Nutr Res Pract.
2021 Dec;15(6):703-714. 10.4162/nrp.2021.15.6.703.
Effects of a low-FODMAP enteral formula on diarrhea on patients in the intensive care unit
- Affiliations
-
- 1Department of Food and Nutrition, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam 13496, Korea
- 2Department of Medical Nutrition, Kyung Hee University, Yongin 17104, Korea
- 3Department of Neurosurgery, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam 13496, Korea
- 4Division of Pulmonology, Allergy, and Critical Care Medicine, Department of Internal Medicine, CHA Bundang Medical Center, School of Medicine, CHA University, Seongnam 13496, Korea
- 5Department of Pharmacy, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam 13496, Korea
- 6Department of Nursing, CHA Bundang Medical Center, CHA University School of Medicine, Seongnam 13496, Korea
- KMID: 2522651
- DOI: http://doi.org/10.4162/nrp.2021.15.6.703
Abstract
- BACKGROUND/OBJECTIVES
A dietary restriction on the intake of fermentable oligosaccharides, disaccharides, monosaccharides, and polyols (FODMAPs) has been reported to be effective in the treatment of gastrointestinal (GI) tract complications. Enteral nutrition (EN) is widely used for patients who cannot obtain their nutritional requirements orally, but many studies have reported EN complications, especially diarrhea, in up to 50% of patients.
SUBJECTS/METHODS
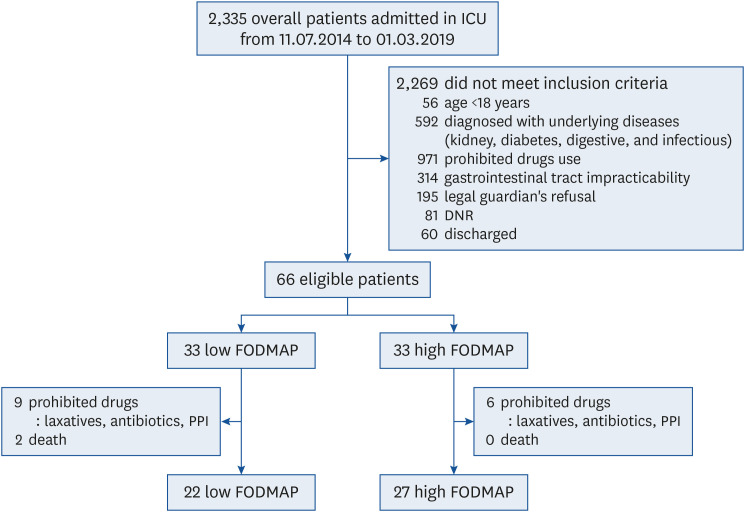
We performed a single-center, non-randomized, controlled trial to determine the effects of a low-FODMAP enteral formula on GI complications in patients in intensive care units (ICUs). Patients in the ICU who needed EN (n = 66) were alternately assigned to the low-FODMAP group (n = 33) or the high-FODMAP group (n = 33).
RESULTS
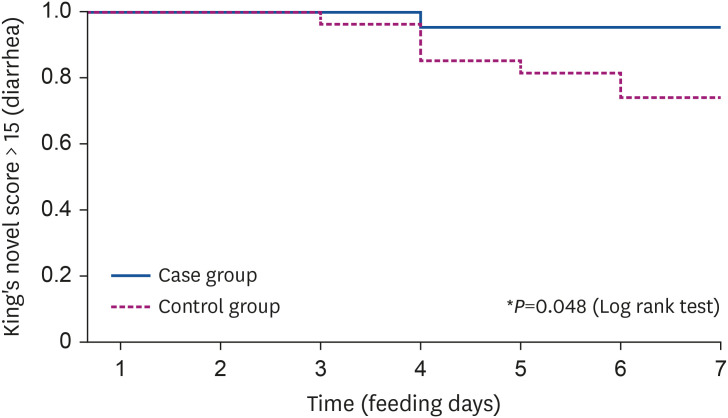
Anthropometric and biochemical parameters were measured, and stool assessment was performed using King's Stool Chart. We excluded patients who received laxatives, GI motility agents, proton pump inhibitors, antifungal agents, and antibiotics other than β-lactams. There were no differences in GI symptoms during 7 days of intervention, including bowel sound, abdominal distension, and vomiting between the 2 groups. However, diarrhea was more frequent in the high-FODMAP group (7/33 patients) than the lowFODMAP group (1/33 patients) (P = 0.044).
CONCLUSIONS
Our results suggest that a low-FODMAP enteral formula may be a practical therapeutic approach for patients who exhibit enteral formula complications. Our study warrants further randomized clinical trials and multicenter trials.
Keyword
Figure
Reference
-
1. Heyland DK, Schroter-Noppe D, Drover JW, Jain M, Keefe L, Dhaliwal R, Day A. Nutrition support in the critical care setting: current practice in canadian ICUs--opportunities for improvement? JPEN J Parenter Enteral Nutr. 2003; 27:74–83. PMID: 12549603.
