J Korean Neurosurg Soc.
2021 Nov;64(6):901-912. 10.3340/jkns.2020.0305.
Posterior Floating Laminotomy as a New Decompression Technique for Posterior Cervical Spinal Fusion Surgery
- Affiliations
-
- 1Department of Neurological Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2521980
- DOI: http://doi.org/10.3340/jkns.2020.0305
Abstract
Objective
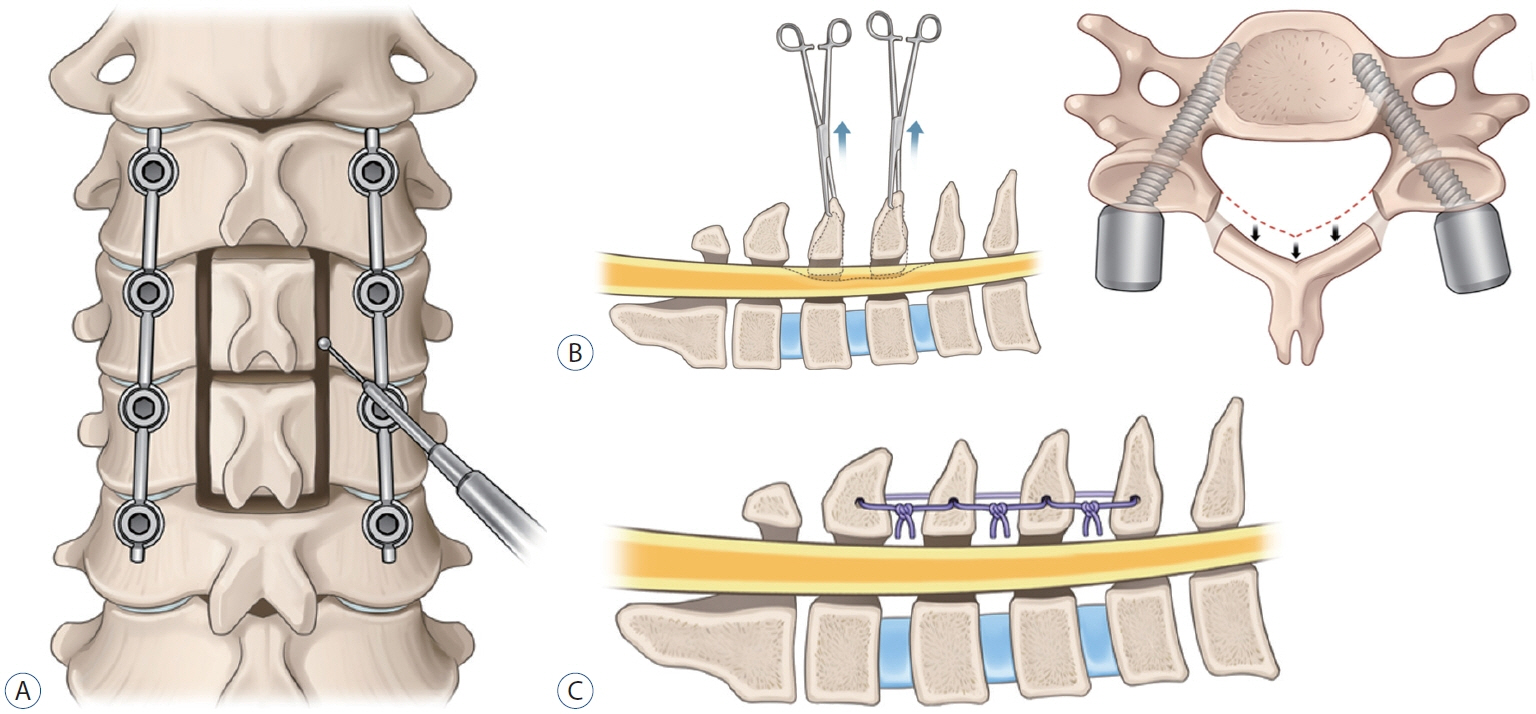
: In the cervical spine, many surgical procedures have been developed to achieve optimal results for various disorders, including degenerative diseases, traumatic injury, and tumor. In this study, we report our experience and follow-up results with a new surgical technique for cervical spine entitled posterior floating laminotomy (PFL) in comparison with conventional laminectomy and fusion (LF).
