Korean J Transplant.
2021 Sep;35(3):161-167. 10.4285/kjt.21.0015.
Use of minor donors for living donor liver transplantation and associated ethical issues
- Affiliations
-
- 1Division of Hepatobiliary Surgery and Liver Transplantation, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2520677
- DOI: http://doi.org/10.4285/kjt.21.0015
Abstract
- Background
Living liver donation by minors is regarded as justifiable only if minors possess the capacity to consent to donation and the procedure is in their best interests. This study analyzed the incidence of and reasons for living donor liver transplantation (LDLT) by minor donors in Korea, and discussed ethical issues regarding liver donation by minors.
Methods
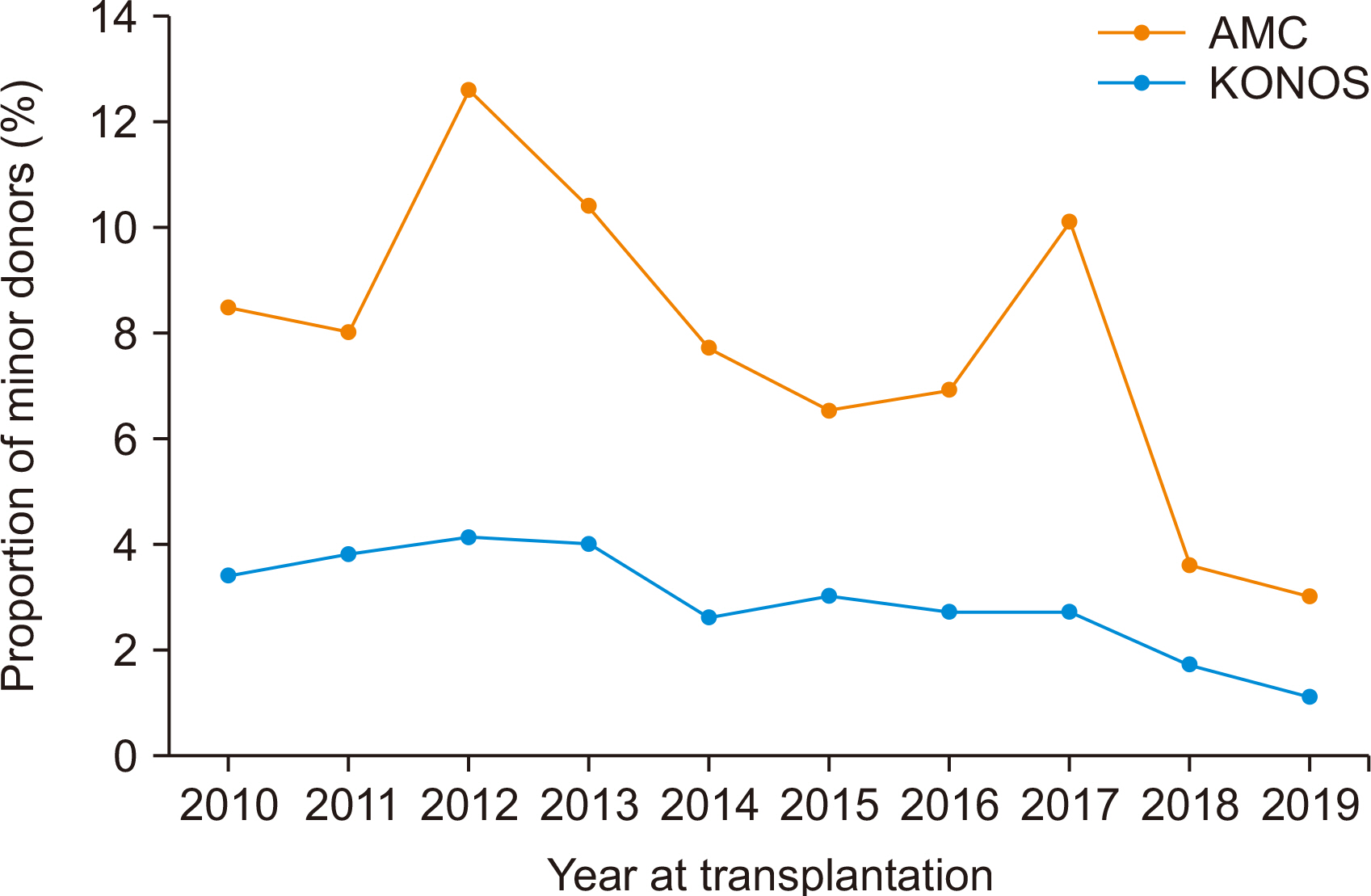
The databases of the Korean Network for Organ Sharing (KONOS) and Asan Medical Center (AMC) from 2010 to 2019 were retrospectively reviewed to determine the incidence of LDLT by minor donors.
