J Korean Med Sci.
2021 Nov;36(43):e282. 10.3346/jkms.2021.36.e282.
Association of Gastroesophageal Reflux Disease with Preterm Birth: Machine Learning Analysis
- Affiliations
-
- 1AI Center, Korea University Anam Hospital, Seoul, Korea
- 2Department of Gastroenterology, Korea University Anam Hospital, Seoul, Korea
- 3Department of Obstetrics and Gynecology, Korea University Anam Hospital, Seoul, Korea
- 4Department of Oral and Maxillofacial Surgery, Korea University Anam Hospital, Seoul, Korea
- KMID: 2522288
- DOI: http://doi.org/10.3346/jkms.2021.36.e282
Abstract
- Background
This study used machine learning and population data for testing the associations of preterm birth with gastroesophageal reflux disease (GERD) and periodontitis.
Methods
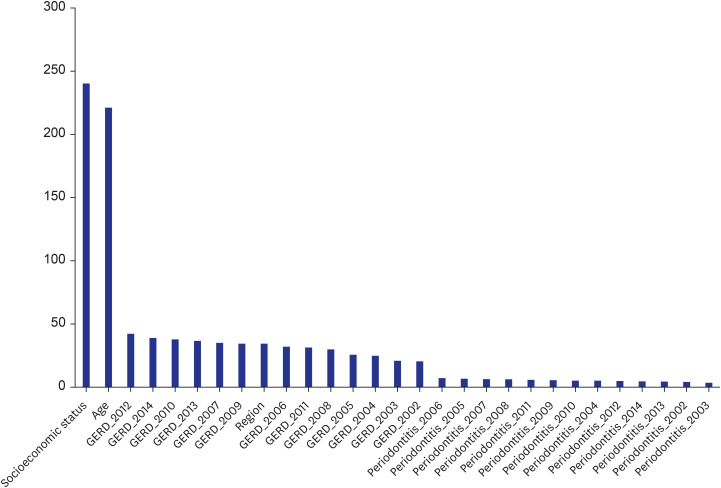
Retrospective cohort data came from Korea National Health Insurance Service claims data for all women who aged 25–40 years and gave births for the first time as singleton pregnancy during 2015–2017 (405,586 women). The dependent variable was preterm birth during 2015–2017 and the independent variables were GERD (coded as no vs. yes) for each of the years 2002–2014, periodontitis (coded as no vs. yes) for each of the years 2002–2014, age (year) in 2014, socioeconomic status in 2014 measured by an insurance fee, and region (city) (coded as no vs. yes) in 2014. Random forest variable importance was adopted for finding main predictors of preterm birth and testing its associations with GERD and periodontitis.
Results
Based on random forest variable importance, main predictors of preterm birth during 2015–2017 were socioeconomic status in 2014, age in 2014, GERD for the years 2012, 2014, 2010, 2013, 2007 and 2009, region (city) in 2014 and GERD for the year 2006. The importance rankings of periodontitis were relatively low.
Conclusion
Preterm birth has a stronger association with GERD than with periodontitis. For the prevention of preterm birth, preventive measures for GERD would be essential together with the improvement of socioeconomic status for pregnant women. Especially, it would be vital to promote active counseling for general GERD symptoms (neglected by pregnant women).
Figure
Reference
-
1. Magro Malosso ER, Saccone G, Simonetti B, Squillante M, Berghella V. US trends in abortion and preterm birth. J Matern Fetal Neonatal Med. 2018; 31(18):2463–2467. PMID: 28629238.
Article2. Lee NH. International trends and implications for preterm birth. Health Welf Policy Forum. 2013; (200):116–127.3. World Health Organization. News: Preterm birth. Updated 2018. Accessed June 1, 2019. http://www.who.int/news-room/fact-sheets/detail/preterm-birth.4. Harrison MS, Goldenberg RL. Global burden of prematurity. Semin Fetal Neonatal Med. 2016; 21(2):74–79. PMID: 26740166.
Article5. Eke PI, Dye BA, Wei L, Slade GD, Thornton-Evans GO, Borgnakke WS, et al. Update on prevalence of periodontitis in adults in the United States: NHANES 2009 to 2012. J Periodontol. 2015; 86(5):611–622. PMID: 25688694.
Article6. Puertas A, Magan-Fernandez A, Blanc V, Revelles L, O'Valle F, Pozo E, et al. Association of periodontitis with preterm birth and low birth weight: a comprehensive review. J Matern Fetal Neonatal Med. 2018; 31(5):597–602. PMID: 28282773.