Methods
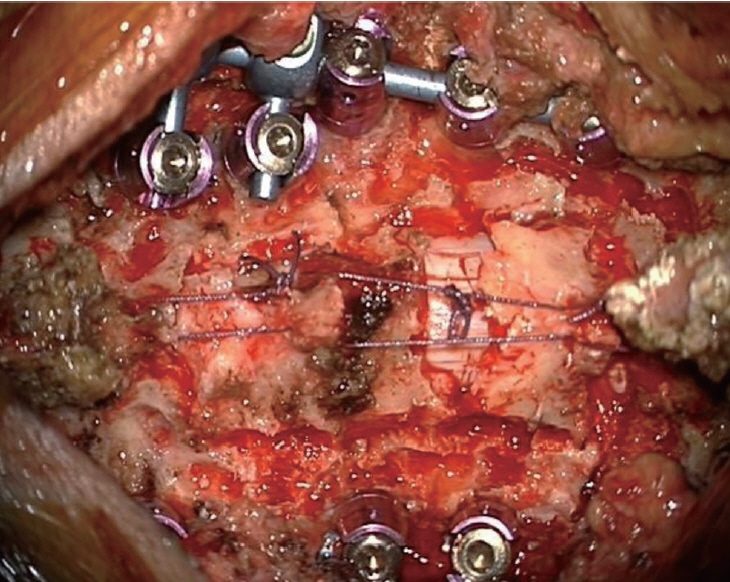
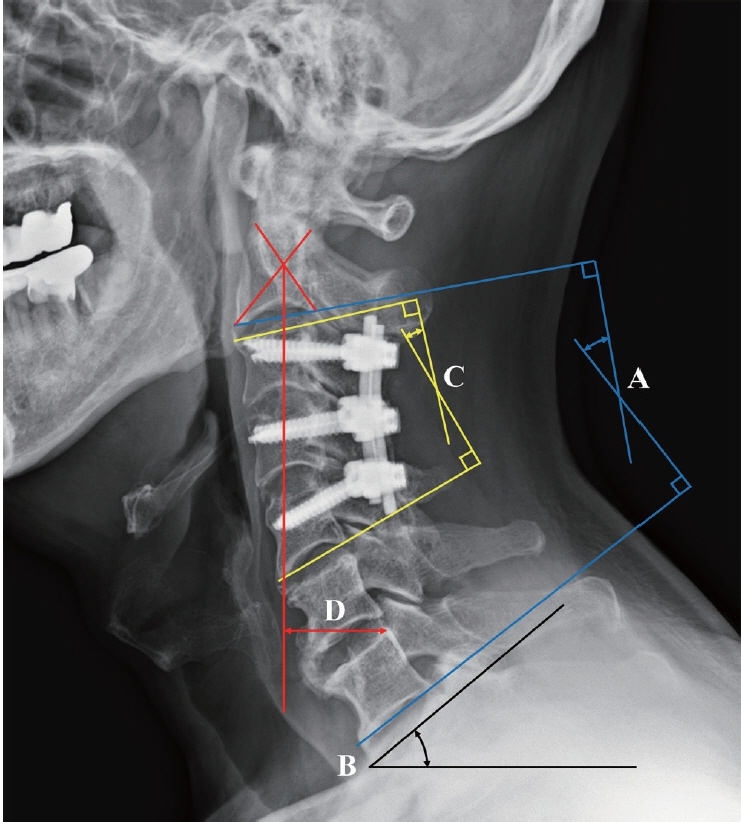
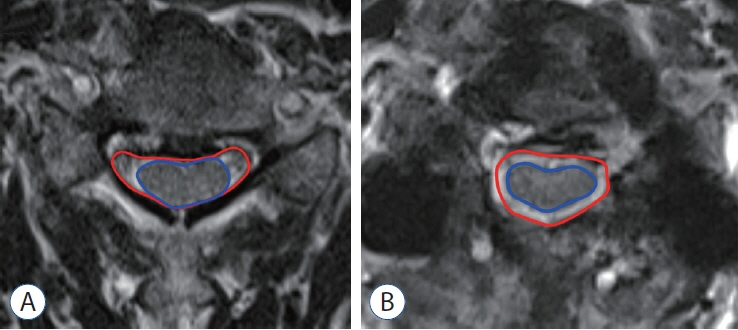
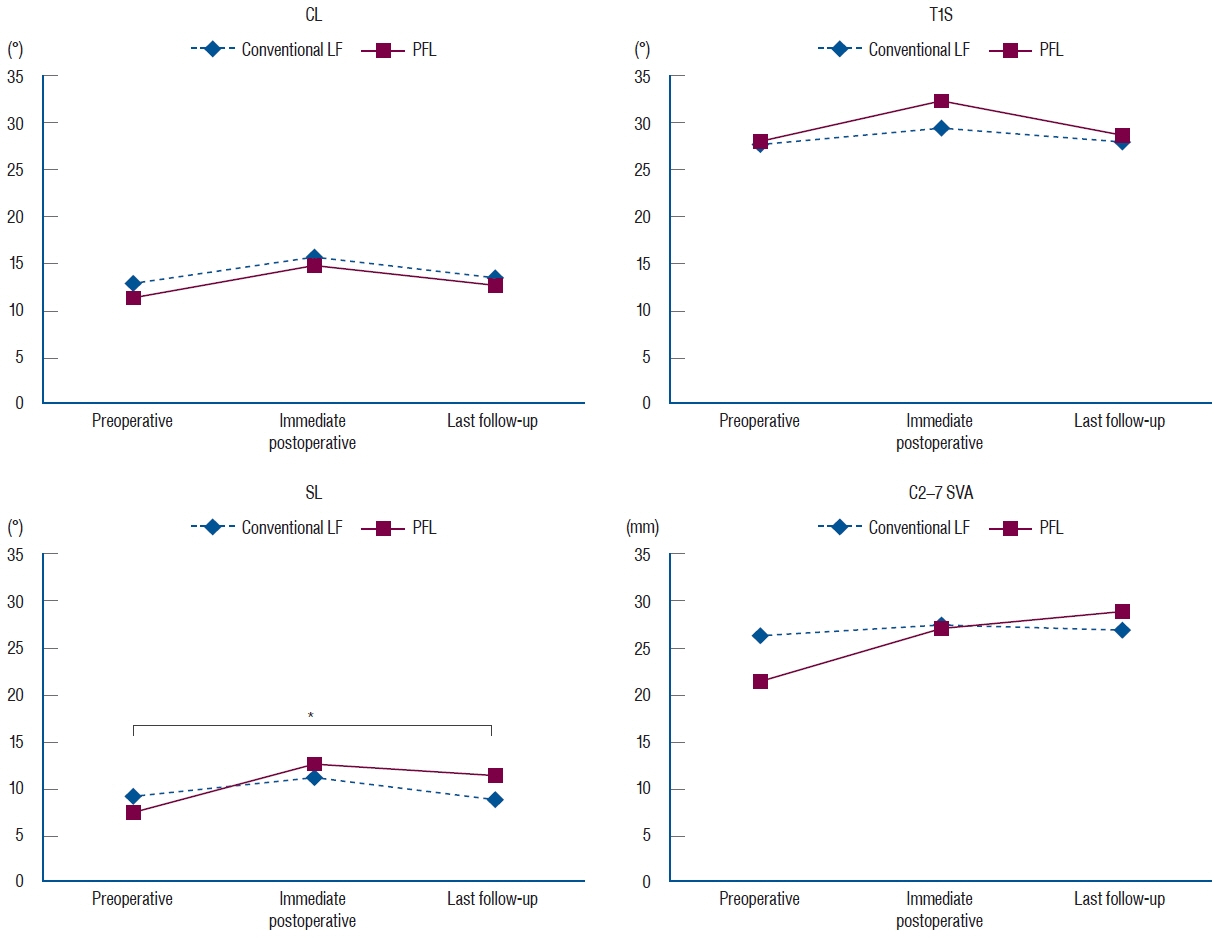
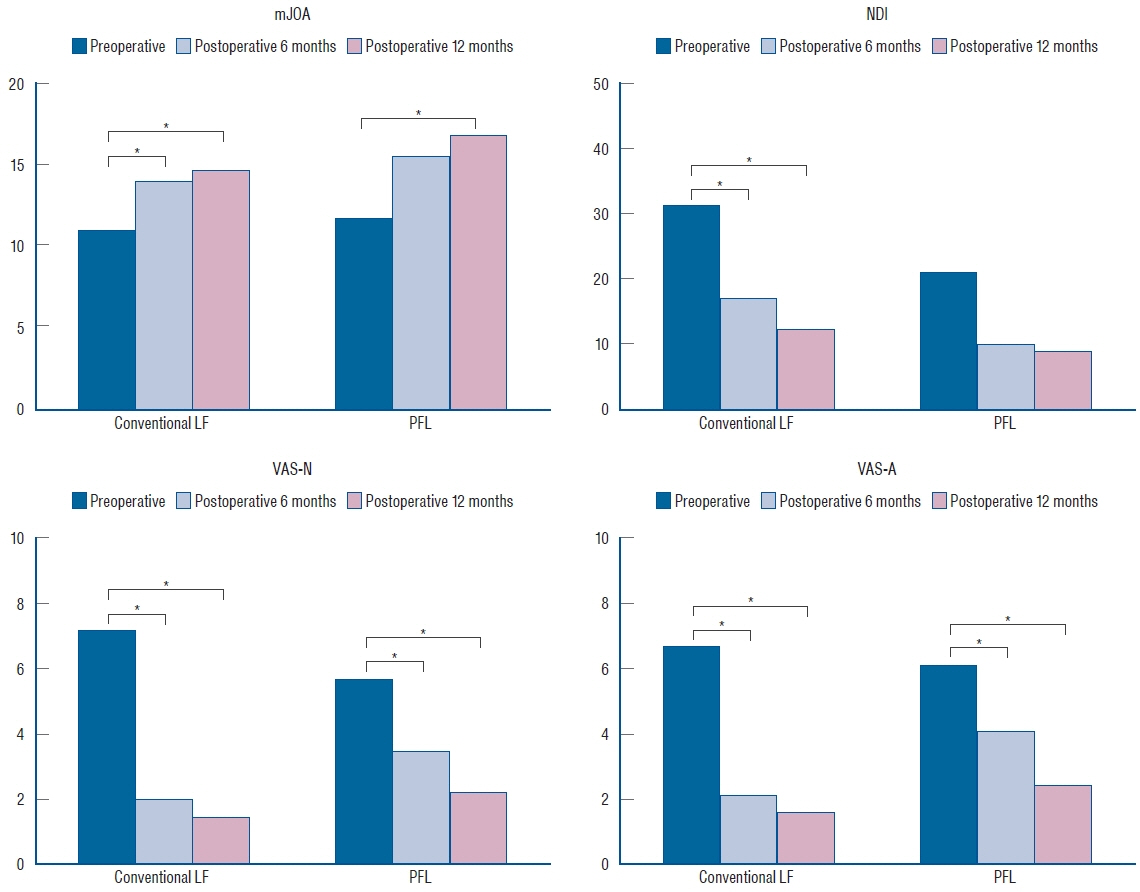
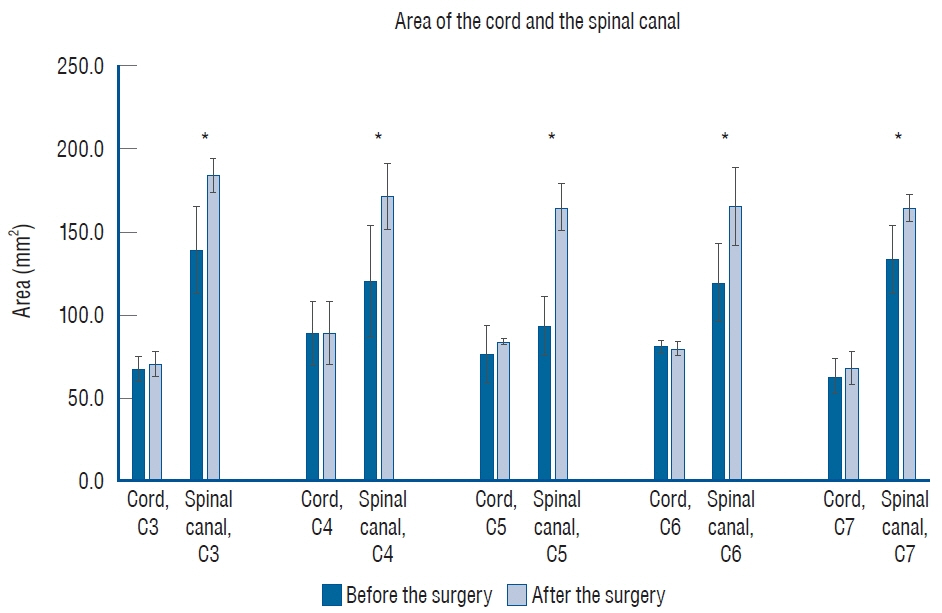
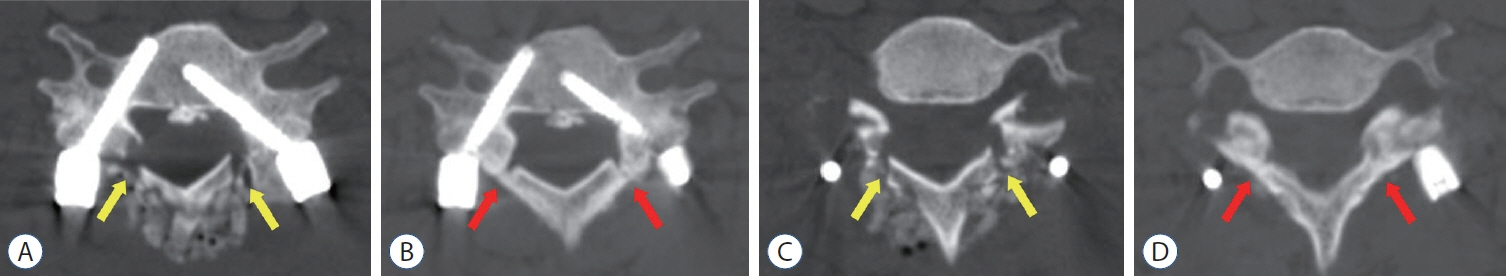