Results
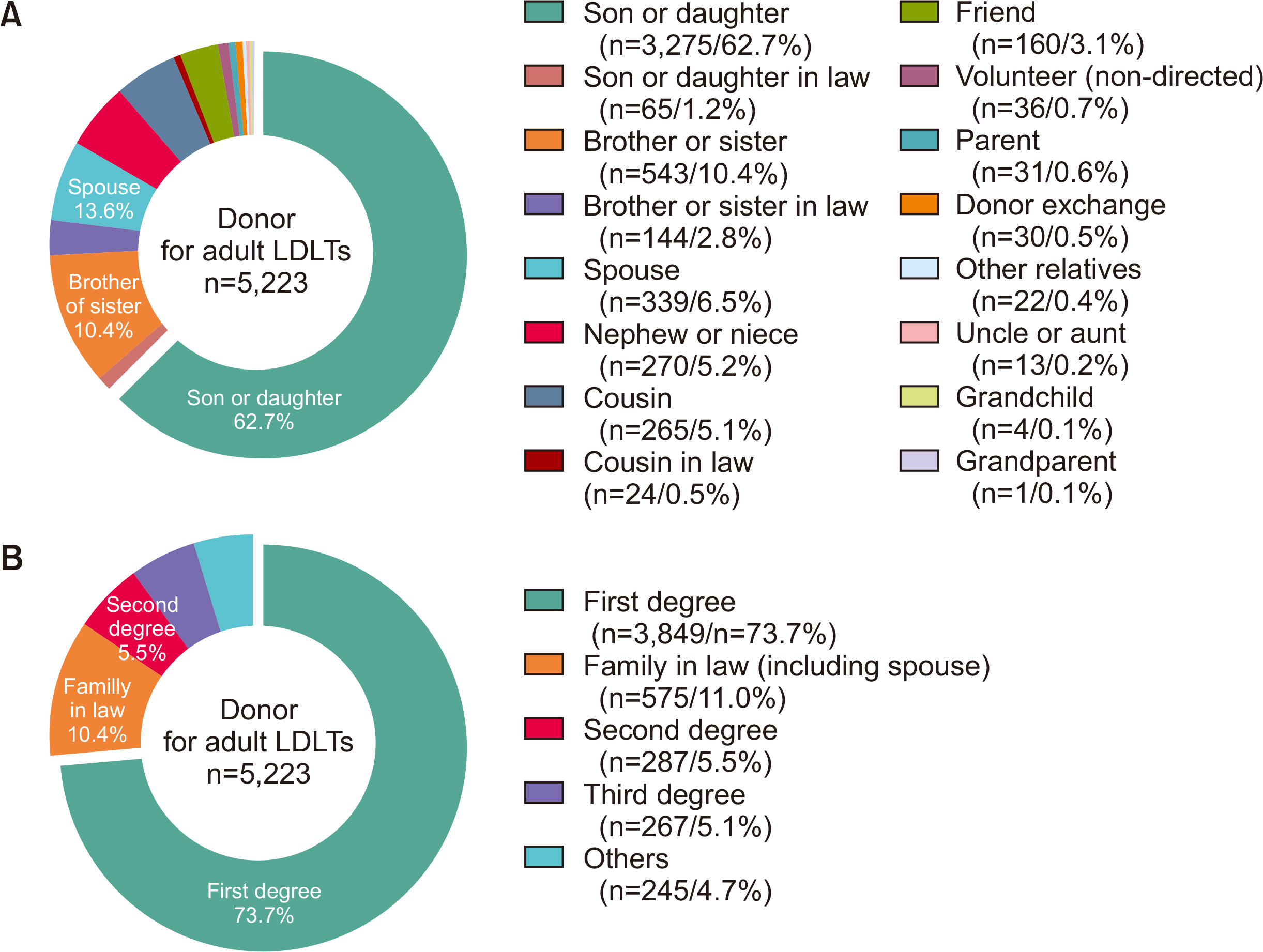
From 2010 to 2019, 590 (4.1%) of 14,243 liver donors in the KONOS database and 276 (7.5%) of 3,401 liver donors in the AMC database were minors. The proportions of minor donors in the KONOS and AMC databases were highest in 2012, at 4.1% and 12.6%, respectively, and lowest in 2019, at 1.1% and 3.0%, respectively. Because most LDLT recipients had relatively low model for end-stage liver disease scores and hepatocellular carcinoma, they were unlikely candidates for deceased-donor liver transplantation and were highly likely to drop out of LDLT if they waited for 1–2 years. The donor-recipient relationship of minor donors in the AMC database was first-degree in 256 (92.8%) and second- or third-degree in 20 (7.2%).
