Clin Endosc.
2021 Sep;54(5):763-766. 10.5946/ce.2020.279.
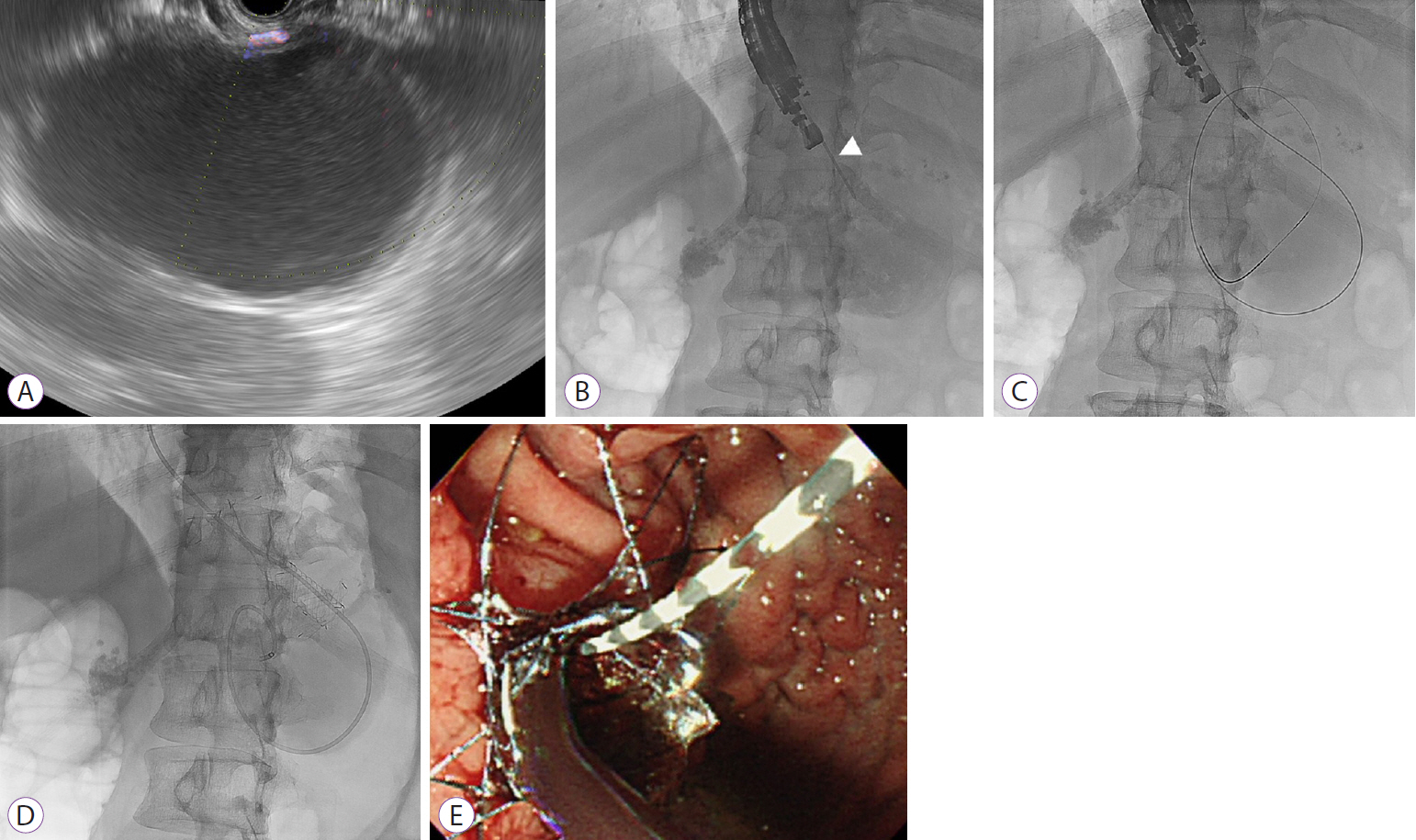
Successful Endoscopic Ultrasound-Guided Treatment of a Spontaneous Rupture of a Hemorrhagic Pancreatic Pseudocyst
- Affiliations
-
- 1Department of Surgery, Wonkwang University College of Medicine and Hospital, Iksan, Korea
- 2Department of Internal Medicine, Wonkwang University College of Medicine and Hospital, Iksan, Korea
- KMID: 2520562
- DOI: http://doi.org/10.5946/ce.2020.279
Abstract
- Spontaneous rupture of a hemorrhagic pancreatic pseudocyst may be life-threatening. Endoscopic ultrasound (EUS)-guided drainage has been reported to be a valuable treatment option for pancreatic pseudocysts. However, its usefulness in the management of a ruptured pancreatic pseudocyst is limited. We report a rare case of a spontaneous rupture of a hemorrhagic pancreatic pseudocyst in a patient with chronic pancreatitis, which was successfully treated with EUS-guided gastrocystostomy with a fully covered self-expandable metallic stent.
Figure
Reference
-
1. Song TJ, Lee SS. Endoscopic drainage of pseudocysts. Clin Endosc. 2014; 47:222–226.
Article2. Habashi S, Draganov PV. Pancreatic pseudocyst. World J Gastroenterol. 2009; 15:38–47.
Article3. Urakami A, Tsunoda T, Kubozoe T, Takeo T, Yamashita K, Imai H. Rupture of a bleeding pancreatic pseudocyst into the stomach. J Hepatobiliary Pancreat Surg. 2002; 9:383–385.
Article4. Hiraishi H, Terano A. Images in clinical medicine. Rupture of a pancreatic pseudocyst into the duodenum. N Engl J Med. 1999; 340:1411.5. Rocha R, Marinho R, Gomes A, et al. Spontaneous rupture of pancreatic pseudocyst: report of two cases. Case Rep Surg. 2016; 2016:7056567.
Article6. Patidar Y, Sureka B, Singh VP, Bansal K, Maiwall R. Spontaneous rupture of intrahepatic pseudocyst into the inferior vena cava. Gastroenterol Rep (Oxf). 2018; 6:225–227.
Article7. Mujer MT, Rai MP, Atti V, Shrotriya S. Spontaneous rupture of a pancreatic pseudocyst. BMJ Case Rep. 2018; 2018:bcr2018226296.
Article8. Alali A, Mosko J, May G, Teshima C. Endoscopic ultrasound-guided management of pancreatic fluid collections: update and review of the literature. Clin Endosc. 2017; 50:117–125.
Article9. Bang JY, Varadarajulu S. Metal versus plastic stent for transmural drainage of pancreatic fluid collections. Clin Endosc. 2013; 46:500–502.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Linear Array Endoscopic Ultrasound-Guided Drainage of a Pancreatic Pseudocyst without Using Fluoroscopy
- Endoscopic Ultrasound-Guided Drainage of Pancreatic Fluid Collections (with Video)
- A Case of Cystoduodenal and Cystocolic Fistula Complicated in Pancreatic Pseudocyst
- Angiographic diagnosis and treatment of a splenic artery pseudoaneurysm following endoscopic cystogastrostomy for a pancreatic pseudocyst
- Endoscopic Ultrasound-Guided Transesophageal Drainage of a Mediastinal Pancreatic Pseudocyst