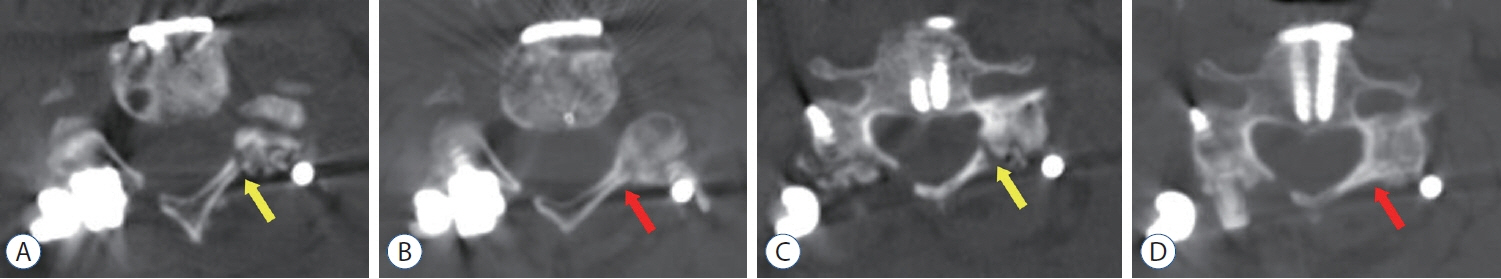
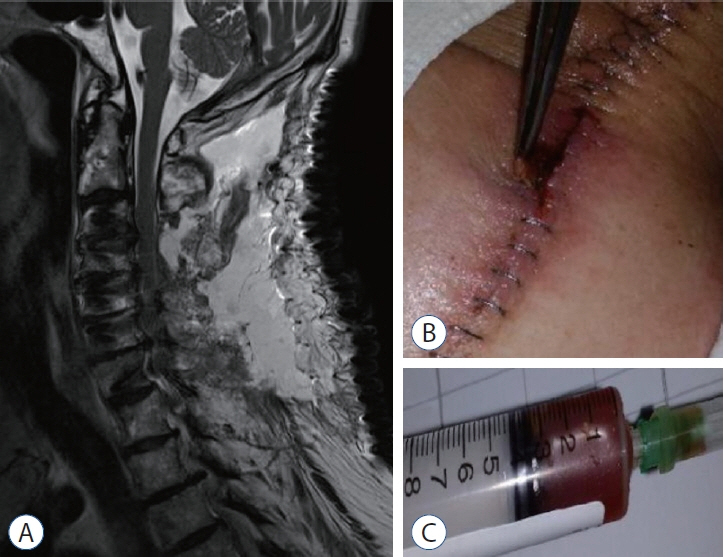
: Data for 85 patients who underwent conventional LF (n=66) or PFL (n=19) for cervical spine disorders between 2012 and 2019 were analyzed. Radiological parameters, including cervical lordosis (CL), T1 slope (T1S), segmental lordosis (SL), and C2–7 sagittal vertical axis (SVA), were measured with lateral spine X-rays. Functional outcomes, comprising the modified Japanese Orthopaedic Association (mJOA), neck disability index (NDI), and visual analog scale (VAS) scores, were also measured. For the patients who underwent PFL, postoperative magnetic resonance image (MRI) was performed in a month after the surgery, and the degree of decompression was evaluated at the T2-weighted axial image, and postoperative computed tomography (CT) was conducted immediately and 1 year after the operation to evaluate the gutter fusion.
