Korean J Gastroenterol.
2021 Sep;78(3):161-167. 10.4166/kjg.2021.040.
Early Cardiac Dysfunction in Biopsy-proven Nonalcoholic Fatty Liver Disease
- Affiliations
-
- 1Department of Medicine, Brooke Army Medical Center, San Antonio, TX, USA
- 2Department of Medicine, Uniformed Services University of Health Sciences, Bethesda, MD, USA
- 3Department of Medicine, Cardiology Service, Brooke Army Medical Center, San Antonio, TX, USA
- 4Pinnacle Clinical Research, San Antonio, TX, USA
- 5Department of Medicine, Gastroenterology and Hepatology Service, Brooke Army Medical Center, San Antonio, TX, USA
- 6US Army Institute for Surgical Research, San Antonio, TX, USA
- KMID: 2520357
- DOI: http://doi.org/10.4166/kjg.2021.040
Abstract
- Background/Aims
Nonalcoholic fatty liver disease (NAFLD) encompasses a range of diseases from nonalcoholic fatty liver (NAFL) to nonalcoholic steatohepatitis (NASH) and has been linked to cardiovascular disease and sub-clinical cardiac remodeling. This paper presents a retrospective study of biopsy-proven NAFL and NASH to examine the differences in subclinical cardiac remodeling.
Methods
Patients were recruited from an institutional repository of patients with liver-biopsy-confirmed NAFLD. Patients with a transthoracic echocardiogram (TTE) within 12 months of the liver biopsy were included. The parameters of the diastolic dysfunction were reviewed for the differences between NAFL and NASH as well as between the stages and grades of NASH.
Results
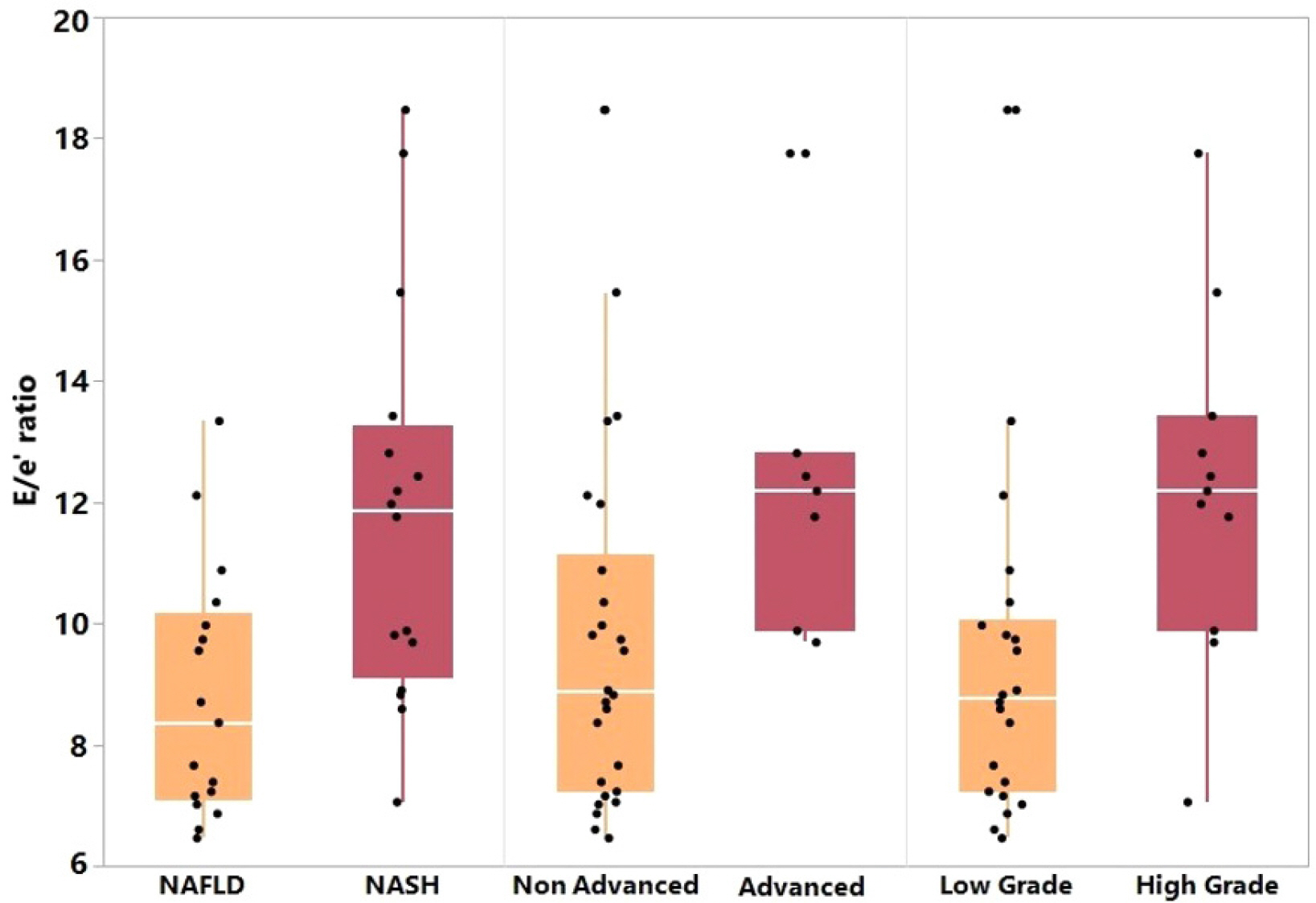
Thirty-three patients were included in the study, 17 with NAFL and 16 with NASH. The NASH patients were more likely to have lower platelets, higher AST, higher ALT, and higher rates of type 2 diabetes mellitus, coronary artery disease, and hypertension than the NAFL patients. The E/e’ ratio on transthoracic echocardiogram was significantly higher in NASH compared to NAFL, advanced-stage NASH compared to early stage, and high-grade NASH compared to low-grade. The E/e’ ratio was also significantly higher in NASH than NAFL in patients without diabetes mellitus. The presence of diastolic dysfunction trended toward significance. The other markers of diastolic dysfunction were similar. Logistic regression revealed a statistical association with E/e' and NASH.
