Ann Surg Treat Res.
2021 Oct;101(4):197-205. 10.4174/astr.2021.101.4.197.
Bariatric surgery versus medical therapy in Korean obese patients: prospective multicenter nonrandomized controlled trial (KOBESS trial)
- Affiliations
-
- 1Department of Surgery, Seoul National University Hospital, Seoul, Korea
- 2Department of Surgery, Seoul National University Bundang Hospital, Seongnam, Korea
- 3College of Pharmacy and Research Institute of Pharmaceutical Sciences, Kyungpook National University, Daegu, Korea
- 4National Evidence-based Healthcare Collaborating Agency, Seoul, Korea
- 5Department of Surgery, Nowon Eulji Medical Center, Eulji University, Seoul, Korea
- 6Department of Surgery, Hanyang University College of Medicine, Seoul, Korea
- 7Department of Surgery, Soonchunhyang University Hospital, Seoul, Korea
- 8Department of Surgery, H+ Yangji Hospital, Seoul, Korea
- 9Department of Surgery, Keimyung University Dongsan Hospital, Daegu, Korea
- 10Department of Surgery, CHA Gangnam Medical Center, Seoul, Korea
- 11Department of Surgery, Cheil General Hospital, Seoul, Korea
- 12Department of Surgery, Asan Medical Center, Seoul, Korea
- 13Department of Surgery, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea
- 14Department of Surgery, Ajou University Hospital, Suwon, Korea
- 15Department of Family Medicine, Kangbook Samsung Hospital, Seoul, Korea
- 16Department of Surgery, Inha University Hospital, Incheon, Korea
- KMID: 2520650
- DOI: http://doi.org/10.4174/astr.2021.101.4.197
Abstract
- Purpose
The aim of this study was to show that bariatric surgery (BS) is more effective than medical therapy (MT) in Asian obese patients.
Methods
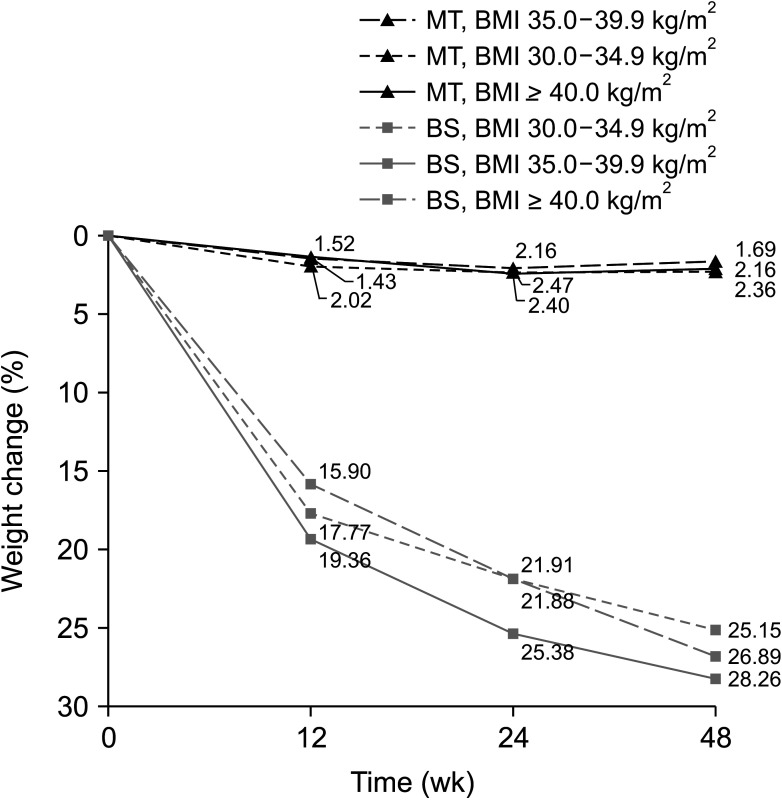
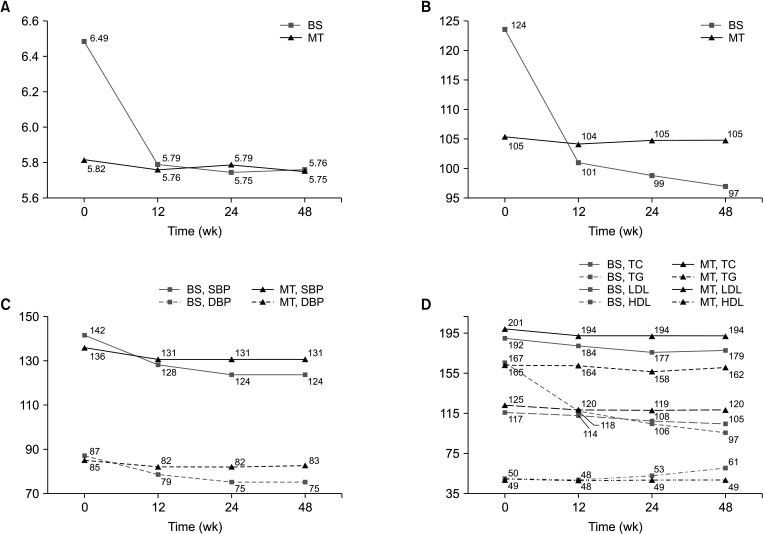
In this prospective, multicenter, nonrandomized, controlled trial, obese patients with body mass index of ≥35 kg/m2 or 30.0–34.9 kg/m2 with obesity-related comorbidities were assigned to undergo BS, such as laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass, or MT. Patients who underwent BS were evaluated 4, 12, 24, and 48 weeks after surgery, whereas patients who received MT were monitored at a hospital every 6 weeks for 1 year. At each visit, weight, waist and hip circumference, and blood pressure were measured, and patients underwent physical examination and laboratory testing. Health-related quality of life (HQOL) was investigated using Euro QOL-5 Dimension, Impact of Weight on Quality of Life questionnaire-Lite and Obesity-related Problems scale.