Results
: There was no difference in CL, T1S, SL, and C2–7 SVA between the groups but there was a difference in the preoperative and postoperative SL angles. The mean difference in the preoperative SL angle compared with that at the last follow-up was -0.3° after conventional LF and 4.7° after PFL (p=0.04), respectively. mJOA, NDI, and VAS scores showed significant improvements (p<0.05) during follow-up in both groups. In the PFL group, postoperative MRI showed sufficient decompression and postoperative CT revealed gutter fusion at 1 year after the operation.
Conclusion
: PFL is a safe surgical method which can preserve postoperative CL and achieve good clinical outcomes.
Keyword
Figure
Reference
-
References
1. Anderson PA, Matz PG, Groff MW, Heary RF, Holly LT, Kaiser MG, et al. Laminectomy and fusion for the treatment of cervical degenerative myelopathy. J Neurosurg Spine. 11:150–156. 2009.
Article2. Baba H, Furusawa N, Imura S, Kawahara N, Tsuchiya H, Tomita K. Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopathy. Spine (Phila Pa 1976). 18:2167–2173. 1993.
Article3. Baisden J, Voo LM, Cusick JF, Pintar FA, Yoganandan N. Evaluation of cervical laminectomy and laminoplasty. A longitudinal study in the goat model. Spine (Phila Pa 1976). 24:1283–1288. discussion 1288-1289. 1999.4. Blizzard DJ, Caputo AM, Sheets CZ, Klement MR, Michael KW, Isaacs RE, et al. Laminoplasty versus laminectomy with fusion for the treatment of spondylotic cervical myelopathy: short-term follow-up. Eur Spine J. 26:85–93. 2017.
Article5. Cierny G 3rd. Surgical treatment of osteomyelitis. Plast Reconstr Surg 127 Suppl. 1:190S–204S. 2011.
Article6. Deutsch H, Haid RW, Rodts GE, Mummaneni PV. Postlaminectomy cervical deformity. Neurosurg Focus. 15:E5. 2003.
Article7. Fehlings MG, Santaguida C, Tetreault L, Arnold P, Barbagallo G, Defino H, et al. Laminectomy and fusion versus laminoplasty for the treatment of degenerative cervical myelopathy: results from the AOSpine North America and International prospective multicenter studies. Spine J. 17:102–108. 2017.
Article8. Gage MJ, Yoon RS, Gaines RJ, Dunbar RP, Egol KA, Liporace FA. Dead space management after orthopaedic trauma: tips, tricks, and pitfalls. J Orthop Trauma. 30:64–70. 2016.9. Highsmith JM, Dhall SS, Haid RW Jr, Rodts GE Jr, Mummaneni PV. Treatment of cervical stenotic myelopathy: a cost and outcome comparison of laminoplasty versus laminectomy and lateral mass fusion. J Neurosurg Spine. 14:619–625. 2011.
Article10. Hukuda S, Mochizuki T, Ogata M, Shichikawa K, Shimomura Y. Operations for cervical spondylotic myelopathy. A comparison of the results of anterior and posterior procedures. J Bone Joint Surg Br. 67:609–615. 1985.
Article11. Kaptain GJ, Simmons NE, Replogle RE, Pobereskin L. Incidence and outcome of kyphotic deformity following laminectomy for cervical spondylotic myelopathy. J Neurosurg. 93(2 Suppl):199–204. 2000.
Article12. Kitahara T, Hanakita J, Takahashi T. Postlaminectomy membrane with dynamic spinal cord compression disclosed with computed tomographic myelography: a case report and literature review. Spinal Cord Ser Cases. 3:17056. 2017.
