Neurointervention.
2021 Nov;16(3):252-259. 10.5469/neuroint.2021.00220.
Embolization Tactics of Spinal Epidural Arteriovenous Fistulas
- Affiliations
-
- 1Neurointervention Clinic, Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Diagnostic and Interventional Radiology Department, Imam Abdulrahman Bin Faisal University, King Fahd Hospital of the University, Al-Khobar City, Saudi Arabia
- KMID: 2522039
- DOI: http://doi.org/10.5469/neuroint.2021.00220
Abstract
- Purpose
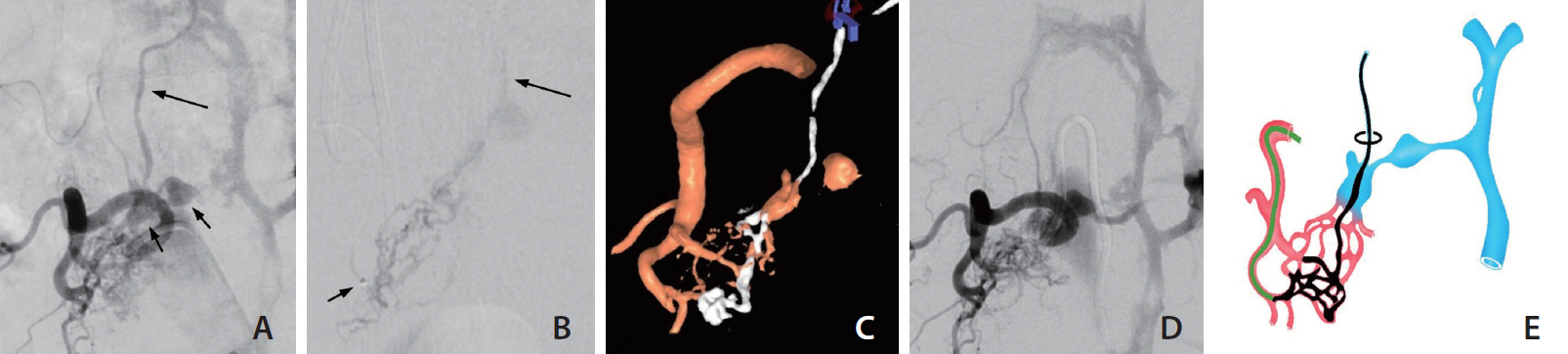
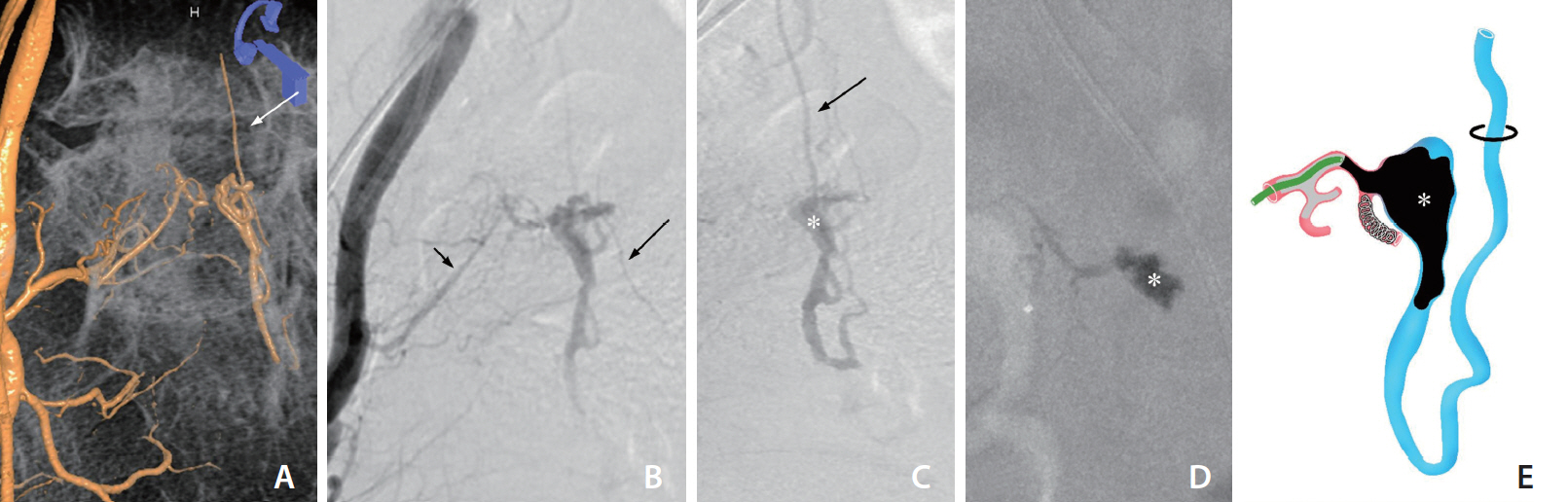
Spinal epidural arteriovenous fistulas (SEDAVFs) show an epidural venous sac often with venous congestive myelopathy (VCM) due to intradural reflux at a remote level to which a transarterial approach would be difficult. We present 12 cases of SEDAVF with VCM and describe 3 main tactics for effective transarterial embolization.