Results
The study included 264 patients from 13 institutions; of these, 64 underwent BS and 200 received MT. Of the patients who underwent BS, 6.3% experienced early complications. Relative weight changes from baseline to 48 weeks were significantly greater in the BS than in the MT group (26.9% vs. 2.1%, P < 0.001), as were the rates of remission of diabetes (47.8% vs. 16.7%, P = 0.014), hypertension (60.0% vs. 26.1%, P < 0.001), and dyslipidemia (63.2% vs. 22.0%, P < 0.001). HQOL was better in the BS than in the MT group at 48 weeks.
Conclusion
BS was safe and effective in Korean obese patients, with greater weight reduction, remission of comorbidities, and quality of life improvement than MT.
Keyword
Figure
Reference
-
1. Deurenberg-Yap M, Yian TB, Kai CS, Deurenberg P, VAN Staveren WA. Manifestation of cardiovascular risk factors at low levels of body mass index and waist-to-hip ratio in Singaporean Chinese. Asia Pac J Clin Nutr. 1999; 8:177–183. PMID: 24394159.
Article2. Low S, Clin MC, Ma S, Heng D, Deurenberg-Yap M. Rationale for redefining obesity in Asians. Ann Acad Med Singap. 2009; 38:66–69. PMID: 19221673.3. Shin HY, Kang HT. Recent trends in the prevalence of underweight, overweight, and obesity in Korean adults: the Korean National Health and Nutrition Examination Survey from 1998 to 2014. J Epidemiol. 2017; 27:413–419. PMID: 28420559.
Article4. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017; 390:2627–2642. PMID: 29029897.5. Celio AC, Pories WJ. A history of bariatric surgery: the maturation of a medical discipline. Surg Clin North Am. 2016; 96:655–667. PMID: 27473793.6. Phillips BT, Shikora SA. The history of metabolic and bariatric surgery: development of standards for patient safety and efficacy. Metabolism. 2018; 79:97–107. PMID: 29307519.
Article7. Umemura A, Lee WJ, Sasaki A, Wakabayashi G. History and current status of bariatric and metabolic surgeries in East Asia. Asian J Endosc Surg. 2015; 8:268–274. PMID: 25906817.
Article8. Heo YS, Park JM, Kim YJ, Kim SM, Park DJ, Lee SK, et al. Bariatric surgery versus conventional therapy in obese Korea patients: a multicenter retrospective cohort study. J Korean Surg Soc. 2012; 83:335–342. PMID: 23230551.
Article9. Puzziferri N, Roshek TB 3rd, Mayo HG, Gallagher R, Belle SH, Livingston EH. Long-term follow-up after bariatric surgery: a systematic review. JAMA. 2014; 312:934–942. PMID: 25182102.10. Raaijmakers LC, Pouwels S, Thomassen SE, Nienhuijs SW. Quality of life and bariatric surgery: a systematic review of short-and long-term results and comparison with community norms. Eur J Clin Nutr. 2017; 71:441–449. PMID: 27804961.11. Schauer PR, Kashyap SR, Wolski K, Brethauer SA, Kirwan JP, Pothier CE, et al. Bariatric surgery versus intensive medical therapy in obese patients with diabetes. N Engl J Med. 2012; 366:1567–1576. PMID: 22449319.
Article12. Lee YK, Nam HS, Chuang LH, Kim KY, Yang HK, Kwon IS, et al. South Korean time trade-off values for EQ-5D health states: modeling with observed values for 101 health states. Value Health. 2009; 12:1187–1193. PMID: 19659703.
Article13. Kolotkin RL, Crosby RD, Kosloski KD, Williams GR. Development of a brief measure to assess quality of life in obesity. Obes Res. 2001; 9:102–111. PMID: 11316344.
