Diabetes Metab J.
2021 Sep;45(5):719-729. 10.4093/dmj.2020.0132.
Longitudinal Change in Myocardial Function and Clinical Parameters in Middle-Aged Subjects: A 3-Year Follow-up Study
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea
- 2Division of Cardiology, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea
- 3Division of Cardiology, Department of Internal Medicine, Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea
- KMID: 2520854
- DOI: http://doi.org/10.4093/dmj.2020.0132
Abstract
- Background
Metabolic syndrome (MetS) is closely associated with the aging process. However, changes in metabolic conditions and cardiac function that occur in middle aged population remain unclear. We evaluated longitudinal changes in metabolic parameters and cardiac function during a 3-year period in subjects with suspected MetS.
Methods
We studied 191 participants with suspected MetS at baseline and after 3 years. Anthropometric parameters, including waist circumference (WC), and metabolic parameters, including fasting blood glucose and lipid profile were measured. Conventional echocardiography with two-dimensional speckle tracking was performed.
Results
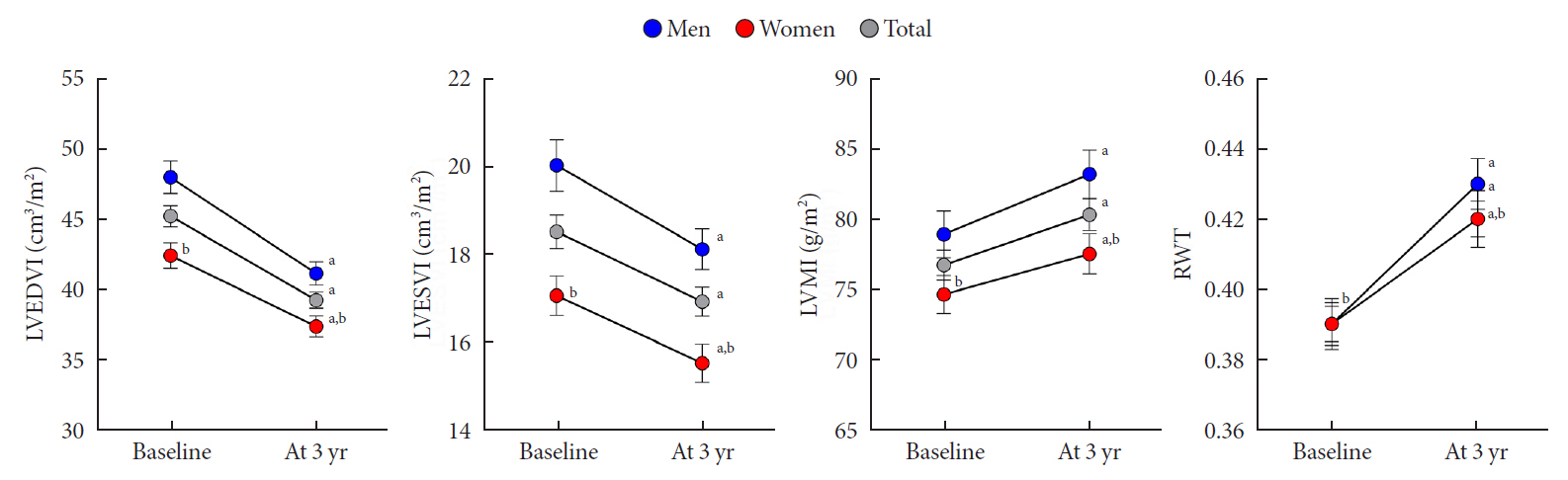
Mean age was 56.2±4.4 years, and there were 97 women (50.8%). Men had increased WC and triglycerides (TG) (WC 91.2±6.8 cm vs. 84.0±8.0 cm, P<0.001; TG 184.4±116.3 mg/dL vs. 128.2±53.6 mg/dL, P<0.001), and reduced global longitudinal strain (GLS) (–15.4%±2.1% vs. –17.1%±2.0%, P<0.001) compared to women. After 3.4 years, values of WC and TG did not change in men but increased in women (all P<0.05). The absolute value of left ventricular (LV) GLS did not change in men but was reduced in women (P=0.011). Change in TG was independently associated with worsening of LV GLS only in women (standardized β, –0.309; 95% confidence interval, –0.130 to –0.009; P=0.025).
