J Korean Med Sci.
2021 Nov;36(45):e289. 10.3346/jkms.2021.36.e289.
Analysis of Tertiary Hospital Utilization in Pediatric Orthopaedics: a Study Using Nationwide Sample Data from Korea
- Affiliations
-
- 1Department of Orthopaedic Surgery, Asan Medical Center Children's Hospital, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Orthopaedic Surgery, Hanyang University Hospital, Hanyang University College of Medicine, Seoul, Korea
- KMID: 2522548
- DOI: http://doi.org/10.3346/jkms.2021.36.e289
Abstract
- Background
In the Korean medical system, the severity classification for a specific disease depends primarily on its nationwide admission rate in tertiary hospitals. Inversely, one of the important designation criteria for a tertiary hospital is the hospital's treatment ratio of patients classified as having a specific severe disease. Most diseases requiring pediatric orthopaedic surgery (POS) are not currently classified as high severity in terms of disease severity. We investigated the admission rates for the representative POS diseases in tertiary hospitals and compared these rates with those for adult orthopaedic surgery (AOS) diseases.
Methods
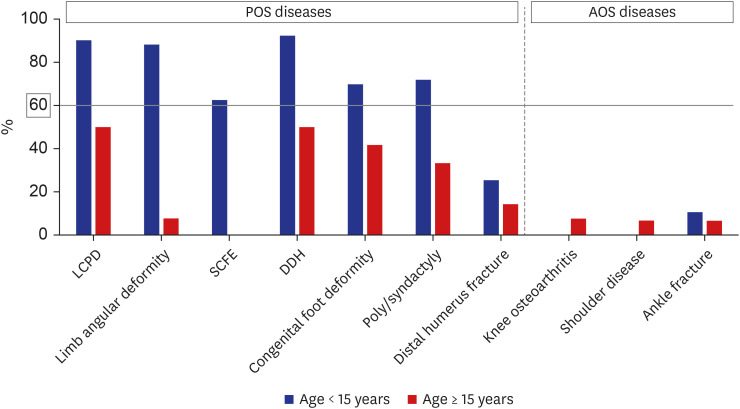
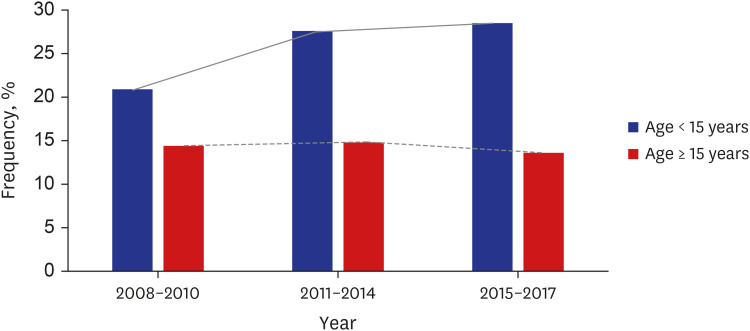
Seven POS diagnoses and three AOS diagnoses were selected based on frequency of admission. Nationwide sample data were used to investigate the admission rates for these representative diagnoses from 2008 to 2017.
Results
Six of the seven frequent POS diagnoses presented high admission rates in tertiary hospitals (62.5–92.3%). In contrast, all frequent AOS diagnoses presented low admission rates in tertiary hospitals.
Conclusion
The admission rates of frequent POS diagnoses in tertiary hospitals are high. Considering that these rates are the most important factors for the classification of disease severity, POS diseases seem to be underestimated in terms of severity. This may lead to a tendency for tertiary hospitals to intentionally reduce the admission of children with POS diseases. As a result, these children may not receive appropriate professional care. Therefore, for the disease severity, POS diseases should be classified differently from general AOS diseases by using different criteria reflecting the patient's age.
Keyword
Figure
Reference
-
1. Keehan SP, Sisko AM, Truffer CJ, Poisal JA, Cuckler GA, Madison AJ, et al. National health spending projections through 2020: economic recovery and reform drive faster spending growth. Health Aff (Millwood). 2011; 30(8):1594–1605. PMID: 21798885.
Article2. Piña IL, Cohen PD, Larson DB, Marion LN, Sills MR, Solberg LI, et al. A framework for describing health care delivery organizations and systems. Am J Public Health. 2015; 105(4):670–679. PMID: 24922130.
Article3. Kim AM, Cho S, Kim HJ, Jung H, Jo MW, Lee JY, et al. Primary care patients' preference for hospitals over clinics in Korea. Int J Environ Res Public Health. 2018; 15(6):15.
Article4. Kim S, Jung C, Yon J, Park H, Yang H, Kang H, et al. A review of the complexity adjustment in the Korean Diagnosis-Related Group (KDRG). Health Inf Manag. 2020; 49(1):62–68. PMID: 30157672.
Article5. Ko JA, Cho DY, Cho SA, Han SJ, Lee DH, Heo YJ. Empirical analysis of patient concentration in tertiary hospitals. Public Health Aff. 2019; 3(1):61–70.
Article6. Carli D, Garagnani L, Lando M, Fairplay T, Bernasconi S, Landi A, et al. VACTERL (vertebral defects, anal atresia, tracheoesophageal fistula with esophageal atresia, cardiac defects, renal and limb anomalies) association: disease spectrum in 25 patients ascertained for their upper limb involvement. J Pediatr. 2014; 164(3):458–462.e1-2. PMID: 24210691.7. Dobbe AM, Gibbons PJ. Common paediatric conditions of the lower limb. J Paediatr Child Health. 2017; 53(11):1077–1085. PMID: 29148202.
