J Korean Neurosurg Soc.
2021 Nov;64(6):933-943. 10.3340/jkns.2020.0338.
Reduction of Radiation Exposure by Modifying Imaging Manner and Fluoroscopic Settings during Percutaneous Pedicle Screw Insertion
- Affiliations
-
- 1Department of Neurosurgery, Daegu Wooridul Spine Hospital, Daegu, Korea
- 2Department of Neurosurgery, Wooridul Spine Hospiral, Seoul, Korea
- 3Department of Anesthesiology and Pain Medicine, Daegu Wooridul Spine Hospital, Daegu, Korea
- KMID: 2521983
- DOI: http://doi.org/10.3340/jkns.2020.0338
Abstract
Objective
: Percutaneous pedicle screw (PPS) fixation is a needle based procedure that requires fluoroscopic image guidance. Consequently, radiation exposure is inevitable for patients, surgeons, and operation room staff. We hypothesize that reducing the production of radiation emission will result in reduced radiation exposure for everyone in the operation room. Research was performed to evaluate reduction of radiation exposure by modifying imaging manner and mode of radiation source.
Methods
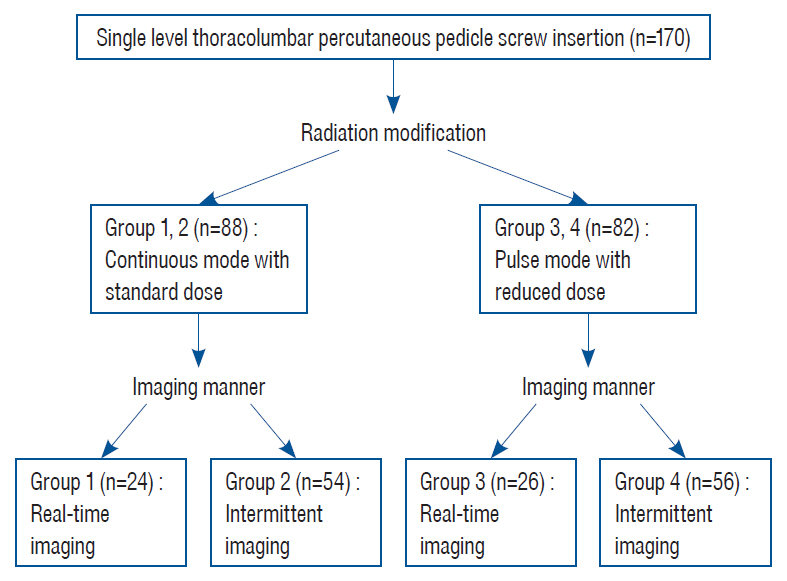
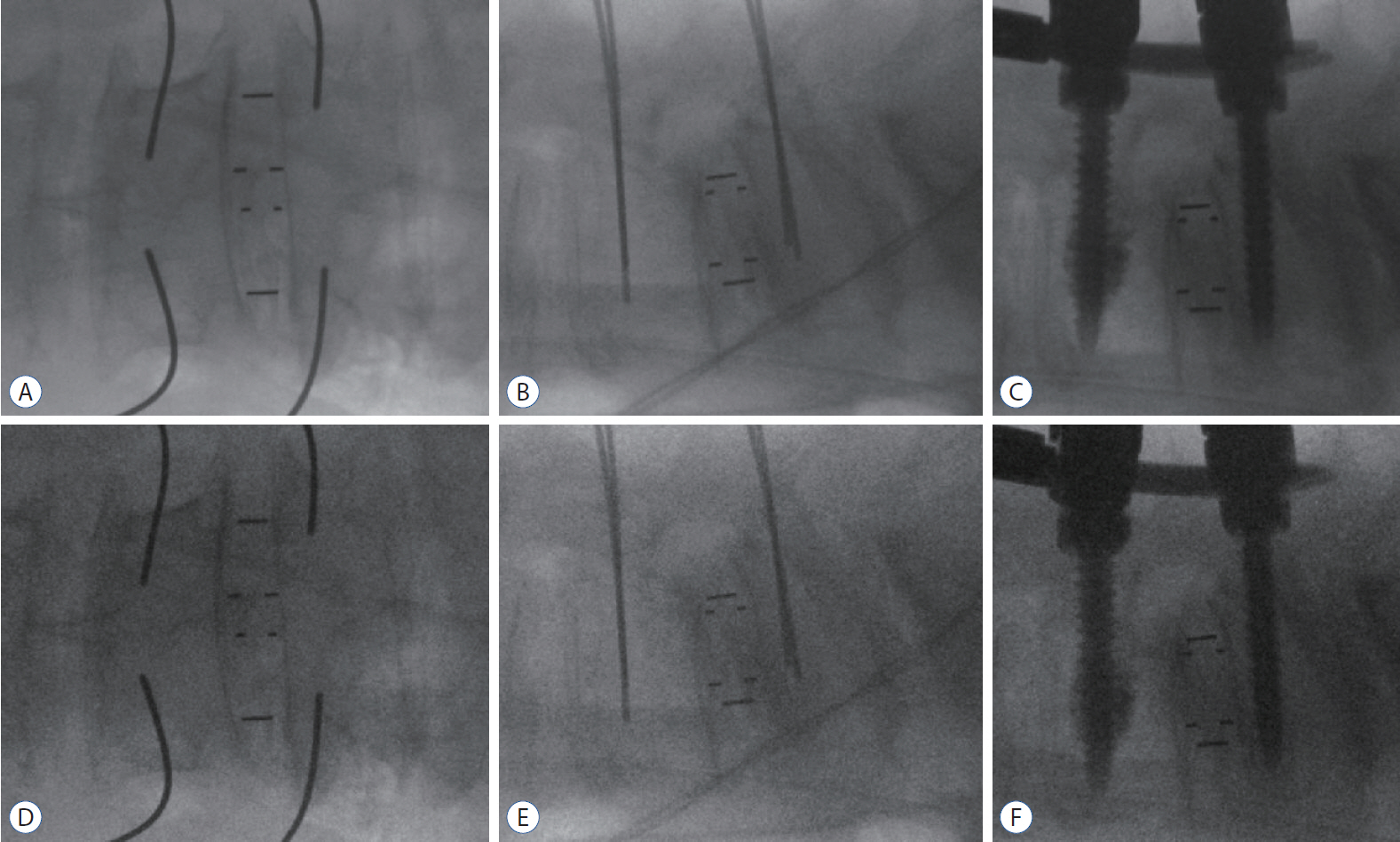
: A total of 170 patients (680 screws) who underwent fusion surgery with PPS fixation from September 2019 to March 2020 were analyzed in this study. Personal dosimeters (Polimaster Ltd.) were worn at the collar outside a lead apron to measure radiation exposure. Patients were assigned to four groups based on imaging manner of fluoroscopy and radiation modification (pulse mode with reduced dose) : continuous use without radiation modification (group 1, n=34), intermittent use without radiation modification (group 2, n=54), continuous use with radiation modification (group 3, n=26), and intermittent use with radiation modification (group 4, n=56). Post hoc Tukey Honest significant difference test was used for individual comparisons of radiation exposure/screw and fluoroscopic time/screw.