Conclusion
In middle aged population, a vulnerable period for metabolic disturbance, cardiac remodeling tended to progress, which was prominent in women. Progression of adiposity and dyslipidemia after menopause may accelerate subclinical cardiac remodeling in middle-aged women. Lifestyle modification and medical interventions may help prevent further cardiac dysfunction in these subjects.
Figure
Reference
-
1. Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics: 2019 update. A report from the American Heart Association. Circulation. 2019; 139:e56–528.2. Kuznetsova T, Thijs L, Knez J, Cauwenberghs N, Petit T, Gu YM, et al. Longitudinal changes in left ventricular diastolic function in a general population. Circ Cardiovasc Imaging. 2015; 8:e002882.
Article3. Cheng S, Xanthakis V, Sullivan LM, Lieb W, Massaro J, Aragam J, et al. Correlates of echocardiographic indices of cardiac remodeling over the adult life course: longitudinal observations from the Framingham Heart Study. Circulation. 2010; 122:570–8.4. Gates PE, Gentile CL, Seals DR, Christou DD. Adiposity contributes to differences in left ventricular structure and diastolic function with age in healthy men. J Clin Endocrinol Metab. 2003; 88:4884–90.
Article5. Lieb W, Xanthakis V, Sullivan LM, Aragam J, Pencina MJ, Larson MG, et al. Longitudinal tracking of left ventricular mass over the adult life course: clinical correlates of short- and long-term change in the Framingham offspring study. Circulation. 2009; 119:3085–92.6. Yang H, Huynh QL, Venn AJ, Dwyer T, Marwick TH. Associations of childhood and adult obesity with left ventricular structure and function. Int J Obes (Lond). 2017; 41:560–8.
Article7. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail. 2016; 18:891–975.8. Lee HY, Oh BH. Paradigm shifts of heart failure therapy: do we need another paradigm? Int J Heart Fail. 2020; 2:145–56.
Article9. Lieb W, Gona P, Larson MG, Aragam J, Zile MR, Cheng S, et al. The natural history of left ventricular geometry in the community: clinical correlates and prognostic significance of change in LV geometric pattern. JACC Cardiovasc Imaging. 2014; 7:870–8.10. Kishi S, Gidding SS, Reis JP, Colangelo LA, Venkatesh BA, Armstrong AC, et al. Association of insulin resistance and glycemic metabolic abnormalities with LV structure and function in middle age: the CARDIA Study. JACC Cardiovasc Imaging. 2017; 10:105–14.11. Huh JH, Kang DR, Jang JY, Shin JH, Kim JY, Choi S, et al. Metabolic syndrome epidemic among Korean adults: Korean survey of Cardiometabolic Syndrome (2018). Atherosclerosis. 2018; 277:47–52.
Article12. Matthews KA, Crawford SL, Chae CU, Everson-Rose SA, Sowers MF, Sternfeld B, et al. Are changes in cardiovascular disease risk factors in midlife women due to chronological aging or to the menopausal transition? J Am Coll Cardiol. 2009; 54:2366–73.
Article13. Kim KJ, Cho HJ, Kim MS, Kang J, Kim KH, Kim D, et al. Focused update of 2016 Korean Society of Heart Failure guidelines for the management of chronic heart failure. Int J Heart Fail. 2019; 1:4–24.
Article14. Cho DH, Joo HJ, Kim MN, Lim DS, Shim WJ, Park SM. Association between epicardial adipose tissue, high-sensitivity C-reactive protein and myocardial dysfunction in middle-aged men with suspected metabolic syndrome. Cardiovasc Diabetol. 2018; 17:95.
Article15. Cho DH, Kim MN, Joo HJ, Shim WJ, Lim DS, Park SM. Visceral obesity, but not central obesity, is associated with cardiac remodeling in subjects with suspected metabolic syndrome. Nutr Metab Cardiovasc Dis. 2019; 29:360–6.
Article16. Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 2015; 28:1–39.
Article17. Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2016; 17:1321–60.
Article18. Cohn JN, Ferrari R, Sharpe N. Cardiac remodeling: concepts and clinical implications. A consensus paper from an international forum on cardiac remodeling. Behalf of an international forum on cardiac remodeling. J Am Coll Cardiol. 2000; 35:569–82.19. Geyer H, Caracciolo G, Abe H, Wilansky S, Carerj S, Gentile F, et al. Assessment of myocardial mechanics using speckle tracking echocardiography: fundamentals and clinical applications. J Am Soc Echocardiogr. 2010; 23:351–69.
