Int J Stem Cells.
2021 Nov;14(4):400-409. 10.15283/ijsc21083.
Peptides Targeting Fms-Related Tyrosine Kinase-4 Activate the Function of Natural Killer Cells in Acute Myeloid Leukemia
- Affiliations
-
- 1Department of Biomedicine & Health Sciences, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 2Leukemia Research Institute, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 3Catholic Hematology Hospital, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Department of Biomedical Science, CHA University, Seongnam, Korea
- KMID: 2522559
- DOI: http://doi.org/10.15283/ijsc21083
Abstract
- Background and Objectives
The increased expression for the Fms-related tyrosine kinase-4 (FLT-4, known as VEGFR-3) is relevant to dysfunctional natural killer (NK) cells in acute myeloid leukemia (AML). MAZ51 (M), a VEGFR-3 inhibiting chemical, was effectively restored the function of NK cells via the high expression of interferon-gamma (IFN-γ) in NK cells, as shown in our previous study. Although tremendous amount of clinical data using peptides are currently available in real clinic, peptides targeting FLT-4 in modulating immune cells such as NK cells are not fully elucidated.
Methods and Results
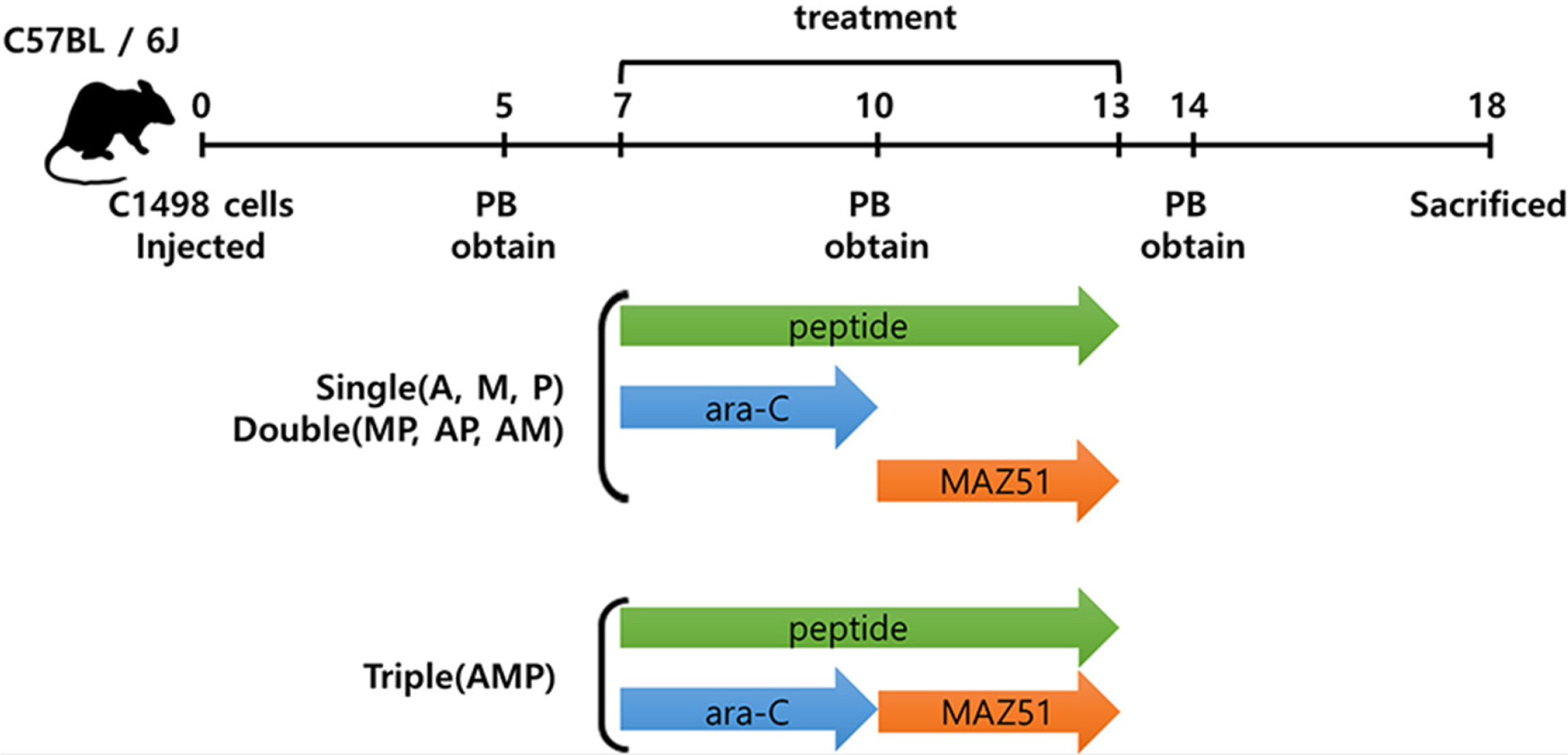
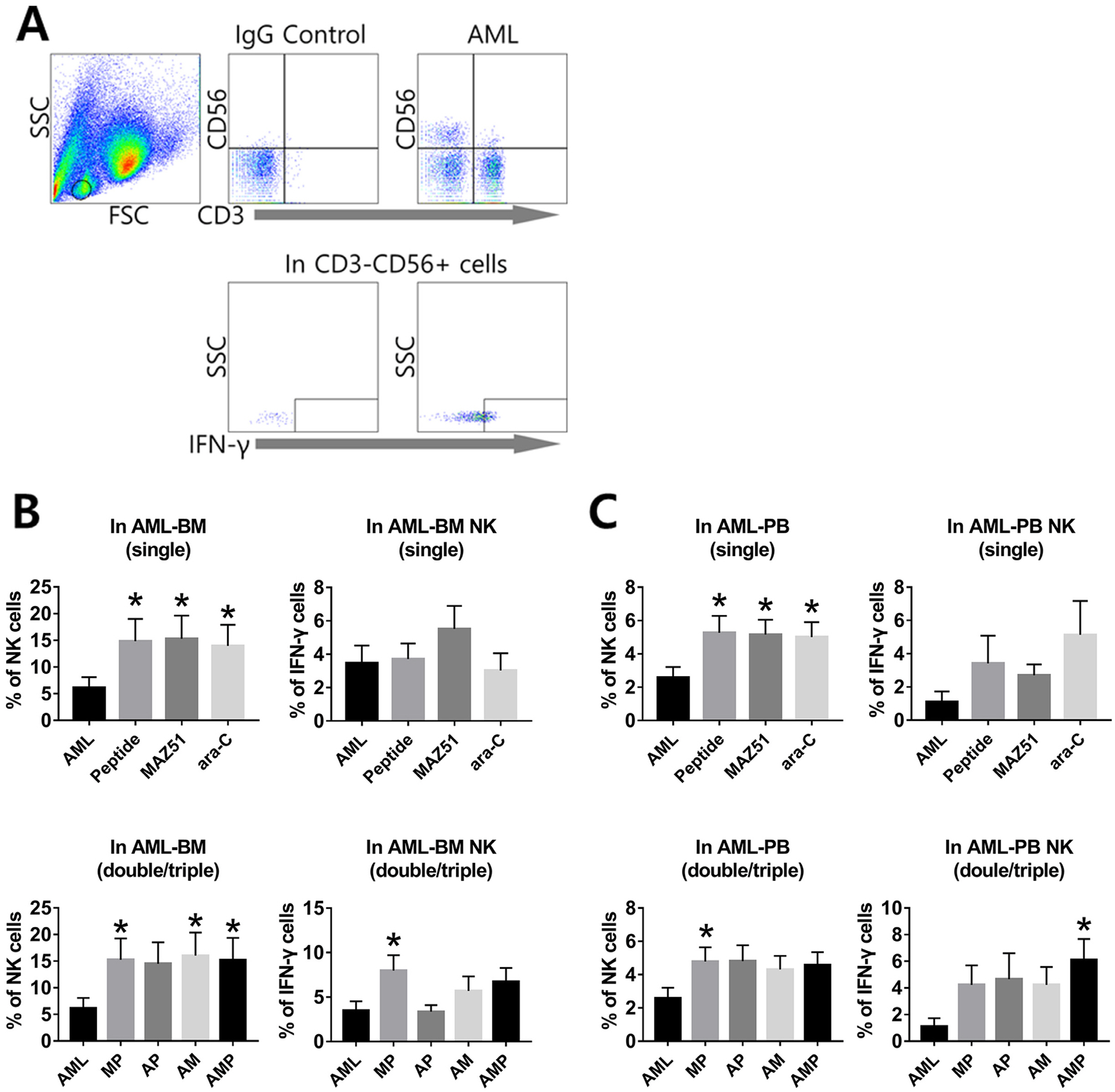
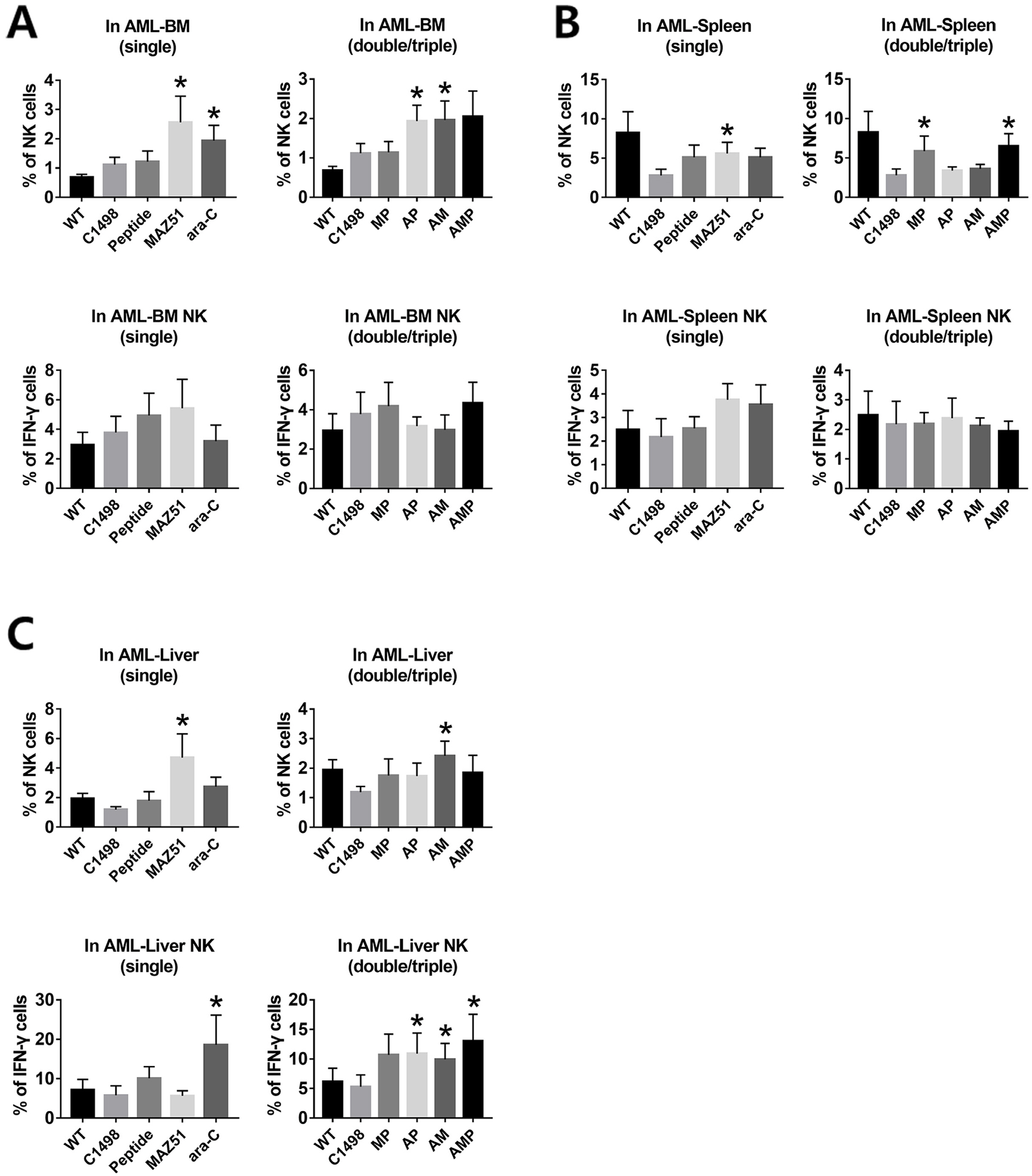
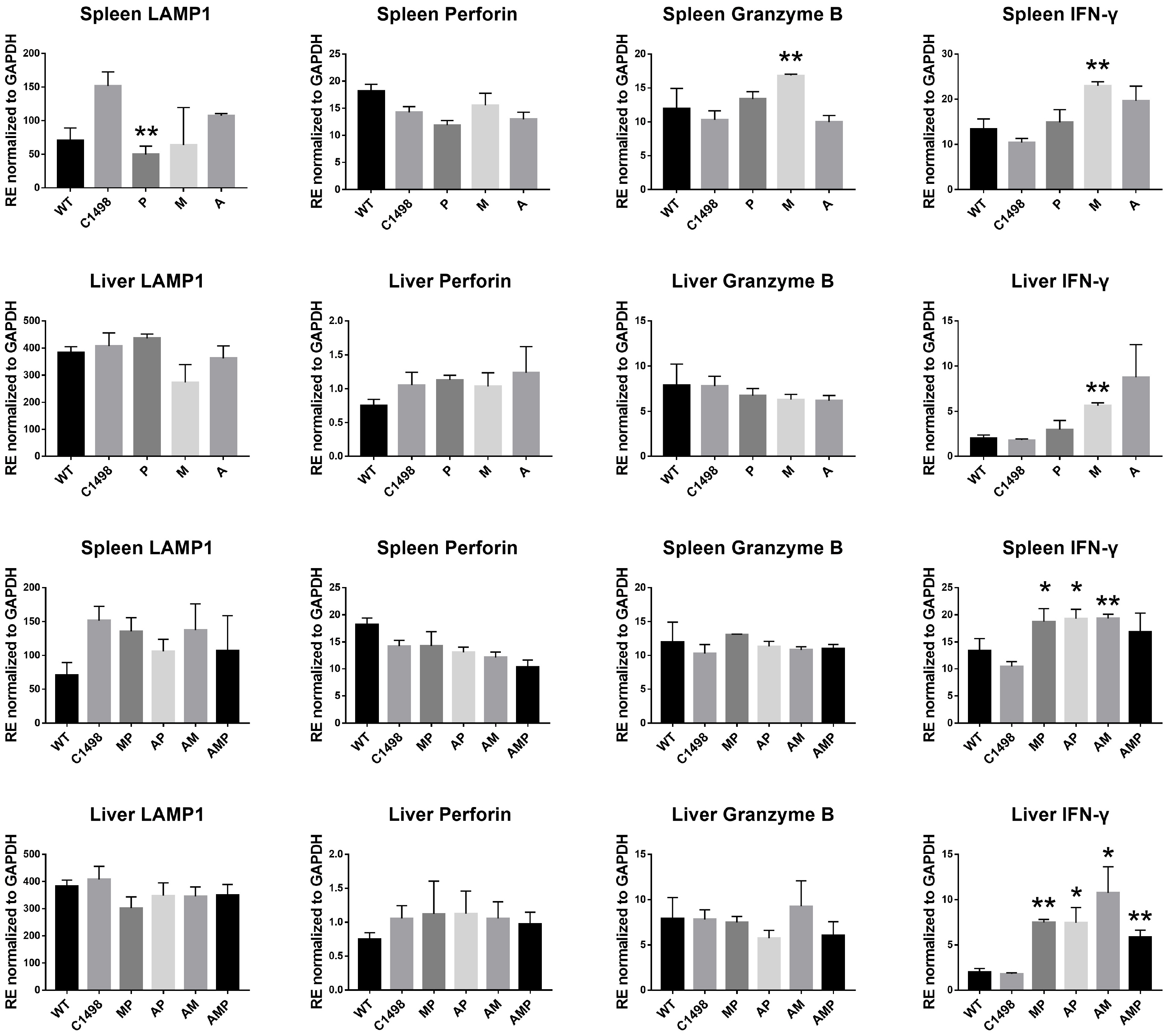
In present study, we developed peptides targeting FLT-4 (P), which is inhibiting an affinity for AML-NK expressing FLT-4 in vitro and in vivo. Bone marrow (BM) and peripheral blood (PB) mononuclear cells (MNCs) from AML patients were treated with combinational cocktails of the three agents including P, M, ara-C (A) and FLT-4 expression and IFN-γ release were examined. In an AML mouse model, IFN-γ expression were examined in T and NK cells from mouse BM, spleen, and liver to address relevance between peptides and immune cell activation. We found that AML-NK cells both in human and mouse samples showed a gradual increase the IFN-γ levels compared to the controls. There was a trend toward a reduction in leukemic blasts in the BM, spleen, and liver from the AML mice, when we compared the effects of combinational treatments.