Results
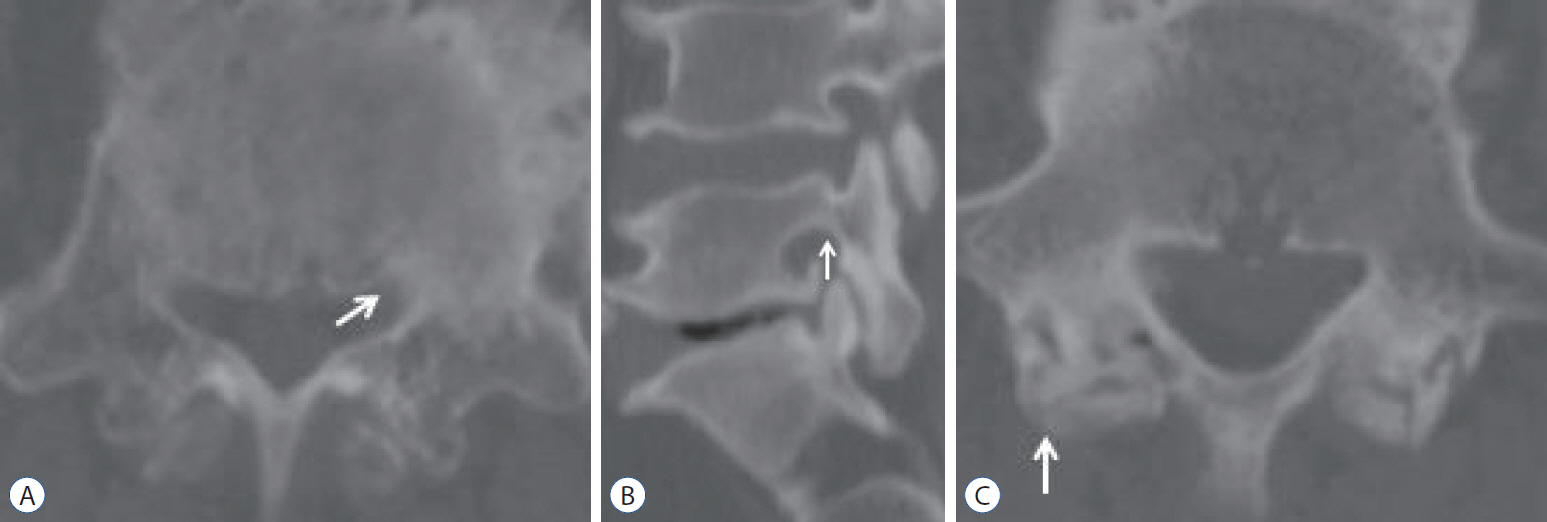
: The average radiation exposure/screw was 71.45±45.75 μSv/screw for group 1, 18.77±11.51 μSv/screw for group 2, 19.58±7.00 μSv/screw for group 3, and 4.26±2.89 μSv/screw for group 4. By changing imaging manner from continuous multiple shot to intermittent single shot, 73.7% radiation reduction was achieved in the no radiation modification groups (groups 1, 2), and 78.2% radiation reduction was achieved in the radiation modification groups (groups 3, 4). Radiation source modification from continuous mode with standard dose to pulse mode with reduced dose resulted in 72.6% radiation reduction in continuous imaging groups (groups 1, 3) and 77.3% radiation reduction in intermittent imaging groups (groups 2, 4). The average radiation exposure/screw was reduced 94.1% by changing imaging manner and modifying radiation source from continuous imaging with standard fluoroscopy setting (group 1) to intermittent imaging with modified fluoroscopy setting (group 4). A total of 680 screws were reviewed postoperatively, and 99.3% (675) were evaluated as pedicle breach grade 0 (<2 mm).
Conclusion
: The average radiation exposure/screw for a spinal surgeon can be reduced 94.1% by changing imaging manner and modifying radiation source from real-time imaging with standard dose to intermittent imaging with modified dose. These modifications can be instantly applied to any procedure using fluoroscopic guidance and may reduce the overall radiation exposure of spine surgeons.
Keyword
Figure