Article20. Russo C, Jin Z, Elkind MS, Rundek T, Homma S, Sacco RL, et al. Prevalence and prognostic value of subclinical left ventricular systolic dysfunction by global longitudinal strain in a community-based cohort. Eur J Heart Fail. 2014; 16:1301–9.
Article21. Yingchoncharoen T, Agarwal S, Popovic ZB, Marwick TH. Normal ranges of left ventricular strain: a meta-analysis. J Am Soc Echocardiogr. 2013; 26:185–91.
Article22. Park JH, Lee JH, Lee SY, Choi JO, Shin MS, Kim MJ, et al. Normal 2-dimensional strain values of the left ventricle: a substudy of the normal echocardiographic measurements in Korean population study. J Cardiovasc Ultrasound. 2016; 24:285–93.
Article23. Lee HJ, Kim HL, Lim WH, Seo JB, Kim SH, Zo JH, et al. Subclinical alterations in left ventricular structure and function according to obesity and metabolic health status. PLoS One. 2019; 14:e0222118.
Article24. Division of Health Policy; Ministry of Health and Welfare. Korea Health Statistics 2018: Korea National Health and Nutrition Examination Survey (KNHANES VII-3). Osong: Ministry of Health and Welfare;2019.25. Son IH, Han YH, Hyun T. Changes in weight, waist circumference, prevalence of obesity, and dietary factors associated with weight gain over 8 years in Korean adults: longitudinal data from the Korean Genome and Epidemiology Study. J Nutr Health. 2017; 50:336–49.
Article26. van den Hurk K, Alssema M, Kamp O, Henry RM, Stehouwer CD, Smulders YM, et al. Independent associations of glucose status and arterial stiffness with left ventricular diastolic dysfunction: an 8-year follow-up of the Hoorn Study. Diabetes Care. 2012; 35:1258–64.
Article27. Krzesinski P, Stanczyk A, Piotrowicz K, Gielerak G, Uziebto-Zyczkowska B, Skrobowski A. Abdominal obesity and hypertension: a double burden to the heart. Hypertens Res. 2016; 39:349–55.
Article28. Mewton N, Liu CY, Croisille P, Bluemke D, Lima JA. Assessment of myocardial fibrosis with cardiovascular magnetic resonance. J Am Coll Cardiol. 2011; 57:891–903.
Article29. Szczepaniak LS, Dobbins RL, Metzger GJ, Sartoni-D’Ambrosia G, Arbique D, Vongpatanasin W, et al. Myocardial triglycerides and systolic function in humans: in vivo evaluation by localized proton spectroscopy and cardiac imaging. Magn Reson Med. 2003; 49:417–23.
Article30. Legedz L, Bricca G, Lantelme P, Rial MO, Champomier P, Vincent M, et al. Insulin resistance and plasma triglyceride level are differently related to cardiac hypertrophy and arterial stiffening in hypertensive subjects. Vasc Health Risk Manag. 2006; 2:485–90.
Article31. Park HA, Park JK, Park SA, Lee JS. Age, menopause, and cardiovascular risk factors among Korean middle-aged women: the 2005 Korea National Health and Nutrition Examination Survey. J Womens Health (Larchmt). 2010; 19:869–76.
Article32. Shin SH, Lee YJ, Heo YS, Park SD, Kwon SW, Woo SI, et al. Beneficial effects of bariatric surgery on cardiac structure and function in obesity. Obes Surg. 2017; 27:620–5.
Article33. Shah RV, Murthy VL, Abbasi SA, Eng J, Wu C, Ouyang P, et al. Weight loss and progressive left ventricular remodelling: the Multi-Ethnic Study of Atherosclerosis (MESA). Eur J Prev Cardiol. 2015; 22:1408–18.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Correlations between Serum Inflammation Factors and Left Ventricular Remodeling in Acute ST Segment Elevation Myocardial Infarction
- The Relationship between Handgrip Strength and Cognitive Function in Elderly Koreans over 8 Years: A Prospective Population-Based Study Using Korean Longitudinal Study of Ageing
- Two-year Follow-up Study of the Relationship between the Changes of Serum Homocysteine and Those of Serum Uric Acid Levels, Lipid Profiles and Renal Function in Gout Patients
- A Study on the Stage of Change in Exercise Behaviors, Exercise Self Efficacy, Depression and Stress in Middle Aged Women
- Quantitative Assessment of Myocardial Tissue Velocity in Normal Children with Doppler Tissue Imaging: Reference Values, Growth and Heart Rate Related Change