J Korean Med Sci.
2021 Dec;36(47):e320. 10.3346/jkms.2021.36.e320.
Epidemiology of Macrosomia in Korea: Growth and Development
- Affiliations
-
- 1Department of Pediatrics, Kangwon National University Hospital, Chuncheon, Korea
- 2Department of Pediatrics, Yonsei University College of Medicine, Seoul, Korea
- 3Department of Pediatrics, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- KMID: 2523240
- DOI: http://doi.org/10.3346/jkms.2021.36.e320
Abstract
- Background
Macrosomia, as an infant with birth weight over 4 kg, can have several perinatal, and neonatal complications. This study aimed to estimate the incidence of macrosomia in Korea and to identify the growth and developmental outcomes and other neonatal complications.
Methods
In total, 397,203 infants who were born in 2013 with birth weight ≥ 2.5 kg and who underwent infant health check-up between their 1 st and 7 th visit were included from the National Health Insurance Service database. The information was obtained by the International Classification of Diseases-10 codes or self-reported questionnaires in the National Health Screening Program.
Results
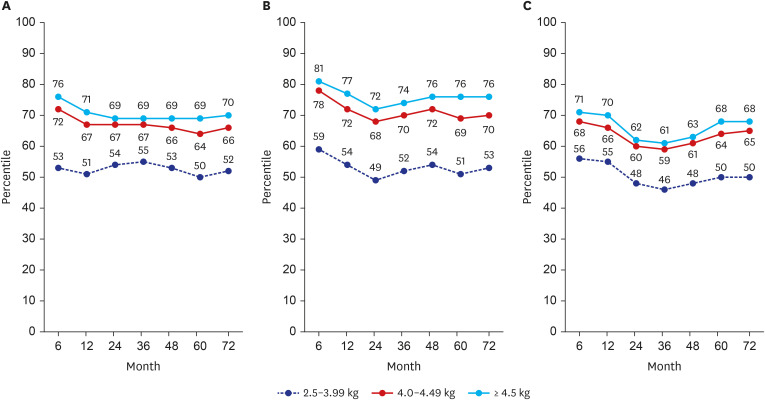
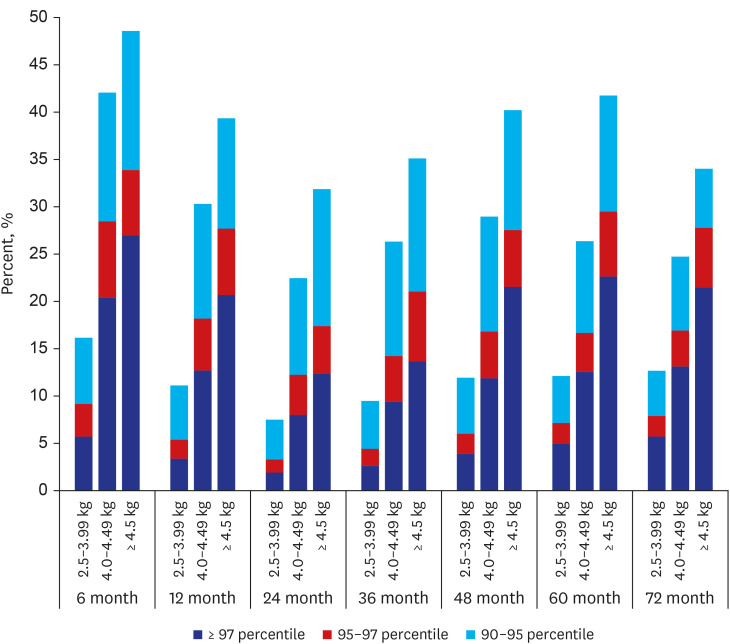
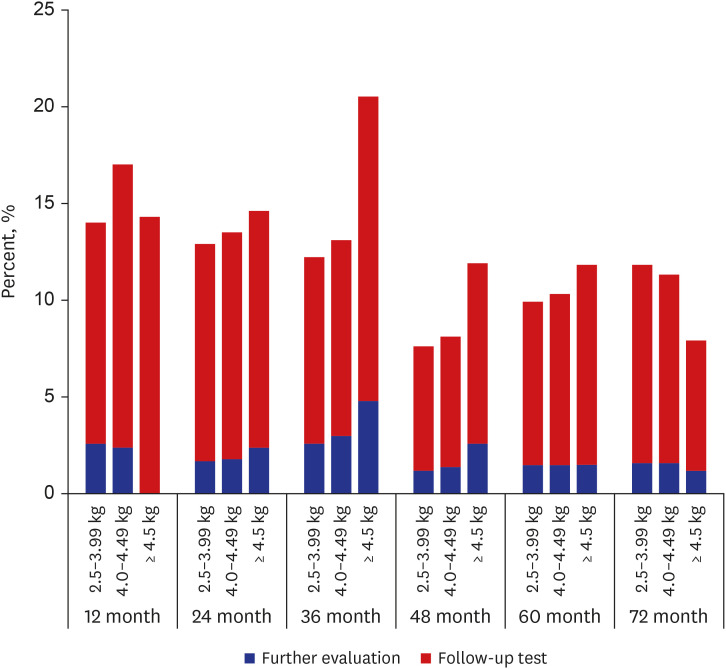
The distribution of infants by birth weight was as follows: 384,181 (97%) infants in the 2.5–3.99 kg (reference) group, 12,016 (3%) infants in the 4.0–4.49 kg group, 772 (0.2%) infants in the 4.5–4.99 kg group, and 78 (0.02%) infants in the ≥ 5 kg group. Macrosomia showed significantly higher incidence of sepsis, male sex, and mothers with GDM and birth injury. There was a significant difference in weight, height, and head circumference according to age, birth weight group, and combination of age and birth weight, respectively (P < 0.001). The number of infants with the weight above the 90 th percentile in macrosomia at each health check-up showed higher incidence than in reference group. The mean body mass index significantly differed among the groups, as 50.6 in infants with 2.5–3.99 kg of birth weight, 63.5 with 4.0–4.49 kg, 71.0 with 4.5–4.99 kg, and 73.1 with ≥ 5 kg. There was a significant difference in the incidence of poor developmental results between infants with macrosomia and the reference group at 24, 36 and 48 month of age.