Article2. Kreymann KG, Berger MM, Deutz NE, Hiesmayr M, Jolliet P, Kazandjiev G, Nitenberg G, van den Berghe G, Wernerman J, Ebner C, Hartl W, Heymann C, Spies C. DGEM (German Society for Nutritional Medicine). ESPEN (European Society for Parenteral and Enteral Nutrition). ESPEN guidelines on enteral nutrition: intensive care. Clin Nutr. 2006; 25:210–223. PMID: 16697087.
Article3. Heyland DK, Konopad E, Alberda C, Keefe L, Cooper C, Cantwell B. How well do critically ill patients tolerate early, intragastric enteral feeding? Results of a prospective, multicenter trial. Nutr Clin Pract. 1999; 14:23–28.
Article4. Whelan K. Enteral-tube-feeding diarrhoea: manipulating the colonic microbiota with probiotics and prebiotics. Proc Nutr Soc. 2007; 66:299–306. PMID: 17637081.
Article5. Pesola GR, Hogg JE, Eissa N, Matthews DE, Carlon GC. Hypertonic nasogastric tube feedings: do they cause diarrhea? Crit Care Med. 1990; 18:1378–1382. PMID: 2123143.6. Barrett JS, Shepherd SJ, Gibson PR. Strategies to manage gastrointestinal symptoms complicating enteral feeding. JPEN J Parenter Enteral Nutr. 2009; 33:21–26. PMID: 19028933.
Article7. van Tilburg MA, Felix CT. Diet and functional abdominal pain in children and adolescents. J Pediatr Gastroenterol Nutr. 2013; 57:141–148. PMID: 23698023.
Article8. Staudacher HM, Whelan K, Irving PM, Lomer MC. Comparison of symptom response following advice for a diet low in fermentable carbohydrates (FODMAPs) versus standard dietary advice in patients with irritable bowel syndrome. J Hum Nutr Diet. 2011; 24:487–495. PMID: 21615553.
Article9. de Roest RH, Dobbs BR, Chapman BA, Batman B, O'Brien LA, Leeper JA, Hebblethwaite CR, Gearry RB. The low FODMAP diet improves gastrointestinal symptoms in patients with irritable bowel syndrome: a prospective study. Int J Clin Pract. 2013; 67:895–903. PMID: 23701141.
Article10. Halmos EP, Power VA, Shepherd SJ, Gibson PR, Muir JG. A diet low in FODMAPs reduces symptoms of irritable bowel syndrome. Gastroenterology. 2014; 146:67–75.e5. PMID: 24076059.11. Barrett JS, Gearry RB, Muir JG, Irving PM, Rose R, Rosella O, Haines ML, Shepherd SJ, Gibson PR. Dietary poorly absorbed, short-chain carbohydrates increase delivery of water and fermentable substrates to the proximal colon. Aliment Pharmacol Ther. 2010; 31:874–882. PMID: 20102355.
Article12. Ong DK, Mitchell SB, Barrett JS, Shepherd SJ, Irving PM, Biesiekierski JR, Smith S, Gibson PR, Muir JG. Manipulation of dietary short chain carbohydrates alters the pattern of gas production and genesis of symptoms in irritable bowel syndrome. J Gastroenterol Hepatol. 2010; 25:1366–1373. PMID: 20659225.
Article13. Halmos EP, Muir JG, Barrett JS, Deng M, Shepherd SJ, Gibson PR. Diarrhoea during enteral nutrition is predicted by the poorly absorbed short-chain carbohydrate (FODMAP) content of the formula. Aliment Pharmacol Ther. 2010; 32:925–933. PMID: 20670219.
Article14. Chang SJ, Huang HH. Diarrhea in enterally fed patients: blame the diet? Curr Opin Clin Nutr Metab Care. 2013; 16:588–594. PMID: 23799327.15. Cho MR, Lee JS, Kim MC. Effects of fiber in enteral formula on stool frequency. J Korean Soc Parenter Enter Nutr. 2013; 5:31–35.
Article16. Lee H. Practical guidelines for enteral nutrition support. J Neurocrit Care. 2010; 3:115–117.17. Harris S, Naina HV, Kuppachi S. Look, feel, listen or look, listen, feel? Am J Med. 2007; 120:e3.
Article18. Whelan K, Judd PA, Taylor MA. Assessment of fecal output in patients receiving enteral tube feeding: validation of a novel chart. Eur J Clin Nutr. 2004; 58:1030–1037. PMID: 15220945.
Article19. Oudemans-van Straaten HM, Bosman RJ, Treskes M, van der Spoel HJ, Zandstra DF. Plasma glutamine depletion and patient outcome in acute ICU admissions. Intensive Care Med. 2001; 27:84–90. PMID: 11280678.
