J Korean Med Sci.
2021 Dec;36(47):e310. 10.3346/jkms.2021.36.e310.
A Multicenter Study of Real-world Practice for Management of Abnormal Liver Function Tests in Children with Acute Infectious Diseases
- Affiliations
-
- 1Department of Pediatrics, Korea University Medical Center Anam Hospital, Seoul, Korea
- 2Department of Pediatrics, Chung-Ang University Hospital, College of Medicine, Chung-Ang University, Seoul, Korea
- 3Department of Pediatrics, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of medicine, Bucheon, Korea
- 4Department of Pediatrics, Kosin Gospel Hospital, Kosin University College of Medicine, Busan, Korea
- 5Department of Pediatrics, Haeundae Paik Hospital, Inje University College of Medicine, Busan, Korea
- 6Department of Pediatrics, Inje University Ilsan Paik Hospital, Goyang, Korea
- 7Department of Pediatrics, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Chuncheon, Korea
- KMID: 2523236
- DOI: http://doi.org/10.3346/jkms.2021.36.e310
Abstract
- Background
Abnormal liver function tests (LFTs) are commonly seen in pediatric patients with acute infectious diseases. Few studies and no definite clinical guidelines for these conditions are available. The present study aimed to elucidate the causes and factors associated with prolongation of liver enzyme elevation. We also investigated actual real-world practices in Korea.
Methods
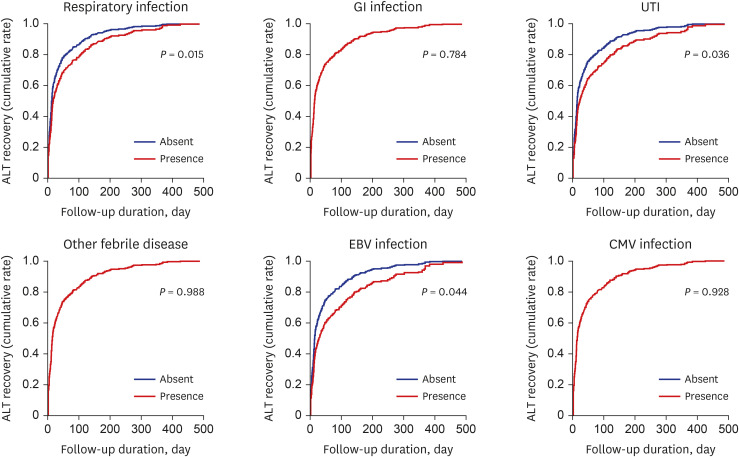
A retrospective study was performed on all patients younger than 18 years, who visited six tertiary teaching hospitals around Korea in 2018 for acute infectious diseases and showed alanine aminotransferase (ALT) levels above 60 IU/L without other specific conditions that could cause ALT elevation. We categorized the infections that cause LFT elevation into six groups: respiratory infection, gastrointestinal infection, urinary tract infection, other febrile disease, Epstein-Barr virus infection, and cytomegalovirus infection. We collected data on the medical specialty of the attending physician who followed up the subject, follow-up duration, percentage of follow-up loss, and their investigation.