Materials and Methods
Among 152 patients with spinal vascular malformations diagnosed in our tertiary hospital between 1993 and 2019, 12 SEDAVF patients with VCM were included. Three different transarterial embolization tactics were applied according to the vascular configuration and microcatheter accessibility. We evaluated treatment results and clinical outcomes before and after treatment.
Results
Transarterial embolization with glue (20–30%) was performed in all patients. The embolization tactics applied in 12 patients were preferential flow (n=2), plug-and-push (n=6), and filling of the venous sac (n=4). Total occlusion of the SEDAVF, including intradural reflux, was achieved in 11 (91.7%) of 12 patients, and partial occlusion was achieved in 1 patient. No periprocedural complications were reported. Spinal cord edema was improved in all patients for an average of 18 months after treatment. Clinical functional outcome in terms of the pain, sensory, motor, and sphincter scale and modified Rankin scores improved during a mean 25-month follow-up (6.3 vs. 3.3, P=0.002; 3.6 vs. 2.3, P=0.002, respectively).
Conclusion
Endovascular treatment for 12 SEDAVF patients with VCM achieved a total occlusion rate of 91.7% without any periprocedural complication. The combined embolization tactics can block intradural reflux causing VCM, resulting in overall good clinical outcomes.
Keyword
Figure
Cited by 1 articles
-
Venous Congestive Myelopathy Caused by Spinal Vascular Malformation
Dae Chul Suh
Neurointervention. 2023;18(2):77-79. doi: 10.5469/neuroint.2023.00262.
Reference
-
1. Byun JS, Tsang ACO, Hilditch CA, Nicholson P, Fang YB, Krings T, et al. Presentation and outcomes of patients with thoracic and lumbosacral spinal epidural arteriovenous fistulas: a systematic review and meta-analysis. J Neurointerv Surg. 2019; 11:95–98.
Article2. Park JE, Koo HW, Liu H, Jung SC, Park D, Suh DC. Clinical characteristics and treatment outcomes of spinal arteriovenous malformations. Clin Neuroradiol. 2018; 28:39–46.
Article3. Geibprasert S, Pereira V, Krings T, Jiarakongmun P, Toulgoat F, Pongpech S, et al. Dural arteriovenous shunts: a new classification of craniospinal epidural venous anatomical bases and clinical correlations. Stroke. 2008; 39:2783–2794.4. Rangel-Castilla L, Holman PJ, Krishna C, Trask TW, Klucznik RP, Diaz OM. Spinal extradural arteriovenous fistulas: a clinical and radiological description of different types and their novel treatment with Onyx. J Neurosurg Spine. 2011; 15:541–549.
Article5. Takai K, Taniguchi M. Comparative analysis of spinal extradural arteriovenous fistulas with or without intradural venous drainage: a systematic literature review. Neurosurg Focus. 2012; 32:E8.
Article6. Takai K. Spinal arteriovenous shunts: angioarchitecture and historical changes in classification. Neurol Med Chir (Tokyo). 2017; 57:356–365.
Article7. Kiyosue H, Tanoue S, Okahara M, Hori Y, Kashiwagi J, Mori H. Spinal ventral epidural arteriovenous fistulas of the lumbar spine: angioarchitecture and endovascular treatment. Neuroradiology. 2013; 55:327–336.
Article8. Lenck S, Nicholson P, Tymianski R, Hilditch C, Nouet A, Patel K, et al. Spinal and paraspinal arteriovenous lesions. Stroke. 2019; 50:2259–2269.
Article9. Kiyosue H, Matsumaru Y, Niimi Y, Takai K, Ishiguro T, Hiramatsu M, JSNET Spinal AV Shunts Study Group, et al. Angiographic and clinical characteristics of thoracolumbar spinal epidural and dural arteriovenous fistulas. Stroke. 2017; 48:3215–3222.
Article10. Cho SH, Suh DC. Transdural segment of the radicular vein in spinal dural arteriovenous fistula. Neurointervention. 2017; 12:57–58.
