. They pose a significant challenge to transvenous embolization (TVE), stereotactic radiosurgery, and surgical treatment. We aim to share our centers’ experience with the transarterial embolization (TAE) for arteriovenous fistulas (AVFs) with large venous pouches and to report the outcome.
Methods
: The authors’ two institutions’ databases were retrospectively reviewed from February 2017 to February 2021. All patients with intracranial high flow PAVFs and aggressive DAVFs with venous outlet ectasia and large venous varix and were treated by TAE were included.
Results
: Fifteen patients harboring 11 DAVFs and four PAVFs met our inclusion criteria. All patients underwent TAE in 17 sessions. Complete angiographic obliteration was achieved after 14 sessions in 12 patients (80%). Four patients (25%) had residual after one TAE session. Technical failure was documented in one patient (6.7%). Fourteen patients (93.3%) had favorable functional outcome (modified Rankin score 0–2).
Conclusions
: TAE for high flow or aggressive intracranial AVFs is a safe and considerable treatment option, especially for those associated with large venous pouches that are challenging and relatively high-risk for TVE.
Keyword
Figure
Reference
-
References
1. Alturki AY, Enriquez-Marulanda A, Schmalz P, Ogilvy CS, Thomas AJ. Transarterial onyx embolization of bilateral transverse-sigmoid dural arteriovenous malformation with transvenous balloon assist-initial U.S. experience with copernic RC venous remodeling balloon. World Neurosurg. 109:398–402. 2018.
Article2. Baharvahdat H, Ooi YC, Kim WJ, Mowla A, Coon AL, Colby GP. Updates in the management of cranial dural arteriovenous fistula. Stroke Vasc Neurol. 5:50–58. 2019.
Article3. Bhattacharya JJ, Thammaroj J. Vein of galen malformations. J Neurol Neurosurg Psychiatry. 74 Suppl 1(Suppl 1):i42–i44. 2003.
Article4. Biondi A, Casasco A, Houdart E, Gioino C, Sourour N, Vivas E, et al. Evolution of angiographic signs of venous hypertension and clinical signs of intracranial hypertension in intracranial dural arteriovenous fistulas. J Neuroradiol. 26:49–58. 1999.5. Borden JA, Wu JK, Shucart WA. A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg. 82:166–179. 1995.
Article6. Cognard C, Gobin YP, Pierot L, Bailly AL, Houdart E, Casasco A, et al. Cerebral dural arteriovenous fistulas: clinical and angiographic correlation with a revised classification of venous drainage. Radiology. 194:671–680. 1995.
Article7. Cooke D, Tatum J, Farid H, Dowd C, Higashida R, Halbach V. Transvenous embolization of a pediatric pial arteriovenous fistula. J Neurointerv Surg. 4:e14. 2012.
Article8. Gandhi D, Chen J, Pearl M, Huang J, Gemmete JJ, Kathuria S. Intracranial dural arteriovenous fistulas: classification, imaging findings, and treatment. AJNR Am J Neuroradiol. 33:1007–1013. 2012.
Article9. Goel A, Jain S, Shah A, Rai S, Gore S, Dharurkar P. Pial arteriovenous fistula: a brief review and report of 14 surgically treated cases. World Neurosurg. 110:e873–e881. 2018.
Article10. Gonzalez LF, Chalouhi N, Jabbour P, Teufack S, Albuquerque FC, Spetzler RF. Rapid and progressive venous thrombosis after occlusion of high-flow arteriovenous fistula. World Neurosurg. 80:e359–e365. 2013.
Article11. Hetts SW, Keenan K, Fullerton HJ, Young WL, English JD, Gupta N, et al. Pediatric intracranial nongalenic pial arteriovenous fistulas: clinical features, angioarchitecture, and outcomes. AJNR Am J Neuroradiol. 33:1710–1719. 2012.
Article12. Hoh BL, Putman CM, Budzik RF, Ogilvy CS. Surgical and endovascular flow disconnection of intracranial pial single-channel arteriovenous fistulae. Neurosurgery. 49:1351–1363. discussion 1363-1364. 2001.
Article13. Jabbour P, Tjoumakaris S, Chalouhi N, Randazzo C, Gonzalez LF, Dumont A, et al. Endovascular treatment of cerebral dural and pial arteriovenous fistulas. Neuroimaging Clin N Am. 23:625–636. 2013.