Results
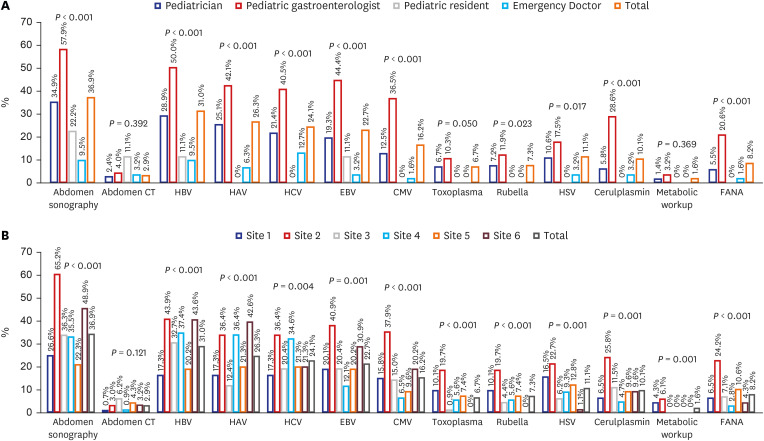
A total of 613 patients were enrolled in this study, half of whom (50.7%) were younger than 12 months. The mean initial aspartate aminotransferase and ALT values were 171.2 ± 274.1 and 194.9 ± 316.1 IU/L (range 23–2,881, 60–2,949 IU/L), respectively; however, other LFTs were within the normal range. Respiratory infection was the most common diagnosis (45.0%), and rhinovirus was the most commonly identified pathogen (9.8%). The follow-up rate was higher with pediatric gastroenterologists (90.5%) and non-gastroenterology pediatricians (76.4%) than with pediatric residents and emergency doctors. Older age was related to better ALT recovery (odds ratio [OR] of age for month = 1.003; 95% confidence interval [CI], 1.001–1.004; P = 0.004), while the number of infection episodes (OR = 0.626; 95% CI, 0.505–0.777; P < 0.001) was associated with poor ALT recovery. Abdominal sonography was the most commonly used diagnostic tool (36.9%), followed by the hepatotropic virus workup. The modalities of hepatitis workup were significantly differently applied by physicians based on their specialties and institutions.
Conclusion
Abnormal liver function test after a systemic infection was common in respiratory infection and under the age of 1 year. Age, number of infections, and initial results of LFTs were related to ALT recovery time. Inter-physician, inter-institution, and inter-specialty variances were observed in real-world practice.
Figure
Cited by 1 articles
-
A Report on a Nationwide Surveillance System for Pediatric Acute Hepatitis of Unknown Etiology in Korea
Kyung Jae Lee, Jae Sung Ko, Kie Young Park, Ki Soo Kang, Kunsong Lee, Jeana Hong, Soon Chul Kim, Yoon Lee, Ben Kang, Yu Bin Kim, Hyun Jin Kim, Byung Wook Eun, Hye-Kyung Cho, Yae-Jean Kim, Mi Jin Kim, Jin Lee, Taek-Jin Lee, Seak Hee Oh, Sowon Park, Eun Ha Hwang, Sangjun Sohn, Jin Gyu Lim, YooJin Kim, Yeoun Joo Lee
J Korean Med Sci. 2023;38(47):e401. doi: 10.3346/jkms.2023.38.e401.
Reference
-
1. Minemura M, Tajiri K, Shimizu Y. Liver involvement in systemic infection. World J Hepatol. 2014; 6(9):632–642. PMID: 25276279.
Article2. Jang M, Oh MS, Oh SC, Kang KS. Distribution of diseases causing liver function test abnormality in children and natural recovery time of the abnormal liver function. J Korean Med Sci. 2016; 31(11):1784–1789. PMID: 27709857.
Article3. Schaffner F, Popper H. Nonspecific reactive hepatitis in aged and infirm people. Am J Dig Dis. 1959; 4(5):389–399. PMID: 13649645.
Article4. Kim TS, Hur TH, Lim SJ, Bin JH, Hahn SH, Kim SY, et al. A rise and fall in AST and ALT level in nonspecific reactive hepatitis. Clin Exp Pediatr. 2008; 51(4):396–400.
Article5. Kim JW, Lee KJ, Yang HR, Chang JY, Moon JS, Khang YH, et al. Prevalence and risk factors of elevated alanine aminotransferase among Korean adolescents: 2001–2014. BMC Public Health. 2018; 18(1):617. PMID: 29751750.
Article6. Park SH, Park HY, Kang JW, Park J, Shin KJ. Aminotransferase upper reference limits and the prevalence of elevated aminotransferases in the Korean adolescent population. J Pediatr Gastroenterol Nutr. 2012; 55(6):668–672. PMID: 22744190.
Article7. Kang Y, Park S, Kim S, Koh H. Estimated prevalence of adolescents with nonalcoholic fatty liver disease in Korea. J Korean Med Sci. 2018; 33(14):e109. PMID: 29607635.