Article11. Suh DC, Cho SH, Park JE, Liu H, Jung SC. Induced-wedge technique to improve liquid embolic agent penetration into spinal dural arteriovenous fistula. World Neurosurg. 2016; 96:309–315.
Article12. Gemmete JJ, Chaudhary N, Elias AE, Toma AK, Pandey AS, Parker RA, et al. Spinal dural arteriovenous fistulas: clinical experience with endovascular treatment as a primary therapy at 2 academic referral centers. AJNR Am J Neuroradiol. 2013; 34:1974–1979.
Article13. Su IC, terBrugge KG, Willinsky RA, Krings T. Factors determining the success of endovascular treatments among patients with spinal dural arteriovenous fistulas. Neuroradiology. 2013; 55:1389–1395.
Article14. Zhao LB, Shim JH, Lee DG, Suh DC. Two microcatheter technique for embolization of arteriovenous fistula with liquid embolic agent. Neurointervention. 2014; 9:32–38.
Article15. Song Y, Cho SH, Lee DW, Sheen JJ, Shin JH, Suh DC. Osseous versus nonosseous spinal epidural arteriovenous fistulas: experiences of 13 patients. AJNR Am J Neuroradiol. 2019; 40:129–134.
Article16. Suh DC. Where did the dura mater come from? Neurointervention. 2020; 15:2–3.
Article17. Suh DC, Song Y, Park D, Han M, Lim YM, Park JE, et al. New grading system for the clinical evaluation of patients with spinal vascular lesions. Neuroradiology. 2018; 60:1035–1041.
Article18. Jung SC, Song Y, Cho SH, Kim J, Noh SY, Lee SH, et al. Endovascular management of aneurysms associated with spinal arteriovenous malformations. J Neurointerv Surg. 2018; 10:198–203.
Article19. Adrianto Y, Yang KH, Koo HW, Park W, Jung SC, Park JE, et al. Concomitant origin of the anterior or posterior spinal artery with the feeder of a spinal dural arteriovenous fistula (SDAVF). J Neurointerv Surg. 2017; 9:405–410.
Article20. Lee CS, Pyun HW, Chae EY, Kim KK, Rhim SC, Suh DC. Reversible aggravation of neurological deficits after steroid medication in patients with venous congestive myelopathy caused by spinal arteriovenous malformation. Interv Neuroradiol. 2009; 15:325–329.
Article21. Nasr DM, Brinjikji W, Clarke MJ, Lanzino G. Clinical presentation and treatment outcomes of spinal epidural arteriovenous fistulas. J Neurosurg Spine. 2017; 26:613–620.
Article22. Huang W, Gross BA, Du R. Spinal extradural arteriovenous fistulas: clinical article. J Neurosurg Spine. 2013; 19:582–590.23. Takai K, Endo T, Yasuhara T, Seki T, Watanabe K, Tanaka Y, et al. Microsurgical versus endovascular treatment of spinal epidural arteriovenous fistulas with intradural venous drainage: a multicenter study of 81 patients. J Neurosurg Spine. 2020; 33:381–391.
Article24. Brinjikji W, Cloft H, Lanzino G. E-029 clinical, angioarchitectural and treatment characteristics of spinal dural arteriovenous fistulas versus spinal epidural arteriovenous fistulas. J Neurointerv Surg. 2020; 12:A42.25. Park KY, Kim JW, Kim BM, Kim DJ, Chung J, Jang CK, et al. Coil-protected technique for liquid embolization in neurovascular malformations. Korean J Radiol. 2019; 20:1285–1292.
Article26. Suh DC, Choi CG, Sung KB, Kim K-K, Rhim SC. Spinal osseous epidural arteriovenous fistula with multiple small arterial feeders converging to a round fistular nidus as a target of venous approach. AJNR Am J Neuroradiol. 2004; 25:69–73.27. Brinjikji W, Yin R, Nasr DM, Lanzino G. Spinal epidural arteriovenous fistulas. J Neurointerv Surg. 2016; 8:1305–1310.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A rare case of sacral epidural arteriovenous fistula with concomitant occult multiple lumbar epidural arteriovenous fistulas
- Spinal Epidural Arteriovenous Fistula Presented with Subdural Hematoma: a Case of Transarterial Embolization Using NBCA
- Traumatic Arteriovenous Fistulas of the Kidney: 2 Cases
- Endovascular Treatment of Spinal Dural and Epidural Arteriovenous Fistula as Complication of Lumbar Surgery
- Complication Associated with Onyx Embolization of Spinal Cord Arteriovenous Malformation