J Cerebrovasc Endovasc Neurosurg.
2021 Dec;23(4):354-358. 10.7461/jcen.2021.E2021.01.003.
Extending the stroke treatment window beyond DAWN in patients with very slow progressor type collaterals: How far can we go?
- Affiliations
-
- 1Department of Interventional Neuroradiology Neuri Brain Vascular Center, Hopital Bicetre, APHP, Paris Sud Université, France
- 2Department of Interventional Neuroradiology, Hospital Estadual Central, Vitória–Espírito, Brazil
- 3Department of Neurology, Hopital Bicetre, APHP, Paris Sud Université, France
- 4Department of Neurology, Escola Superior de Ciências da Santa Casa de Misericórdia de Vitória, Hospital da Santa Casa de Vitória, Vitória ES, Brazil
- KMID: 2523894
- DOI: http://doi.org/10.7461/jcen.2021.E2021.01.003
Abstract
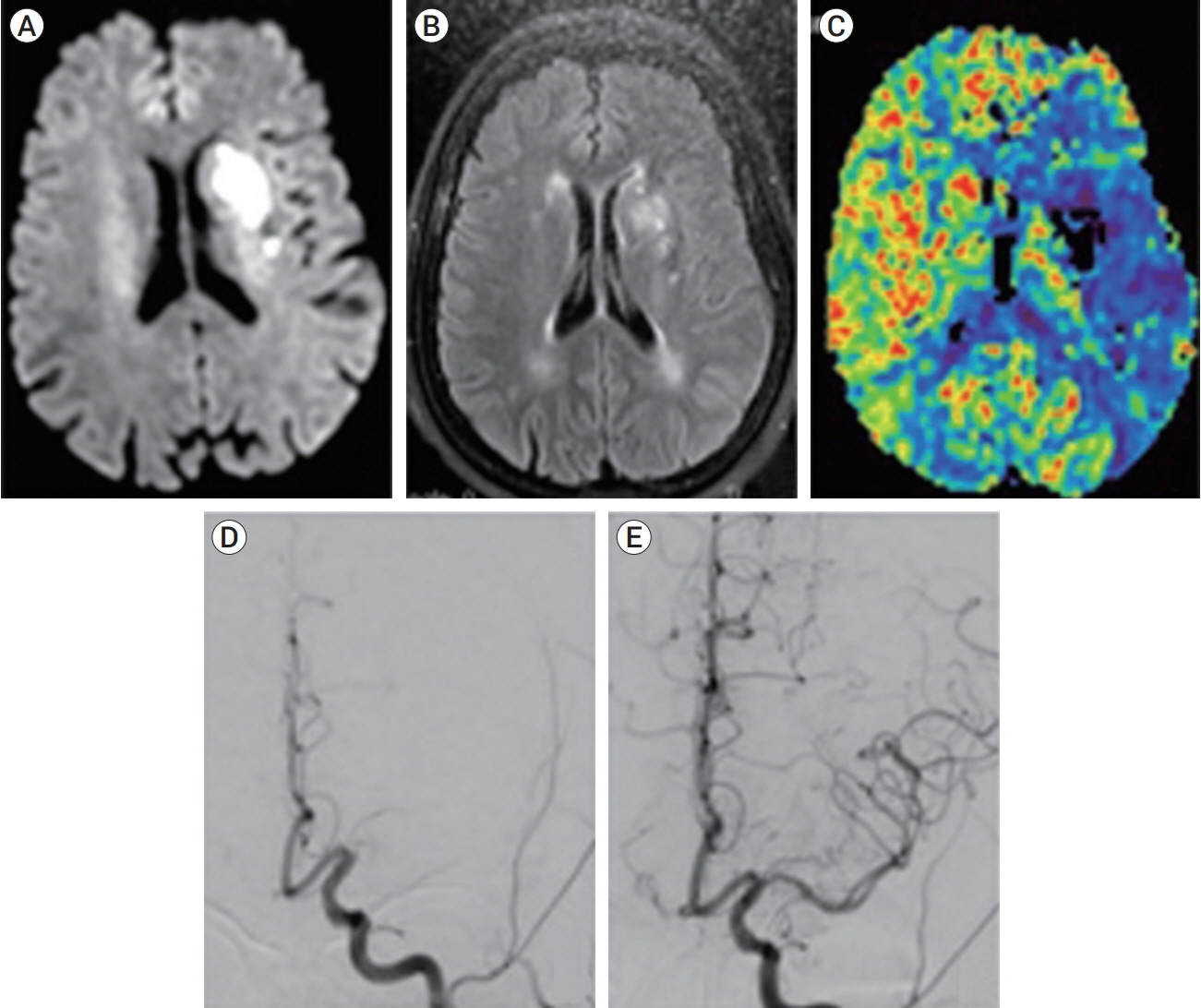
- Five trials published in 2015 showed the benefit of endovascular thrombectomy (ET) in patients with stroke and large vessel occlusion, extending the treatment window has become an obsession of all physicians. In 2018, the DAWN and DEFUSE-3 trials showed that, with careful selection of patients, the procedure could be carried out up to 24 hours after symptom onset with good outcomes. In addition, there have been cases where the DAWN criteria were met, and treatment occurred >24 hours after symptom onset. We present the case of a 68-year-old female whose groin puncture occurred 52 hours after the time last known well (TLKW), after neurological worsening of the initial situation, with a large mismatch ratio observed on magnetic resonance imaging, achieving TICI (the Thrombolysis in Cerebral Infarction scale) grade 3 recanalization. Five days after the procedure, the patient was discharged with NIHSS (National Institutes of Health Stroke Scale) score of 3. Some types of collateral circulation (slow progressors and “turtle” progressors, our term for very slow progressors) can extend the treatment window beyond 24 hours of the TLKW but can lead to a hyperperfusion-like syndrome immediately after the ET. Further studies are needed to evaluate the reproducibility of this hypothetical syndrome.