Conclusions
Our results suggest that the function of AML-NK cells was synergistically activated by P in combination with M or A.
Keyword
Figure
Reference
-
References
1. Folkman J. 1971; Tumor angiogenesis: therapeutic implications. N Engl J Med. 285:1182–1186. DOI: 10.1056/NEJM197111182852108. PMID: 4938153.
Article2. Kampen KR, Scherpen FJG, Mahmud H, Ter Elst A, Mulder AB, Guryev V, Verhagen HJMP, De Keersmaecker K, Smit L, Kornblau SM, De Bont ESJM. 2018; VEGFC antibody therapy drives differentiation of AML. Cancer Res. 78:5940–5948. DOI: 10.1158/0008-5472.CAN-18-0250. PMID: 30185550.
Article3. de Jonge HJ, Valk PJ, Veeger NJ, ter Elst A, den Boer ML, Cloos J, de Haas V, van den Heuvel-Eibrink MM, Kaspers GJ, Zwaan CM, Kamps WA, Löwenberg B, de Bont ES. 2010; High VEGFC expression is associated with unique gene expression profiles and predicts adverse prognosis in pediatric and adult acute myeloid leukemia. Blood. 116:1747–1754. DOI: 10.1182/blood-2010-03-270991. PMID: 20522712.
Article4. Pizzolo G, Trentin L, Vinante F, Agostini C, Zambello R, Masciarelli M, Feruglio C, Dazzi F, Todeschini G, Chilosi M, Veneri D, Zanotti R, Benedetti F, Perona G, Semenzato G. 1988; Natural killer cell function and lymphoid subpopulations in acute non-lymphoblastic leukaemia in complete remission. Br J Cancer. 58:368–372. DOI: 10.1038/bjc.1988.221. PMID: 3179190. PMCID: PMC2246608.
Article5. Rey J, Fauriat C, Kochbati E, Orlanducci F, Charbonnier A, D'Incan E, Andre P, Romagne F, Barbarat B, Vey N, Olive D. 2017; Kinetics of cytotoxic lymphocytes reconstitution after induction chemotherapy in elderly AML patients reveals progressive recovery of normal phenotypic and functional features in NK cells. Front Immunol. 8:64. DOI: 10.3389/fimmu.2017.00064. PMID: 28210257. PMCID: PMC5288405.
Article6. Vivier E, Tomasello E, Baratin M, Walzer T, Ugolini S. 2008; Functions of natural killer cells. Nat Immunol. 9:503–510. DOI: 10.1038/ni1582. PMID: 18425107.
Article7. Carlsten M, Järås M. 2019; Natural killer cells in myeloid malignancies: immune surveillance, NK cell dysfunction, and pharmacological opportunities to bolster the endogenous NK cells. Front Immunol. 10:2357. DOI: 10.3389/fimmu.2019.02357. PMID: 31681270. PMCID: PMC6797594.
Article8. Paul S, Lal G. 2017; The molecular mechanism of natural killer cells function and its importance in cancer immuno-therapy. Front Immunol. 8:1124. DOI: 10.3389/fimmu.2017.01124. PMID: 28955340. PMCID: PMC5601256.