Reference
-
References
1. Ahn Y, Kim CH, Lee JH, Lee SH, Kim JS. Radiation exposure to the surgeon during percutaneous endoscopic lumbar discectomy: a prospective study. Spine (Phila Pa 1976). 38:617–625. 2013.
Article2. Bindal RK, Glaze S, Ognoskie M, Tunner V, Malone R, Ghosh S. Surgeon and patient radiation exposure in minimally invasive transforaminal lumbar interbody fusion. J Neurosurg Spine. 9:570–573. 2008.
Article3. Braun E, Sack AM, Sayed D, Manion S, Hamm B, Brimacombe M, et al. Reducing radiation exposure in lumbar transforaminal epidural steroid injections with pulsed fluoroscopy: a randomized, double-blind, controlled clinical trial. Pain Physician. 21:53–60. 2018.4. Choi HC. Fluoroscopic radiation exposure during percutaneous kyphoplasty. J Korean Neurosurg Soc. 49:37–42. 2011.
Article5. Gautschi OP, Schatlo B, Schaller K, Tessitore E. Clinically relevant complications related to pedicle screw placement in thoracolumbar surgery and their management: a literature review of 35,630 pedicle screws. Neurosurg Focus. 31:E8. 2011.
Article6. Godzik J, Nayar G, Hunter WD, Tumialán LM. Decreasing radiation emission in minimally invasive spine surgery using ultra-low-radiation imaging with image enhancement: a prospective cohort study. World Neurosurg. 122:e805–e811. 2019.
Article7. Gupta G, Singh R, Kotasthane DS, Kotasthane VD. Myelodysplastic syndromes/neoplasms: recent classification system based on World Health Organization classification of tumors - International Agency for Research on Cancer for Hematopoietic and Lymphoid Tissues. J Blood Med. 1:171–182. 2010.8. Hall EJ. Lessons we have learned from our children: cancer risks from diagnostic radiology. Pediatr Radiol. 32:700–706. 2002.