Article20. Reintam A, Parm P, Kitus R, Kern H, Starkopf J. Gastrointestinal symptoms in intensive care patients. Acta Anaesthesiol Scand. 2009; 53:318–324. PMID: 19243317.
Article21. Mentec H, Dupont H, Bocchetti M, Cani P, Ponche F, Bleichner G. Upper digestive intolerance during enteral nutrition in critically ill patients: frequency, risk factors, and complications. Crit Care Med. 2001; 29:1955–1961. PMID: 11588461.
Article22. Whelan K, Judd PA, Preedy VR, Taylor MA. Enteral feeding: the effect on faecal output, the faecal microflora and SCFA concentrations. Proc Nutr Soc. 2004; 63:105–113. PMID: 15099408.
Article23. Dorman BP, Hill C, McGrath M, Mansour A, Dobson D, Pearse T, Singleton J, Al-Omoush A, Barry M, Colongon AR, Perez M, Fitzgerald D, Zabala M. Bowel management in the intensive care unit. Intensive Crit Care Nurs. 2004; 20:320–329. PMID: 15567673.
Article24. Mueller CM. The ASPEN Adult Nutrition Support Core Curriculum. Silver Spring (MD): American Society for Parenteral and Enteral Nutrition;2017. p. 230–231. p. 26825. Thorson MA, Bliss DZ, Savik K. Re-examination of risk factors for non-Clostridium difficile-associated diarrhoea in hospitalized patients. J Adv Nurs. 2008; 62:354–364. PMID: 18426460.
Article26. Homann HH, Kemen M, Fuessenich C, Senkal M, Zumtobel V. Reduction in diarrhea incidence by soluble fiber in patients receiving total or supplemental enteral nutrition. JPEN J Parenter Enteral Nutr. 1994; 18:486–490. PMID: 7602722.
Article27. Spapen H, Diltoer M, Van Malderen C, Opdenacker G, Suys E, Huyghens L. Soluble fiber reduces the incidence of diarrhea in septic patients receiving total enteral nutrition: a prospective, double-blind, randomized, and controlled trial. Clin Nutr. 2001; 20:301–305. PMID: 11478826.
Article28. Nakao M, Ogura Y, Satake S, Ito I, Iguchi A, Takagi K, Nabeshima T. Usefulness of soluble dietary fiber for the treatment of diarrhea during enteral nutrition in elderly patients. Nutrition. 2002; 18:35–39. PMID: 11827762.
Article29. Yoon SR, Lee JH, Lee JH, Na GY, Lee KH, Lee YB, Jung GH, Kim OY. Low-FODMAP formula improves diarrhea and nutritional status in hospitalized patients receiving enteral nutrition: a randomized, multicenter, double-blind clinical trial. Nutr J. 2015; 14:116. PMID: 26530312.
Article30. Trabal J, Leyes P, Hervás S, Herrera M, de Talló Forga M. Factors associated with nosocomial diarrhea in patients with enteral tube feeding. Nutr Hosp. 2008; 23:500–504. PMID: 19160901.31. AlKhawaja S. Diarrhea in critically Ill patient. EC Nutr. 2017; 9:105–115.32. Lewis K, Alqahtani Z, Mcintyre L, Almenawer S, Alshamsi F, Rhodes A, Evans L, Angus DC, Alhazzani W. The efficacy and safety of prokinetic agents in critically ill patients receiving enteral nutrition: a systematic review and meta-analysis of randomized trials. Crit Care. 2016; 20:259. PMID: 27527069.
Article33. Guenter PA, Settle RG, Perlmutter S, Marino PL, DeSimone GA, Rolandelli RH. Tube feeding-related diarrhea in acutely Ill patients. JPEN J Parenter Enteral Nutr. 1991; 15:277–280. PMID: 1650854.34. Williams P, Cotta MO, Roberts JA. Pharmacokinetics/pharmacodynamics of β-lactams and therapeutic drug monitoring: from theory to practical issues in the intensive care unit. Semin Respir Crit Care Med. 2019; 40:476–487. PMID: 31585474.
Article35. McFarland LV, Surawicz CM, Greenberg RN, Elmer GW, Moyer KA, Melcher SA, Bowen KE, Cox JL. Prevention of beta-lactam-associated diarrhea by Saccharomyces boulardii compared with placebo. Am J Gastroenterol. 1995; 90:439–448. PMID: 7872284.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Sources and Formulation of Macro- and Micro-Nutrients in Enteral Nutrition Formula
- Factors Influencing the Occurrence of Diarrhea in Patients Admitted to Intensive Care Units
- Esophageal Obstruction Caused by the Solidification of Residue of an Enteral Feeding Formula
- Effects of Fiber in Enteral Formula on Stool Frequency
- Enteral nutrition associated non-occlusive bowel ischemia