Ann Rehabil Med.
2021 Dec;45(6):431-439. 10.5535/arm.21068.
Peak Voluntary Cough Flow and Oropharyngeal Dysphagia as Risk Factors for Pneumonia
- Affiliations
-
- 1Department of Rehabilitation Medicine, Kangwon National University Hospital, Kangwon National University School of Medicine, Chuncheon, Korea
- KMID: 2523840
- DOI: http://doi.org/10.5535/arm.21068
Abstract
Objective
To investigate the relationship between voluntary peak cough flow (PCF), oropharyngeal dysphagia, and pneumonia in patients who were evaluated with videofluoroscopic swallowing study (VFSS).
Methods
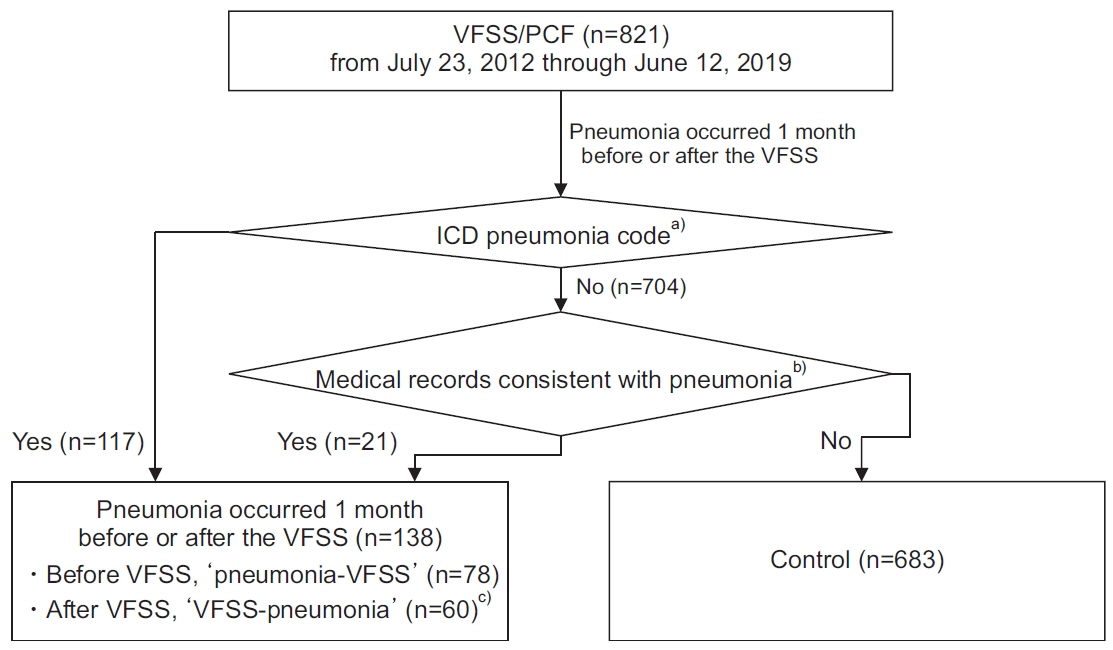
Patients who underwent both VFSS and PCF measurement on the same day were enrolled retrospectively (n=821). Pneumonia (n=138) and control (n=683) groups were assigned based on presence of pneumonia within 1 month from the date of VFSS assessment. In addition, sex, age (<65 and ≥65 years), preceding conditions, modified Barthel Index (MBI), Mini-Mental State Examination (MMSE), PCF value (<160, ≥160 and <270, and ≥270 L/min), and presence of aspiration/penetration on VFSS were reviewed.
Results
Pneumonia group was more likely to be male (n=108; 78.3%), ≥65 years (n=121; 87.7%), with neurodegenerative (n=25; 18.1%) or other miscellaneous diseases (n=50; 36.2%), and in poor functional level with lower value of MBI (39.1±26.59). However, MMSE was not significantly different in comparison to that of the control group. The pneumonia group was also more likely to have dysphagia (82.6%) and lower value of PCF (<160 L/min, 70.3%). In multivariable logistic regression analysis, male sex (odd ratio [OR]=6.62; 95% confidence interval [CI], 2.70–16.26), other miscellaneous diseases as preceding conditions (OR=2.52; 95% CI, 1.14–5.58), dysphagia (OR=3.82; 95% CI, 1.42–10.23), and PCF <160 L/min (OR=14.34; 95% CI, 1.84–111.60) were factors significantly related with pneumonia.