Conclusion
Macrosomia was significantly associated with the risk of sepsis, birth injury, obesity and developmental problem especially in a boy born from mothers with gestational diabetes mellitus. Careful monitoring and proper strategies for monitoring growth and development are needed.
Keyword
Figure
Reference
-
1. Bae CW. Neonatal Epidemiology in Korea: Statistics and Clinical Treatment. Seoul, Korea: Shinheung Medscience;2012.2. Kang BH, Moon JY, Chung SH, Choi YS, Lee KS, Chang JY, et al. Birth statistics of high birth weight infants (macrosomia) in Korea. Korean J Pediatr. 2012; 55(8):280–285. PMID: 22977440.
Article3. Statistics Korea. Population trend survey. Updated 2021. Accessed April 21, 2021. https://kosis.kr/statHtml/statHtml.do?orgId=101&tblId=DT_1B80A04&conn_path=I3 .4. Henriksen T. The macrosomic fetus: a challenge in current obstetrics. Acta Obstet Gynecol Scand. 2008; 87(2):134–145. PMID: 18231880.
Article5. Langer O. Fetal macrosomia: etiologic factors. Clin Obstet Gynecol. 2000; 43(2):283–297. PMID: 10863626.
Article6. Bérard J, Dufour P, Vinatier D, Subtil D, Vanderstichèle S, Monnier JC, et al. Fetal macrosomia: risk factors and outcome. A study of the outcome concerning 100 cases >4500 g. Eur J Obstet Gynecol Reprod Biol. 1998; 77(1):51–59. PMID: 9550201.7. Optum. ICD-10-CM. The Complete Official Draft Code Set 2015. Salt Lake City, UT, USA: Optum;2014.8. AAPC. Updated 2015. Accessed April 8, 2021. http://news.aapc.com/ipps-rule-sets-i-10-date-for-2015/ .9. Eun BL. Standardization and Validity Reevaluation of the Korean Developmental Screening Test for Infants & Children. Cheongju, Korea: Korea Centers for Disease Control and Prevention;2017.10. Hwang JS. Neonate born to diabetic mother. Korean J Perinatol. 2006; 17(3):241–246.11. Cho AR, Kyeung KS, Park MA, Lee YM, Jeong EH. Risk factors of gestational diabetes mellitus. Korean J Perinatol. 2007; 18(4):329–337.12. Wollschlaeger K, Nieder J, Köppe I, Härtlein K. A study of fetal macrosomia. Arch Gynecol Obstet. 1999; 263(1-2):51–55. PMID: 10728630.