Figure
Reference
-
1. Aguilar-Salinas P, Santos R, Granja MF, Effendi S, Sauvageau E, Hanel R, et al. Revisiting the therapeutic time window dogma: successful thrombectomy 6 days after stroke onset. BMJ Case Reports. 2018; 2018:bcr-2018-014039.
Article2. Albers GW, Marks MP, Kemp S, Christensen S, Tsai JP, Ortega-Gutierrez S, et al. Thrombectomy for stroke at 6 to 16 hours with selection by perfusion imaging. N Engl J Med. 2018; Feb. 378(8):708–18.
Article3. Berkhemer OA, Fransen PSS, Beumer D, van den Berg LA, Lingsma HF, Yoo AJ, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med. 2015; Jan. 372(1):11–20.4. Campbell BCV, Mitchell PJ, Kleinig TJ, Dewey HM, Churilov L, Yassi L, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med. 2015; Mar. 372(11):1009–18.
Article5. Chu YT, Lee KP, Chen CH, Sung PS, Lin YH, Lee CW, et al. Contrast-induced encephalopathy after endovascular thrombectomy for acute ischemic stroke. Stroke. 2020; Dec. 51(21):3756–9.
Article6. Copen WA, Rezai Gharai L, Barak ER, Schwamm LH, Wu O, Kamalian S, et al. Existence of the diffusion-perfusion mismatch within 24 hours after onset of acute stroke: Dependence on proximal arterial occlusion. Radiology. 2009; Mar. 250(3):878–86.
Article7. Desai SM, Haussen DC, Aghaebrahim A, Al-Bayati AR, Santos R, Nogueira RG, et al. Thrombectomy 24 hours after stroke: Beyond DAWN. J Neurointerv Surg. 2018; Nov. 10(11):1039–42.
Article8. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 372:1019–30.9. Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008; Sep. 359(13):1317–29.
Article10. Jovin TG, Chamorro A, Cobo E, Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med. 2015; 372:2296–306.
Article11. Nogueira RG, Jadhav AP, Haussen DC, Bonafe A, Budzik RF, Bhuva P, et al. Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med. 2018; Jan. 378(1):11–21.12. Rocha M, Jovin TG. Fast versus slow progressors of infarct growth in large vessel occlusion stroke: clinical and research implications. Stroke. 2017; Sep. 48(9):2621–7.13. Saver JL, Goyal M, Bonafe A, Diener HC, Levy EI. Pereiraet VM, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med. 2015; Jun. 372(24):2285–95.14. So C, Chaudhry N, Gandhi D, Cole JW, Motta M. Endovascular thrombectomy in acute-onset ischemic stroke-beyond the standard time windows: A case report and a review of the literature. Case Rep Neurol. 2018; Sep. 10(3):279–85.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Imaging in Acute Anterior Circulation Ischemic Stroke: Current and Future
- An Update of Recent Guideline for the Endovascular Recanalization Therapy in Acute Ischemic Stroke
- The Clinical Benefit and Care Burden of Extending the Window of Endovascular Thrombectomy for Stroke in the Emergency Room
- Reperfusion therapy in acute ischemic stroke
- Impact of Slow Blood Filling via Collaterals on Infarct Growth: Comparison of Mismatch and Collateral Status