Article9. Lee JY, Park S, Kim DC, Yoon JH, Shin SH, Min WS, Kim HJ. 2013; A VEGFR-3 antagonist increases IFN-γ expression on low functioning NK cells in acute myeloid leukemia. J Clin Immunol. 33:826–837. DOI: 10.1007/s10875-013-9877-2. PMID: 23404187.
Article10. Lee JY, Park S, Min WS, Kim HJ. 2014; Restoration of natural killer cell cytotoxicity by VEGFR-3 inhibition in myelogenous leukemia. Cancer Lett. 354:281–289. DOI: 10.1016/j.canlet.2014.08.027. PMID: 25157650.
Article11. Cho HI, Celis E. 2009; Optimized peptide vaccines eliciting extensive CD8 T-cell responses with therapeutic antitumor effects. Cancer Res. 69:9012–9019. DOI: 10.1158/0008-5472.CAN-09-2019. PMID: 19903852. PMCID: PMC2789207.
Article12. Chapel A, Garcia-Beltran WF, Hölzemer A, Ziegler M, Lunemann S, Martrus G, Altfeld M. 2017; Peptide-specific engagement of the activating NK cell receptor KIR2DS1. Sci Rep. 7:2414. DOI: 10.1038/s41598-017-02449-x. PMID: 28546555. PMCID: PMC5445099.
Article13. Allen TM. 2002; Ligand-targeted therapeutics in anticancer therapy. Nat Rev Cancer. 2:750–763. DOI: 10.1038/nrc903. PMID: 12360278.
Article14. Borghouts C, Kunz C, Groner B. 2005; Current strategies for the development of peptide-based anti-cancer therapeutics. J Pept Sci. 11:713–726. DOI: 10.1002/psc.717. PMID: 16138387.
Article15. Stiuso P, Caraglia M, De Rosa G, Giordano A. 2013; Bioactive peptides in cancer: therapeutic use and delivery strategies. J Amino Acids. 2013:568953. DOI: 10.1155/2013/568953. PMID: 23986866. PMCID: PMC3671240.
Article16. Liersch R, Schliemann C, Bieker R, Hintelmann H, Buechner T, Berdel WE, Mesters RM. 2008; Expression of VEGF-C and its receptor VEGFR-3 in the bone marrow of patients with acute myeloid leukaemia. Leuk Res. 32:954–961. DOI: 10.1016/j.leukres.2007.10.005. PMID: 18006056.
Article17. Kak G, Raza M, Tiwari BK. 2018; Interferon-gamma (IFN-γ): exploring its implications in infectious diseases. Biomol Concepts. 9:64–79. DOI: 10.1515/bmc-2018-0007. PMID: 29856726.
Article18. Lee SE, Lee JY, Han AR, Hwang HS, Min WS, Kim HJ. 2018; Effect of high VEGF-C mRNA expression on achievement of complete remission in adult acute myeloid leukemia. Transl Oncol. 11:567–574. DOI: 10.1016/j.tranon.2018.02.018. PMID: 29544089. PMCID: PMC5854918.
Article19. Abel AM, Yang C, Thakar MS, Malarkannan S. 2018; Natural killer cells: development, maturation, and clinical utili-zation. Front Immunol. 9:1869. DOI: 10.3389/fimmu.2018.01869. PMID: 30150991. PMCID: PMC6099181.
Article20. Sciumè G, De Angelis G, Benigni G, Ponzetta A, Morrone S, Santoni A, Bernardini G. 2011; CX3CR1 expression defines 2 KLRG1+ mouse NK-cell subsets with distinct functional properties and positioning in the bone marrow. Blood. 117:4467–4475. DOI: 10.1182/blood-2010-07-297101. PMID: 21364193.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Differentiation induction of dendritic cell phenotypes from human leukemic cell lines
- Prognostic Significance of FLT3 Internal Tandem Duplication in Acute Myeloid Leukemia with Normal Karyotype
- FLT3 mutations in acute myeloid leukemia: a review focusing on clinically applicable drugs
- Expansion and Activation of Natural Killer Cells for Cancer Immunotherapy
- Targeting the CXCL12/CXCR4 axis in acute myeloid leukemia: from bench to bedside