Article8. Lee IS. Investigation and proposals of Korean diagnosis related group and patient classification system. Korean J Med. 2018; 93(3):231–236.
Article9. Korean Ministry of Health and Welfare. Statutes of designation and evaluation the tertiary hospital. Updated 2016. Accessed June 25, 2021. http://opendata.hira.or.kr/op/opc/olapHifrqSickInfo.do .10. Averill RF, Mullin RL, Steinbeck BA, Goldfield NI, Grant TM. Development of the ICD-10 procedure coding system (ICD-10-PCS). Top Health Inf Manage. 2001; 21(3):54–88. PMID: 11234732.11. Abzug JM, Herman MJ. Management of supracondylar humerus fractures in children: current concepts. J Am Acad Orthop Surg. 2012; 20(2):69–77. PMID: 22302444.
Article12. Leroux J, Abu Amara S, Lechevallier J. Legg-Calvé-Perthes disease. Orthop Traumatol Surg Res. 2018; 104(1S):S107–S112. PMID: 29155310.
Article13. Kim I, Kim HA, Seo YI, Song YW, Jeong JY, Kim DH. The prevalence of knee osteoarthritis in elderly community residents in Korea. J Korean Med Sci. 2010; 25(2):293–298. PMID: 20119586.
Article14. Lee S, Kim SJ. Prevalence of knee osteoarthritis, risk factors, and quality of life: the Fifth Korean National Health and Nutrition Examination Survey. Int J Rheum Dis. 2017; 20(7):809–817. PMID: 26578271.
Article15. Oh JH, Chung SW, Oh CH, Kim SH, Park SJ, Kim KW, et al. The prevalence of shoulder osteoarthritis in the elderly Korean population: association with risk factors and function. J Shoulder Elbow Surg. 2011; 20(5):756–763. PMID: 21530320.
Article16. Health Insurance Review and Assessment Service. Open national data of admission statistics. Updated 2020. Accessed June 25, 2021. http://opendata.hira.or.kr/op/opc/olapHifrqSickInfo.do .17. Korean National Health Insurance Service. National sample cohort data for patients record. Updated 2018. Accessed June 25, 2021. https://nhiss.nhis.or.kr/bd/ay/bdaya001iv.do .18. Ahn E. Introducing big data analysis using data from National Health Insurance Service. Korean J Anesthesiol. 2020; 73(3):205–211. PMID: 32506896.
Article19. Kang MS, Kim HS. Characteristics and trends of traumatic injuries in children visiting emergency departments in South Korea: a retrospective serial cross-sectional study using both nationwide-sample and single-institutional data. PLoS One. 2019; 14(8):e0220798. PMID: 31398222.
Article20. Kim S, Kwon S. Has the National Health Insurance improved the inequality in the use of tertiary-care hospitals in Korea? Health Policy. 2014; 118(3):377–385. PMID: 25459734.
Article21. Health Insurance Review and Assessment Service. Improvement for evaluating disease group classification about the composition ratio of severe diseases in tertiary hospital. Updated 2019. Accessed June 25, 2021. http://repository.hira.or.kr/handle/2019.oak/1080 .22. Gutman IM, Niemeier TE, Gilbert SR. National databases in pediatric orthopaedic surgery: a comparison of demographics, procedures, and outcomes. J Pediatr Orthop. 2019; 39(8):e636–e640. PMID: 31393308.
Article23. Peddada KV, Sullivan BT, Margalit A, Sponseller PD. Fracture patterns differ between osteogenesis imperfecta and routine pediatric fractures. J Pediatr Orthop. 2018; 38(4):e207–e212. PMID: 29356793.
Article24. McClure PK, Herzenberg JE. The natural history of lower extremity malalignment. J Pediatr Orthop. 2019; 39(6):Suppl 1. S14–S19. PMID: 31169641.
Article25. Mosca VS. Flexible flatfoot in children and adolescents. J Child Orthop. 2010; 4(2):107–121. PMID: 21455468.
Article26. Bright RW, Burstein AH, Elmore SM. Epiphyseal-plate cartilage. A biomechanical and histological analysis of failure modes. J Bone Joint Surg Am. 1974; 56(4):688–703. PMID: 4835816.27. Polaner DM, Houck CS, Anderson C, Bannister C, Hardy C, Honkanen A, et al. Critical elements for the pediatric perioperative anesthesia environment. Pediatrics. 2015; 136(6):1200–1205. PMID: 26620064.
Article28. Salazar JH, Goldstein SD, Yang J, Gause C, Swarup A, Hsiung GE, et al. Regionalization of pediatric surgery: trends already underway. Ann Surg. 2016; 263(6):1062–1066. PMID: 26855367.29. Jones S, Phillips N, Ali F, Fernandes JA, Flowers MJ, Smith TW. Triplane fractures of the distal tibia requiring open reduction and internal fixation. Pre-operative planning using computed tomography. Injury. 2003; 34(4):293–298. PMID: 12667783.30. Lalonde KA, Letts M. Traumatic growth arrest of the distal tibia: a clinical and radiographic review. Can J Surg. 2005; 48(2):143–147. PMID: 15887795.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cancer Patients' Utilization of Tertiary Hospitals in Seoul Before and After the Benefit Expansion Policy
- A Study on Health Service Utilization and it's Determinants in the Low Income Family in Korea
- Impacts of Implementation of Patient Referral System in terms of Medical Expenditures and Medical Utilization
- Health Service Utilization Patterns Among The Chronically Disabled Aged in Korea
- Difference in Healthcare Utilization for Percutaneous Transluminal Coronary Angioplasty Inpatients by Insurance Types: Propensity Score Matching Analysis