Conclusions
Liver donation by minors is limitedly acceptable only when the minor proves informed, well‐considered, and autonomous consent to the procedure and the procedure is in the minor's best interests. We suggest that minors be allowed to donate only to first-degree family members.
Figure
Reference
-
1. Capitaine L, Thys K, Van Assche K, Sterckx S, Pennings G. 2013; Should minors be considered as potential living liver donors? Liver Transpl. 19:649–55. DOI: 10.1002/lt.23633. PMID: 23463629.
Article2. Hwang S, Lee SG, Lee YJ, Sung KB, Park KM, Kim KH, et al. 2006; Lessons learned from 1,000 living donor liver transplantations in a single center: how to make living donations safe. Liver Transpl. 12:920–7. DOI: 10.1002/lt.20734. PMID: 16721780.
Article3. Lee JG, Lee KW, Kwon CH, Chu CW, Kim BW, Choi DL, et al. 2017; Donor safety in living donor liver transplantation: the Korean organ transplantation registry study. Liver Transpl. 23:999–1006. DOI: 10.1002/lt.24778. PMID: 28431203.
Article4. Choi SS, Cho SS, Kim SH, Jun IG, Hwang GS, Kim YK. 2013; Factors associated with blood transfusion in donor hepatectomy: results from 2344 donors at a large single center. Transplantation. 96:1000–7. DOI: 10.1097/TP.0b013e3182a41937. PMID: 23985722.5. Weithorn LA, Campbell SB. 1982; The competency of children and adolescents to make informed treatment decisions. Child Dev. 53:1589–98. DOI: 10.2307/1130087.
Article6. Hale S. 1990; A global developmental trend in cognitive processing speed. Child Dev. 61:653–63. DOI: 10.2307/1130951. PMID: 2364741.
Article7. Steinberg L, Cauffman E, Woolard J, Graham S, Banich M. 2009; Are adolescents less mature than adults?: minorsʼ access to abortion, the juvenile death penalty, and the alleged APA "flip-flop". Am Psychol. 64:583–94. DOI: 10.1037/a0014763. PMID: 19824745.8. Gardner M, Steinberg L. 2005; Peer influence on risk taking, risk preference, and risky decision making in adolescence and adulthood: an experimental study. Dev Psychol. 41:625–35. DOI: 10.1037/0012-1649.41.4.625. PMID: 16060809.
Article9. Schlam L, Wood JP. 2000; Informed consent to the medical treatment of minors: law and practice. Health Matrix Clevel. 10:141–74.10. Halpern-Felsher BL, Cauffman E. 2001; Costs and benefits of a decision: decision-making competence in adolescents and adults. J Appl Dev Psychol. 22:257–73. DOI: 10.1016/S0193-3973(01)00083-1.11. Farrington DP. 2003; Developmental and life-course criminology: key theoretical and empirical issues-The 2002 Sutherland Award address. Criminology. 41:221–55. DOI: 10.1111/j.1745-9125.2003.tb00987.x.
Article12. Ha H, Hong J, Kim I, Lee S, Lee A, Ha T, et al. 2019; Deceased donor liver transplantation under the Korean model for end-stage liver disease score-based liver allocation system: 2-year allocation results at a high-volume transplantation center. Korean J Transplant. 33:112–7. DOI: 10.4285/jkstn.2019.33.4.112.
Article13. Min SI, Ahn C, Han DJ, Kim SI, Chung SY, Lee SK, et al. 2015; To achieve national self-sufficiency: recent progresses in deceased donation in Korea. Transplantation. 99:765–70. DOI: 10.1097/TP.0000000000000412. PMID: 25226175.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Use of minor donors for living donor liver transplantation and associated ethical issues
- Current Issues in Living Donor Liver Transplantation
- Liver retransplantation for adult recipients
- Decreasing the operation time of living donor liver transplantation in the era of laparoscopic living donor hepatectomy
- Endoscopic management of anastomotic stricture after living-donor liver transplantation