Article9. Hou BB, Yao Y, Wu LM, Qiao Y, Zheng LH, Ding LG, et al. Optimized fluoroscopy setting and appropriate project position can reduce X-ray radiation doses rates during electrophysiology procedures. Chin Med J (Engl). 128:1151–1153. 2015.
Article10. Lai ZH, Sá Dos Reis C, Sun Z. Effective dose and image optimisation of lateral lumbar spine radiography: a phantom study. Eur Radiol Exp. 4:13. 2020.
Article11. Lakhwani OP, Dalal V, Jindal M, Nagala A. Radiation protection and standardization. J Clin Orthop Trauma. 10:738–743. 2019.
Article12. Lee K, Lee KM, Park MS, Lee B, Kwon DG, Chung CY. Measurements of surgeons’ exposure to ionizing radiation dose during intraoperative use of C-arm fluoroscopy. Spine (Phila Pa 1976). 37:1240–1244. 2012.
Article13. Lee SY, Min E, Bae J, Chung CY, Lee KM, Kwon SS, et al. Types and arrangement of thyroid shields to reduce exposure of surgeons to ionizing radiation during intraoperative use of C-arm fluoroscopy. Spine (Phila Pa 1976). 38:2108–2112. 2013.
Article14. Lin EC. Radiation risk from medical imaging. Mayo Clin Proc. 85:1142–1146. quiz 1146. 2010.
Article15. Nayar G, Blizzard DJ, Wang TY, Cook S, Back AG, Vincent D, et al. Pedicle screw placement accuracy using ultra-low radiation imaging with image enhancement versus conventional fluoroscopy in minimally invasive transforaminal lumbar interbody fusion: an internally randomized controlled trial. J Neurosurg Spine. 28:186–193. 2018.
Article16. Richards PJ, George J, Metelko M, Brown M. Spine computed tomography doses and cancer induction. Spine (Phila Pa 1976). 35:430–433. 2010.
Article17. Smuck M, Zheng P, Chong T, Kao MC, Geisser ME. Duration of fluoroscopic-guided spine interventions and radiation exposure is increased in overweight patients. PM R. 5:291–6. quiz 296. 2013.
Article18. Srinivasan D, Than KD, Wang AC, La Marca F, Wang PI, Schermerhorn TC, et al. Radiation safety and spine surgery: systematic review of exposure limits and methods to minimize radiation exposure. World Neurosurg. 82:1337–1343. 2014.
Article19. Valentin J, Alexakhin RM, Cousins C, et al. The 2007 recommendations of the international commission on radiological protection. Orlando: Elsevier;2007.20. Wang H, Zhou Y, Li C, Liu J, Xiang L. Comparison of open versus percutaneous pedicle screw fixation using the sextant system in the treatment of traumatic thoracolumbar fractures. Clin Spine Surg. 30:E239–E246. 2017.
Article21. Wang TY, Farber SH, Perkins SS, Back AG, Byrd SA, Chi D, et al. Internally randomized control trial of radiation exposure using ultra-low radiation imaging versus traditional C-arm fluoroscopy for patients undergoing single-level minimally invasive transforaminal lumbar interbody fusion. Spine (Phila Pa 1976). 42:217–223. 2017.
Article22. Yoshihara H, Paulino CB. Radiation exposure to the surgeons and patients in fluoroscopic-guided segmental pedicle screw placement for pediatric scoliosis. Spine (Phila Pa 1976). 43:E1398–E1402. 2018.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Utility and Feasibility of Smart Glasses in Spine Surgery: Minimizing Radiation Exposure During Percutaneous Pedicle Screw Insertion
- Accuracy of Percutaneous Lumbosacral Pedicle Screw Placement Using the Oblique Fluoroscopic View Based on Computed Tomography Evaluations
- Commentary on “The Utility and Feasibility of Smart Glasses in Spine Surgery: Minimizing Radiation Exposure During Percutaneous Pedicle Screw Insertion”
- Accuracy of Percutaneous Pedicle Screw Placement after Single-Position versus Dual-Position Insertion for Lateral Interbody Fusion and Pedicle Screw Fixation Using Fluoroscopy
- Cervical Pedicle Screw Insertion Using the Technique with Direct Exposure of the Pedicle by Laminoforaminotomy