Conclusion
Impaired swallowing and coughing function showed an independent association with the development of pneumonia. Patients with PCF <160 L/min require more attention with lung care and should be encouraged with voluntary coughing strategy to prevent possible pulmonary complications.
Figure
Cited by 1 articles
-
Correlation Between Articulatory Diadochokinetic Parameters and Dysphagia Parameters in Subacute Stroke Patients
Back Min Oh, Hyun Seok, Sang-Hyun Kim, Seung Yeol Lee, Su Jung Park, Beom Jin Kim, Hyun Jung Kim
Ann Rehabil Med. 2023;47(3):192-204. doi: 10.5535/arm.23018.
Reference
-
1. Choi MJ, Song JY, Noh JY, Yoon JG, Lee SN, Heo JY, et al. Disease burden of hospitalized communityacquired pneumonia in South Korea: analysis based on age and underlying medical conditions. Medicine (Baltimore). 2017; 96:e8429.2. Loeb M, McGeer A, McArthur M, Walter S, Simor AE. Risk factors for pneumonia and other lower respiratory tract infections in elderly residents of long-term care facilities. Arch Intern Med. 1999; 159:2058–64.
Article3. Statistics Korea. The Annual Report on the Causes of Death Statistics 2019. Daejeon: Statistics Korea;2020.4. World Health Organization. The top 10 causes of death [Internet]. Geneva: World Health Organization;2020; [cited 2021 Nov 1]. Available from: https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death.5. Pikus L, Levine MS, Yang YX, Rubesin SE, Katzka DA, Laufer I, et al. Videofluoroscopic studies of swallowing dysfunction and the relative risk of pneumonia. AJR Am J Roentgenol. 2003; 180:1613–6.
Article6. Kulnik ST, Birring SS, Hodsoll J, Moxham J, Rafferty GF, Kalra L. Higher cough flow is associated with lower risk of pneumonia in acute stroke. Thorax. 2016; 71:474–5.
Article7. Tzani P, Chiesa S, Aiello M, Scarascia A, Catellani C, Elia D, et al. The value of cough peak flow in the assessment of cough efficacy in neuromuscular patients: a cross sectional study. Eur J Phys Rehabil Med. 2014; 50:427–32.8. Hammond CA, Goldstein LB, Horner RD, Ying J, Gray L, Gonzalez-Rothi L, et al. Predicting aspiration in patients with ischemic stroke: comparison of clinical signs and aerodynamic measures of voluntary cough. Chest. 2009; 135:769–77.9. Plowman EK, Watts SA, Robison R, Tabor L, Dion C, Gaziano J, et al. Voluntary cough airflow differentiates safe versus unsafe swallowing in amyotrophic lateral sclerosis. Dysphagia. 2016; 31:383–90.
Article10. Bianchi C, Baiardi P, Khirani S, Cantarella G. Cough peak flow as a predictor of pulmonary morbidity in patients with dysphagia. Am J Phys Med Rehabil. 2012; 91:783–8.
Article11. Jung HY, Park BK, Shin HS, Kang YK, Pyun SB, Paik NJ, et al. Development of the Korean version of Modified Barthel Index (K-MBI): multi-center study for subjects with stroke. J Korean Acad Rehabil Med. 2007; 31:283–97.12. Park JH, Kwon YC. Modification of the mini‐mental state examination for use in the elderly in a non‐western society. Part 1: development of Korean version of mini‐mental state examination. Int J Geriatr Psychiatry. 1990; 5:381–7.
Article13. Sahni AS, Wolfe L. Respiratory care in neuromuscular diseases. Respir Care. 2018; 63:601–8.
Article14. Rosenbek JC, Robbins JA, Roecker EB, Coyle JL, Wood JL. A penetration-aspiration scale. Dysphagia. 1996; 11:93–8.
Article15. Sakai Y, Ohira M, Yokokawa Y. Cough strength is an indicator of aspiration risk when restarting food intake in elderly subjects with community-acquired pneumonia. Respir Care. 2020; 65:169–76.
Article16. Manabe T, Teramoto S, Tamiya N, Okochi J, Hizawa N. Risk factors for aspiration pneumonia in older adults. PLoS One. 2015; 10:e0140060.