Article13. Beta J, Khan N, Fiolna M, Khalil A, Ramadan G, Akolekar R. Maternal and neonatal complications of fetal macrosomia: cohort study. Ultrasound Obstet Gynecol. 2019; 54(3):319–325. PMID: 30938000.
Article14. Boulet SL, Alexander GR, Salihu HM, Pass M. Macrosomic births in the united states: determinants, outcomes, and proposed grades of risk. Am J Obstet Gynecol. 2003; 188(5):1372–1378. PMID: 12748514.
Article15. Taal HR, Vd Heijden AJ, Steegers EA, Hofman A, Jaddoe VW. Small and large size for gestational age at birth, infant growth, and childhood overweight. Obesity (Silver Spring). 2013; 21(6):1261–1268. PMID: 23666877.
Article16. Gong YH, Ji CY, Shan JP. A longitudinal study on the catch-up growth of preterm and term infants of low, appropriate, and high birth weight. Asia Pac J Public Health. 2015; 27(2):NP1421–NP1431. PMID: 23695540.
Article17. Peters JT, Woelfle J, Joergens S, Schreiner F, Bartmann P, Gohlke B. Effect of post-natal catch-down and feeding practices on auxology, body composition and muscle function in children born large-for-gestational-age. J Diabetes Metab. 2017; 8(9):1–6.
Article18. Schellong K, Schulz S, Harder T, Plagemann A. Birth weight and long-term overweight risk: systematic review and a meta-analysis including 643,902 persons from 66 studies and 26 countries globally. PLoS One. 2012; 7(10):e47776. PMID: 23082214.
Article19. Simmonds M, Burch J, Llewellyn A, Griffiths C, Yang H, Owen C, et al. The use of measures of obesity in childhood for predicting obesity and the development of obesity-related diseases in adulthood: a systematic review and meta-analysis. Health Technol Assess. 2015; 19(43):1–336.
Article20. Deng JR, Tan WQ, Yang SY, Ao LP, Liang JP, Li LX, et al. High birth weight and its interaction with physical activity influence the risk of obesity in early school-aged children. World J Pediatr. 2020; 16(4):385–392. PMID: 32100262.
Article21. Oldroyd J, Renzaho A, Skouteris H. Low and high birth weight as risk factors for obesity among 4 to 5-year-old Australian children: does gender matter? Eur J Pediatr. 2011; 170(7):899–906. PMID: 21174121.
Article22. Boulet SL, Alexander GR, Salihu HM, Pass M. Macrosomic births in the united states: determinants, outcomes, and proposed grades of risk. Am J Obstet Gynecol. 2003; 188(5):1372–1378. PMID: 12748514.
Article23. Brilli Y, Restrepo BJ. Birth weight, neonatal care, and infant mortality: Evidence from macrosomic babies. Econ Hum Biol. 2020; 37:100825. PMID: 32028210.
Article24. Kristensen P, Keyes KM, Susser E, Corbett K, Mehlum IS, Irgens LM. High birth weight and perinatal mortality among siblings: a register based study in Norway, 1967-2011. PLoS One. 2017; 12(2):e0172891. PMID: 28245262.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Postpartum 75g Oral Glucose Tolerance Test in Mothers of Macrosimia
- Analysis of the Incidence of Macrosomia in Japan by Parental Nationalities at 5-year Intervals From 1995 to 2020
- Clinical survey of fetal macrosomia
- Cohen–Gibson syndrome in a family: The first familial case report
- Clinical Survey of Fetal Macrosomia