Article7. Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R; Global Consensus Group. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006; 101(8):1900–1920. PMID: 16928254.
Article8. Patrick L. Gastroesophageal reflux disease (GERD): a review of conventional and alternative treatments. Altern Med Rev. 2011; 16(2):116–133. PMID: 21649454.9. Vinesh E, Masthan K, Kumar MS, Jeyapriya SM, Babu A, Thinakaran M. A clinicopathologic study of oral changes in gastroesophageal reflux disease, gastritis, and ulcerative colitis. J Contemp Dent Pract. 2016; 17(11):943–947. PMID: 27965506.10. Deppe H, Mücke T, Wagenpfeil S, Kesting M, Rozej A, Bajbouj M, et al. Erosive esophageal reflux vs. non erosive esophageal reflux: oral findings in 71 patients. BMC Oral Health. 2015; 15:84. PMID: 26208714.
Article11. Ali RA, Egan LJ. Gastroesophageal reflux disease in pregnancy. Best Pract Res Clin Gastroenterol. 2007; 21(5):793–806. PMID: 17889808.
Article12. Lee KS, Song IS, Kim ES, Ahn KH. Determinants of spontaneous preterm labor and birth including gastroesophageal reflux disease and periodontitis. J Korean Med Sci. 2020; 35(14):e105. PMID: 32281316.
Article13. Han J, Micheline K. Data Mining: Concepts and Techniques. 2nd ed. San Francisco, CA, USA: Elsevier;2006.14. Song JY, Kim HH, Cho EJ, Kim TY. The relationship between gastroesophageal reflux disease and chronic periodontitis. Gut Liver. 2014; 8(1):35–40. PMID: 24516699.
Article15. Adachi K, Mishiro T, Tanaka S, Yoshikawa H, Kinoshita Y. A study on the relationship between reflux esophagitis and periodontitis. Intern Med. 2016; 55(18):2523–2528. PMID: 27629943.
Article16. Souza RF, Huo X, Mittal V, Schuler CM, Carmack SW, Zhang HY, et al. Gastroesophageal reflux might cause esophagitis through a cytokine-mediated mechanism rather than caustic acid injury. Gastroenterology. 2009; 137(5):1776–1784. PMID: 19660463.
Article17. Kahrilas PJ. Turning the pathogenesis of acute peptic esophagitis inside out. JAMA. 2016; 315(19):2077–2078. PMID: 27187299.
Article18. Dunbar KB, Agoston AT, Odze RD, Huo X, Pham TH, Cipher DJ, et al. Association of acute gastroesophageal reflux disease with esophageal histologic changes. JAMA. 2016; 315(19):2104–2112. PMID: 27187303.
Article19. Hagberg H, Mallard C, Jacobsson B. Role of cytokines in preterm labour and brain injury. BJOG. 2005; 112(Suppl 1):16–18. PMID: 15715588.
Article20. Cappelletti M, Della Bella S, Ferrazzi E, Mavilio D, Divanovic S. Inflammation and preterm birth. J Leukoc Biol. 2016; 99(1):67–78. PMID: 26538528.
Article21. Sivarajasingam SP, Imami N, Johnson MR. Myometrial cytokines and their role in the onset of labour. J Endocrinol. 2016; 231(3):R101–R119. PMID: 27647860.
Article22. Pandey M, Chauhan M, Awasthi S. Interplay of cytokines in preterm birth. Indian J Med Res. 2017; 146(3):316–327. PMID: 29355137.23. Kim YJ, Lee BE, Park HS, Kang JG, Kim JO, Ha EH. Risk factors for preterm birth in Korea: a multicenter prospective study. Gynecol Obstet Invest. 2005; 60(4):206–212. PMID: 16088197.24. Di Renzo GC, Giardina I, Rosati A, Clerici G, Torricelli M, Petraglia F, et al. Maternal risk factors for preterm birth: a country-based population analysis. Eur J Obstet Gynecol Reprod Biol. 2011; 159(2):342–346. PMID: 22036591.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Determinants of Spontaneous Preterm Labor and Birth Including Gastroesophageal Reflux Disease and Periodontitis
- A Study of Gastroesophageal Reflux using 24hour pH Meter in Fullterm and Preterm Infants
- Relation between Gastroesophageal Reflux and Apnea in Preterm Infants
- 24 Hour Esophageal PH Monitoring in Preterm Infants
- Radiologic studies on gastroesophageal reflux