Article8. Korea Disease Control and Prevention Agency. Infectious Diseases Surveillance Yearbook 2019. Cheongju, Korea: Korea Disease Control and Prevention Agency;2020.9. Cui HJ, Tong XL, Li P, Hao YX, Chen XG, Li AG, et al. Serum hepatic enzyme manifestations in patients with severe acute respiratory syndrome: retrospective analysis. World J Gastroenterol. 2004; 10(11):1652–1655. PMID: 15162543.
Article10. Matoq A, Salahuddin A. Acute hepatitis and pancytopenia in healthy infant with adenovirus. Case Rep Pediatr. 2016; 2016:8648190. PMID: 27340581.
Article11. Oh JS, Choi JS, Lee YH, Ko KO, Lim JW, Cheon EJ, et al. The relationships between respiratory virus infection and aminotransferase in children. Pediatr Gastroenterol Hepatol Nutr. 2016; 19(4):243–250. PMID: 28090469.
Article12. Polakos NK, Cornejo JC, Murray DA, Wright KO, Treanor JJ, Crispe IN, et al. Kupffer cell-dependent hepatitis occurs during influenza infection. Am J Pathol. 2006; 168(4):1169–1178. PMID: 16565492.
Article13. Alhammadi AH, Hendaus MA, Kayoum AA. Alteration of liver function due to H1N1 infection: a case report. Clin Exp Gastroenterol. 2013; 6:173–175. PMID: 24068870.
Article14. Eisenhut M, Thorburn K, Ahmed T. Transaminase levels in ventilated children with respiratory syncytial virus bronchiolitis. Intensive Care Med. 2004; 30(5):931–934. PMID: 15024569.
Article15. Kucuk O, Ugras M, Biçer S, Çöl D, Giray T, Erdag GC, et al. Hypertransaminasaemia in children with viral gastroenteritis. Infez Med. 2016; 24(1):32–37. PMID: 27031894.16. Park JY, Ko KO, Lim JW, Cheon EJ, Yoon JM. Increase in aminotransferase levels during urinary tract infections in children. Pediatr Gastroenterol Hepatol Nutr. 2013; 16(2):89–94. PMID: 24010112.
Article17. Pastor CM, Billiar TR, Losser MR, Payen DM. Liver injury during sepsis. J Crit Care. 1995; 10(4):183–197. PMID: 8924968.
Article18. Szabo G, Romics L Jr, Frendl G. Liver in sepsis and systemic inflammatory response syndrome. Clin Liver Dis. 2002; 6(4):1045–1066. PMID: 12516206.
Article19. Bechini A, Levi M, Falla A, Ahmad A, Veldhuijzen I, Tiscione E, et al. The role of the general practitioner in the screening and clinical management of chronic viral hepatitis in six EU countries. J Prev Med Hyg. 2016; 57(2):E51–E60. PMID: 27582629.20. Gladman LM, Gorard DA. General practitioner and hospital specialist attitudes to functional gastrointestinal disorders. Aliment Pharmacol Ther. 2003; 17(5):651–654. PMID: 12641513.
Article21. Tatlow-Golden M, Prihodova L, Gavin B, Cullen W, McNicholas F. What do general practitioners know about ADHD? Attitudes and knowledge among first-contact gatekeepers: systematic narrative review. BMC Fam Pract. 2016; 17(1):129. PMID: 27605006.
Article22. Burton BK. Inborn errors of metabolism in infancy: a guide to diagnosis. Pediatrics. 1998; 102(6):E69. PMID: 9832597.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Diagnostic Approach to Abnormal Liver Function Tests in Asymptomatic Patients
- Ultrasonographic evaluation of patients with abnormal liver function tests in the emergency department
- A Case of Infectious Mononucleosis
- Allopurinol Induced Abnormalities of Liver Function Test in Gout Patients
- Distribution of Diseases Causing Liver Function Test Abnormality in Children and Natural Recovery Time of the Abnormal Liver Function