Article17. Marik PE, Kaplan D. Aspiration pneumonia and dysphagia in the elderly. Chest. 2003; 124:328–36.
Article18. van der Maarel-Wierink CD, Vanobbergen JN, Bronkhorst EM, Schols JM, de Baat C. Risk factors for aspiration pneumonia in frail older people: a systematic literature review. J Am Med Dir Assoc. 2011; 12:344–54.19. Langmore SE, Terpenning MS, Schork A, Chen Y, Murray JT, Lopatin D, et al. Predictors of aspiration pneumonia: how important is dysphagia? Dysphagia. 1998; 13:69–81.
Article20. Hammond CA, Goldstein LB. Cough and aspiration of food and liquids due to oral-pharyngeal dysphagia: ACCP evidence-based clinical practice guidelines. Chest. 2006; 129(1 Suppl):154S–168S.21. Min SW, Oh SH, Kim GC, Sim YJ, Kim DK, Jeong HJ. Clinical importance of peak cough flow in dysphagia evaluation of patients diagnosed with ischemic stroke. Ann Rehabil Med. 2018; 42:798–803.
Article22. Kimura Y, Takahashi M, Wada F, Hachisuka K. Differences in the peak cough flow among stroke patients with and without dysphagia. J UOEH. 2013; 35:9–16.
Article23. World Health Organization. WHO global report on trends in prevalence of tobacco use 2000-2025. 3rd ed. Geneva, Switzerland: World Health Organization;2019.24. Almirall J, Gonzalez CA, Balanzo X, Bolibar I. Proportion of community-acquired pneumonia cases attributable to tobacco smoking. Chest. 1999; 116:375–9.
Article25. Bello S, Menendez R, Antoni T, Reyes S, Zalacain R, Capelastegui A, et al. Tobacco smoking increases the risk for death from pneumococcal pneumonia. Chest. 2014; 146:1029–37.
Article26. World Health Organization. Global status report on alcohol and health 2018. Geneva, Switzerland: World Health Organization;2018.27. Koivula I, Sten M, Makela PH. Risk factors for pneumonia in the elderly. Am J Med. 1994; 96:313–20.
Article28. Lee SJ, Lee KW, Kim SB, Lee JH, Park MK. Voluntary cough and swallowing function characteristics of acute stroke patients based on lesion type. Arch Phys Med Rehabil. 2015; 96:1866–72.
Article29. Burkhardt C, Neuwirth C, Sommacal A, Andersen PM, Weber M. Is survival improved by the use of NIV and PEG in amyotrophic lateral sclerosis (ALS)? A post-mortem study of 80 ALS patients. PLoS One. 2017; 12:e0177555.
Article30. Anderson KK, Arnold PM. Oropharyngeal dysphagia after anterior cervical spine surgery: a review. Global Spine J. 2013; 3:273–86.
Article31. Son YR, Choi KH, Kim TG. Dysphagia in tongue cancer patients. Ann Rehabil Med. 2015; 39:210–7.
Article32. Astudillo L, Peron JM, Sailler L, Danjoux M, RigalHuguet F, Arlet-Suau E. Dysphagia revealing esophageal involvement by non-Hodgkin’s lymphoma. Ann Hematol. 2005; 84:482–3.
Article33. Moverare T, Lohmander A, Hultcrantz M, Sjogreen L. Peripheral facial palsy: speech, communication and oral motor function. Eur Ann Otorhinolaryngol Head Neck Dis. 2017; 134:27–31.34. Ha JF. Unilateral vocal fold palsy & dysphagia: a review. Auris Nasus Larynx. 2020; 47:315–34.35. Almirall J, Rofes L, Serra-Prat M, Icart R, Palomera E, Arreola V, et al. Oropharyngeal dysphagia is a risk factor for community-acquired pneumonia in the elderly. Eur Respir J. 2013; 41:923–8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Oropharyngeal Cancer and Dysphagia
- Dysphagia Due to Bilateral Facial Palsy in B-Cell Acute Lymphoblastic Leukemia: A Case Report
- Clinical Importance of Peak Cough Flow in Dysphagia Evaluation of Patients Diagnosed With Ischemic Stroke
- Improvement of Peak Cough Flow After the Application of a Mechanical In-exsufflator in Patients With Neuromuscular Disease and Pneumonia: A Pilot Study
- Oropharyngeal Dysphagia in the Elderly