Article14. Kirsch M, Henkes H, Liebig T, Weber W, Esser J, Golik S, et al. Endovascular management of dural carotid-cavernous sinus fistulas in 141 patients. Neuroradiology. 48:486–490. 2006.
Article15. Koebbe CJ, Singhal D, Sheehan J, Flickinger JC, Horowitz M, Kondziolka D, et al. Radiosurgery for dural arteriovenous fistulas. Surg Neurol. 64:392–398. discussion 398-399. 2005.
Article16. Kwon BJ, Han MH, Kang HS, Chang KH. MR imaging findings of intracranial dural arteriovenous fistulas: relations with venous drainage patterns. AJNR Am J Neuroradiol. 26:2500–2507. 2005.17. Lasjaunias P, Manelfe C, Chiu M. Angiographic architecture of intracranial vascular malformations and fistulas--pretherapeutic aspects. Neurosurg Rev. 9:253–263. 1986.
Article18. Lekkhong E, Pongpech S, Ter Brugge K, Jiarakongmun P, Willinsky R, Geibprasert S, et al. Transvenous embolization of intracranial dural arteriovenous shunts through occluded venous segments: experience in 51 Patients. AJNR Am J Neuroradiol. 32:1738–1744. 2011.
Article19. Liu CA, Chen HC, Luo CB, Guo WY, Mu-Huo Teng M, Chen HH, et al. Dural sinus malformation with arteriovenous fistulae in a newborn: positive outcome following endovascular management. J Chin Med Assoc. 75:43–46. 2012.
Article20. Lv X, Chen X, Ge H, He H, Jiang C, Li Y. Adjunct to embolize the high-flow fistula part of arteriovenous malformation using a double-lumen balloon catheter. World Neurosurg. 96:370–374. 2016.
Article21. Maejima R, Ohshima T, Miyachi S, Matsuo N, Kawaguchi R, Takayasu M. Neonatal intracranial pial arteriovenous fistula treated with endovascular embolization: a case report. World Neurosurg. 118:261–264. 2018.
Article22. Mohammed N, Hung YC, Xu Z, Starke RM, Kano H, Lee J, et al. A propensity score-matched cohort analysis of outcomes after stereotactic radiosurgery in older versus younger patients with dural arteriovenous fistula: an international multicenter study. World Neurosurg. 125:e1114–e1124. 2019.
Article23. Oh SH, Choi JH, Kim BS, Lee KS, Shin YS. Treatment outcomes according to various treatment modalities for intracranial dural arteriovenous fistulas in the onyx era: a 10-year single-center experience. World Neurosurg. 126:e825–e834. 2019.
Article24. Pan L, Wen JP, Ma LT. Differences between CS-DAVF and TCCF--to reveal and redefine CS-DAVF. Chin Neurosurg J. 4:26. 2018.
Article25. Qureshi AM, Bhatia K, Kostynskyy A, Krings T. Clinical and angioarchitectural features of ruptured dural arteriovenous fistulas. World Neurosurg. 147:e476–e481. 2021.
Article26. Viñuela F, Drake CG, Fox AJ, Pelz DM. Giant intracranial varices secondary to high-flow arteriovenous fistulae. J Neurosurg. 66:198–203. 1987.
Article27. Yang WH, Lu MS, Cheng YK, Wang TC. Pial arteriovenous fistula: a review of literature. Br J Neurosurg. 25:580–585. 2011.
Article28. Yuki I, Kim RH, Duckwiler G, Jahan R, Tateshima S, Gonzalez N, et al. Treatment of brain arteriovenous malformations with high-flow arteriovenous fistulas: risk and complications associated with endovascular embolization in multimodality treatment. Clinical article. J Neurosurg. 113:715–722. 2010.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ruptured Cerebral Arteriovenous Malformation with Giant Venous Aneurysm: Case Report
- A Case of Arteriovenous Malformation Harboring of Large Venous Aneurysm
- Embolization of Cerebral Pial Arteriovenous Fistula Under Balloon-assisted Flow Control Using NBCA: a Case Report
- Vein of Galen Aneurysmal Malformation: Treatment by Transarterial Venous Sac and Fistula Embolization Using Coils and Glue
- A Case of Pial Arteriovenous Fistula with Giant Venous Aneurysm and Multiple Varices Treated with Coil Embolization