Article13. Lawrence BD, Jacobs WB, Norvell DC, Hermsmeyer JT, Chapman JR, Brodke DS. Anterior versus posterior approach for treatment of cervical spondylotic myelopathy: a systematic review. Spine (Phila Pa 1976). 38(22 Suppl 1):S173–S182. 2013.14. Masuda S, Fujibayashi S, Otsuki B, Kimura H, Matsuda S. Efficacy of target drug delivery and dead space reduction using antibiotic-loaded bone cement for the treatment of complex spinal infection. Clin Spine Surg. 30:E1246–E1250. 2017.
Article15. McCormack HM, Horne DJ, Sheather S. Clinical applications of visual analogue scales: a critical review. Psychol Med. 18:1007–1019. 1988.
Article16. McLaughlin MR, Wahlig JB, Pollack IF. Incidence of postlaminectomy kyphosis after Chiari decompression. Spine (Phila Pa 1976). 22:613–617. 1997.
Article17. Metsemakers WJ, Fragomen AT, Moriarty TF, Morgenstern M, Egol KA, Zalavras C, et al. Evidence-based recommendations for local antimicrobial strategies and dead space management in fracture-related infection. J Orthop Trauma. 34:18–29. 2020.
Article18. Miyazaki K, Tada K, Matsuda Y, Okuno M, Yasuda T, Murakami H. Posterior extensive simultaneous multisegment decompression with posterolateral fusion for cervical myelopathy with cervical instability and kyphotic and/or S-shaped deformities. Spine (Phila Pa 1976). 14:1160–1170. 1989.
Article19. Ogura K, Miyamoto S, Sakuraba M, Chuman H, Fujiwara T, Kawai A. Immediate soft-tissue reconstruction using a rectus abdominis myocutaneous flap following wide resection of malignant bone tumours of the pelvis. Bone Joint J. 96-B:270–273. 2014.
Article20. Pal GP, Sherk HH. The vertical stability of the cervical spine. Spine (Phila Pa 1976). 13:447–449. 1988.
Article21. Pilitsis JG, Lucas DR, Rengachary SS. Bone healing and spinal fusion. Neurosurg Focus. 13:e1. 2002.
Article22. Prasad SS, O’Malley M, Caplan M, Shackleford IM, Pydisetty RK. MRI measurements of the cervical spine and their correlation to Pavlov’s ratio. Spine (Phila Pa 1976). 28:1263–1268. 2003.
Article23. Raynor RB, Pugh J, Shapiro I. Cervical facetectomy and its effect on spine strength. J Neurosurg. 63:278–282. 1985.
Article24. Rönnberg K, Lind B, Zoega B, Gadeholt-Göthlin G, Halldin K, Gellerstedt M, et al. Peridural scar and its relation to clinical outcome: a randomised study on surgically treated lumbar disc herniation patients. Eur Spine J. 17:1714–1720. 2008.
Article25. Rüegg TB, Wicki AG, Aebli N, Wisianowsky C, Krebs J. The diagnostic value of magnetic resonance imaging measurements for assessing cervical spinal canal stenosis. J Neurosurg Spine. 22:230–236. 2015.
Article26. Seo J, Park JH, Song EH, Lee YS, Jung SK, Jeon SR, et al. Postoperative nonpathologic fever after spinal surgery: incidence and risk factor analysis. World Neurosurg. 103:78–83. 2017.
Article27. Tan LA, Kasliwal MK, Traynelis VC. Surgical seroma. J Neurosurg Spine. 19:793–794. 2013.28. Vernon H, Mior S. The neck disability index: a study of reliability and validity. J Manipulative Physiol Ther. 14:409–415. 1991.29. Yew A, Kimball J, Lu DC. Surgical seroma formation following posterior cervical laminectomy and fusion without rhBMP-2: case report. J Neurosurg Spine. 19:297–300. 2013.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Ossification of Posterior Longitudinal Ligament in Cervical Spine with Anterior Fusion and Anterior Decompression: Report of 3 Cases
- A Case of Large Cervical Intradural Lipoma with Externsion into the Posterior Fossa
- Degenerative Cervical Myelopathy: Pathophysiology and Current Treatment Strategies
- Clinical Comparison between Decompression and Posterior Lumbar Interbody Fusion in Chronic Lower Back Pain Involving Degenerative Disc Disease and Spinal Stenosis
- Circumferential Spinal Cord Decompression through a Single Posterior Approach with Microendoscopy for Thoracic and Thoracolumbar Ossification of the Posterior Longitudinal Ligament