Clin Endosc.
2021 Sep;54(5):754-758. 10.5946/ce.2021.060.
Management of Biliopancreatic Limb Bleeding after Roux-en-Y Gastric Bypass: A Case Report
- Affiliations
-
- 1School of Medicine, Pontificia Universidad Católica de Chile
- 2Department of Gastroenterology, School of Medicine, Pontificia Universidad Católica de Chile
- 3Department of Internal Medicine, School of Medicine, Pontificia Universidad Católica de Chile
- 4Department of Digestive Surgery, Division of Surgery, School of Medicine, Pontificia Universidad Católica de Chile
- 5Unit of Gastroenterology, Complejo Asistencial Dr. Sótero Del Río, Santiago, Chile
- KMID: 2520560
- DOI: http://doi.org/10.5946/ce.2021.060
Abstract
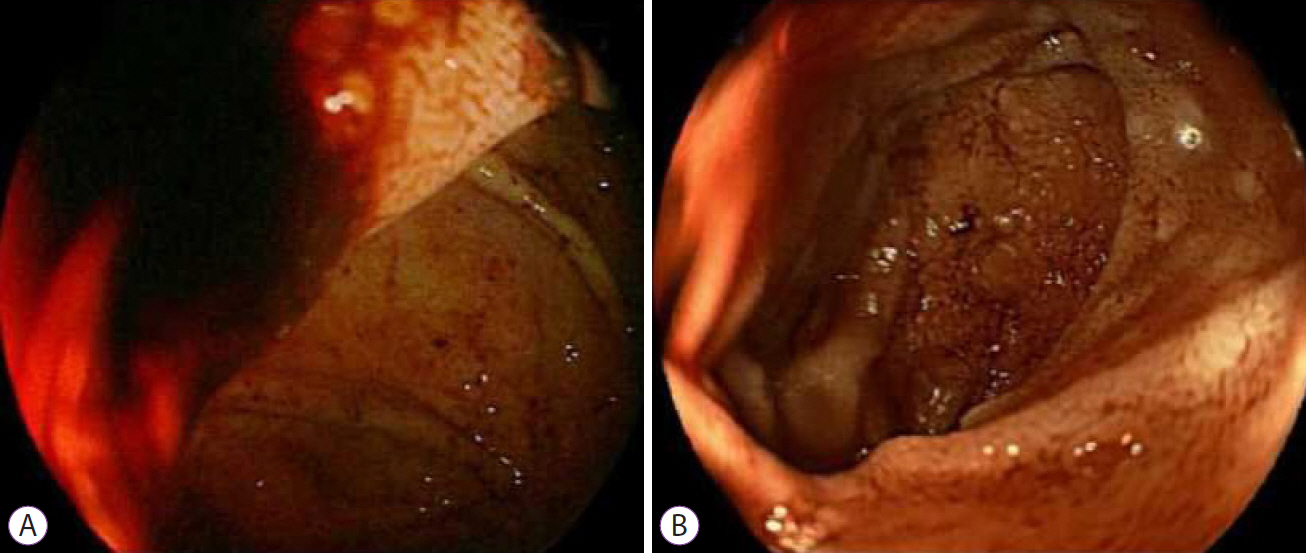
- The Roux-en-Y gastric bypass is one of the most extensive surgical treatments for obesity. The treatment of upper gastrointestinal bleeding after Roux-en-Y gastric bypass is complex due to the difficulty of accessing the excluded gastric antrum and duodenal bulb. There is no consensus regarding the management of this complication. While various techniques have been described to access the biliopancreatic limb, double-balloon enteroscopy is the most commonly used. If double-balloon enteroscopy is unavailable, a pediatric colonoscope may be used as an alternative; however, its use in such cases has not been described. We report the case of a 50-year-old male patient who underwent gastric bypass 13 years ago and was admitted for a second episode of upper gastrointestinal bleeding. The initial approach using upper endoscopy, colonoscopy, and abdominal computed tomography angiography did not reveal the cause of gastrointestinal hemorrhage; therefore, an endoscopic study of the biliopancreatic limb was performed using a pediatric colonoscope. A Forrest Ib ulcer was found in the duodenal bulb, and endoscopic therapy was administered. The evolution was found to be satisfactory.