Article14. Sullivan M, Karlsson J, Sjöström L, Backman L, Bengtsson C, Bouchard C, et al. Swedish obese subjects (SOS): an intervention study of obesity. Baseline evaluation of health and psychosocial functioning in the first 1743 subjects examined. Int J Obes Relat Metab Disord. 1993; 17:503–512. PMID: 8220652.15. Gloy VL, Briel M, Bhatt DL, Kashyap SR, Schauer PR, Mingrone G, et al. Bariatric surgery versus non-surgical treatment for obesity: a systematic review and metaanalysis of randomised controlled trials. BMJ. 2013; 347:f5934. PMID: 24149519.
Article16. Haruta H, Kasama K, Ohta M, Sasaki A, Yamamoto H, Miyazaki Y, et al. Long-term outcomes of bariatric and metabolic surgery in Japan: results of a multi-institutional survey. Obes Surg. 2017; 27:754–762. PMID: 27631329.
Article17. Park CH, Nam SJ, Choi HS, Kim KO, Kim DH, Kim JW, et al. Comparative efficacy of bariatric surgery in the treatment of morbid obesity and diabetes mellitus: a systematic review and network metaanalysis. Obes Surg. 2019; 29:2180–2190. PMID: 31037599.
Article18. Sjostrom L. Review of the key results from the Swedish Obese Subjects (SOS) trial: a prospective controlled intervention study of bariatric surgery. J Intern Med. 2013; 273:219–234. PMID: 23163728.19. Fried M, Hainer V, Basdevant A, Buchwald H, Deitel M, Finer N, et al. Interdisciplinary European guidelines on surgery of severe obesity. Obes Facts. 2008; 1:52–59. PMID: 20054163.
Article20. Ryan DH, Kahan S. Guideline recommendations for obesity management. Med Clin North Am. 2018; 102:49–63. PMID: 29156187.
Article21. Courcoulas AP, Goodpaster BH, Eagleton JK, Belle SH, Kalarchian MA, Lang W, et al. Surgical vs medical treatments for type 2 diabetes mellitus: a randomized clinical trial. JAMA Surg. 2014; 149:707–715. PMID: 24899268.22. Hatoum IJ, Blackstone R, Hunter TD, Francis DM, Steinbuch M, Harris JL, et al. Clinical factors associated with remission of obesity-related comorbidities after bariatric surgery. JAMA Surg. 2016; 151:130–137. PMID: 26465084.
Article23. Adams TD, Davidson LE, Litwin SE, Kolotkin RL, LaMonte MJ, Pendleton RC, et al. Health benefits of gastric bypass surgery after 6 years. JAMA. 2012; 308:1122–1131. PMID: 22990271.
Article24. Park JY, Heo Y, Kim YJ, Park JM, Kim SM, Park DJ, et al. Long-term effect of bariatric surgery versus conventional therapy in obese Korean patients: a multicenter retrospective cohort study. Ann Surg Treat Res. 2019; 96:283–289. PMID: 31183332.
Article25. Sjöström L, Lindroos AK, Peltonen M, Torgerson J, Bouchard C, Carlsson B, et al. Lifestyle, diabetes, and cardiovascular risk factors 10 years after bariatric surgery. N Engl J Med. 2004; 351:2683–2693. PMID: 15616203.
Article26. Oh SH, Song HJ, Kwon JW, Park DJ, Lee YJ, Chun H, et al. The improvement of quality of life in patients treated with bariatric surgery in Korea. J Korean Surg Soc. 2013; 84:131–139. PMID: 23486845.
Article27. Falk V, Twells L, Gregory D, Murphy R, Smith C, Boone D, et al. Laparoscopic sleeve gastrectomy at a new bariatric surger y centre in Canada: 30-day complication rates using the Clavien-Dindo c lassi f icat ion. Can J Surg. 2016; 59:93–97. PMID: 27007089.28. Peterli R, Borbély Y, Kern B, Gass M, Peters T, Thurnheer M, et al. Early results of the Swiss Multicentre Bypass or Sleeve Study (SM-BOSS): a prospective randomized trial comparing laparoscopic sleeve gastrectomy and Roux-en-Y gastric bypass. Ann Surg. 2013; 258:690–695. PMID: 23989054.29. Peterli R, Wölnerhanssen BK, Vetter D, Nett P, Gass M, Borbély Y, et al. Laparoscopic sleeve gastrectomy versus Roux-Y-gastric bypass for morbid obesity-3-year outcomes of the prospective randomized Swiss Multicenter Bypass or Sleeve Study (SM-BOSS). Ann Surg. 2017; 265:466–473. PMID: 28170356.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Status of Bariatric and Metabolic Surgery in Korea
- Can Bariatric Surgery Be a Surgical Treatment to Prevent the Progression of Chronic Kidney Disease?
- A prospective randomized trial comparing the efficacy of temperature-responsive gel with local anesthetics versus local anesthetic infusion pump device for postoperative pain control after bariatric surgery
- Recent Advances in Sentinel Node Navigation Surgery for Early Gastric Cancer
- Impact of peritoneal vaginoplasty combined with radical hysterectomy on the quality of sexual life for patients with early-stage cervical cancer: trial protocol for a multi-center superiority randomized controlled trial