Keyword
Figure
Cited by 1 articles
-
Endoscopic management of postoperative bleeding
Sung Hyeok Ryou, Ki Bae Bang
Clin Endosc. 2023;56(6):706-715. doi: 10.5946/ce.2023.028.
Reference
-
1. World Health Organization. Obesity and overweight [Internet]. Geneva: WHO;c2020. [updated 2020 Apr 1; cited 2021 Apr 2]. Available from: https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight.2. Coblijn UK, Karres J, de Raaff CAL, et al. Predicting postoperative complications after bariatric surgery: the Bariatric Surgery Index for Complications, BASIC. Surg Endosc. 2017; 31:4438–4445.
Article3. Hendrickson CM, Gibb SL, Miyazawa BY, et al. Elevated plasma levels of TIMP-3 are associated with a higher risk of acute respiratory distress syndrome and death following severe isolated traumatic brain injury. Trauma Surg Acute Care Open. 2018; 3:e000171.
Article4. Fernández-Esparrach G, Bordas JM, Pellisé M, et al. Endoscopic management of early GI hemorrhage after laparoscopic gastric bypass. Gastrointest Endosc. 2008; 67:552–555.
Article5. Heneghan HM, Meron-Eldar S, Yenumula P, Rogula T, Brethauer SA, Schauer PR. Incidence and management of bleeding complications after gastric bypass surgery in the morbidly obese. Surg Obes Relat Dis. 2012; 8:729–735.
Article6. Coblijn UK, Lagarde SM, Tuynman JB, van Meyel JJM, van Wagensveld BA. Delayed massive bleeding two years after Roux-en-Y gastric bypass. JSLS. 2013; 17:476–480.
Article7. García-García ML, Martín-Lorenzo JG, Torralba-Martínez JA, et al. Emergency endoscopy for gastrointestinal bleeding after bariatric surgery. therapeutic algorithm. Cir Esp. 2015; 93:97–104.
Article8. Gralnek IM, Dumonceau J-M, Kuipers EJ, et al. Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) guideline. Endoscopy. 2015; 47:a1–a46.
Article9. Skinner M, Peter S, Wilcox CM, Mönkemüller K. Diagnostic and therapeutic utility of double-balloon enteroscopy for obscure GI bleeding in patients with surgically altered upper GI anatomy. Gastrointest Endosc. 2014; 80:181–186.
Article10. Ali R, Wild D, Shieh F, et al. Deep enteroscopy with a conventional colonoscope: initial multicenter study by using a through-the-scope balloon catheter system. Gastrointest Endosc. 2015; 82:855–860.
Article11. Mahawar KK. Liver Dysfunction with both Roux-en-Y and one-anastomosis gastric bypass is almost exclusively seen with longer than standard limb lengths. Obes Surg. 2018; 28:548–549.
Article12. Issa H, Al-Saif O, Al-Momen S, Bseiso B, Al-Salem A. Bleeding duodenal ulcer after Roux-en-Y gastric bypass surgery: the value of laparoscopic gastroduodenoscopy. Ann Saudi Med. 2010; 30:67–69.
Article13. Zerey M, Sigmon LB, Kuwada TS, Heniford BT, Sing RF. Bleeding duodenal ulcer after roux-en-Y gastric bypass surgery. J Am Osteopath Assoc. 2008; 108:25–27.14. Palmer ED. The vigorous diagnostic approach to upper-gastrointestinal tract hemorrhage. A 23-year prospective study of 14,000 patients. JAMA. 1969; 207:1477–1480.
Article15. Seo JH, Hong SJ, Kim J-H, et al. Long-term recurrence rates of peptic ulcers without Helicobacter pylori. Gut Liver. 2016; 10:719–725.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous gastrostomy tube placement of the excluded gastric remnant after laparoscopic bariatric surgery in three patients
- A Clinical Study of the Uncut Roux-en-Y Gastrojejunostomy Using a Short Roux Limb after Subtotal Gastrectomy
- Gastric Cancer After Bariatric Surgeries
- Robotic Roux-en-Y Gastric Bypass and Robotic Sleeve Gastrectomy for Morbid Obesity: Case Reports
- A Peterson's hernia and subsequent small bowel volvulus: surgical reconstruction utilizing transverse colon as a new Roux-en-Y limb - 1 case