Conclusions
NASH patients had evidence of a higher E/e’ ratio than NAFL, and there was a trend towards a significant diastolic dysfunction. Patients with NASH compared to NAFL should be closely monitored for signs and symptoms of cardiac dysfunction.
Keyword
Figure
Reference
-
1. Rinella ME. 2015; Nonalcoholic fatty liver disease: a systematic review. JAMA. 313:2263–2273. DOI: 10.1001/jama.2015.5370. PMID: 26057287.2. Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. 2016; Global epidemiology of nonalcoholic fatty liver disease-metaanalytic assessment of prevalence, incidence, and outcomes. Hepatology. 64:73–84. DOI: 10.1002/hep.28431. PMID: 26707365.
Article3. Younossi Z, Tacke F, Arrese M, et al. 2019; Global perspectives on nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Hepatology. 69:2672–2682. DOI: 10.1002/hep.30251. PMID: 30179269.
Article4. Lonardo A, Nascimbeni F, Mantovani A, Targher G. 2018; Hypertension, diabetes, atherosclerosis and NASH: cause or consequence? J Hepatol. 68:335–352. DOI: 10.1016/j.jhep.2017.09.021. PMID: 29122390.
Article5. Lonardo A, Lugari S, Ballestri S, Nascimbeni F, Baldelli E, Maurantonio M. 2019; A round trip from nonalcoholic fatty liver disease to diabetes: molecular targets to the rescue? Acta Diabetol. 56:385–396. DOI: 10.1007/s00592-018-1266-0. PMID: 30519965.
Article6. Loria P, Marchesini G, Nascimbeni F, et al. 2014; Cardiovascular risk, lipidemic phenotype and steatosis. A comparative analysis of cirrhotic and non-cirrhotic liver disease due to varying etiology. Atherosclerosis. 232:99–109. DOI: 10.1016/j.atherosclerosis.2013.10.030. PMID: 24401223.
Article7. Williams CD, Stengel J, Asike MI, et al. 2011; Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology. 140:124–131. DOI: 10.1053/j.gastro.2010.09.038. PMID: 20858492.
Article8. Hallsworth K, Hollingsworth KG, Thoma C, et al. 2013; Cardiac structure and function are altered in adults with non-alcoholic fatty liver disease. J Hepatol. 58:757–762. DOI: 10.1016/j.jhep.2012.11.015. PMID: 23178979.
Article9. Singh S, Allen AM, Wang Z, Prokop LJ, Murad MH, Loomba R. 2015; Fibrosis progression in nonalcoholic fatty liver vs nonalcoholic steatohepatitis: a systematic review and meta-analysis of paired-biopsy studies. Clin Gastroenterol Hepatol. 13:643–654.e1. quiz e39–40. DOI: 10.1016/j.cgh.2014.04.014. PMID: 24768810. PMCID: PMC4208976.
Article10. VanWagner LB, Wilcox JE, Colangelo LA, et al. 2015; Association of nonalcoholic fatty liver disease with subclinical myocardial remodeling and dysfunction: a population-based study. Hepatology. 62:773–783. DOI: 10.1002/hep.27869. PMID: 25914296. PMCID: PMC4549239.
Article11. Bonci E, Chiesa C, Versacci P, Anania C, Silvestri L, Pacifico L. 2015; Association of nonalcoholic fatty liver disease with subclinical cardiovascular changes: a systematic review and meta-analysis. Biomed Res Int. 2015:213737. DOI: 10.1155/2015/213737. PMID: 26273598. PMCID: PMC4529899.
Article12. Bhatia LS, Curzen NP, Calder PC, Byrne CD. 2012; Non-alcoholic fatty liver disease: a new and important cardiovascular risk factor? Eur Heart J. 33:1190–1200. DOI: 10.1093/eurheartj/ehr453. PMID: 22408036.
Article13. Karabay CY, Kocabay G, Kalayci A, et al. 2014; Impaired left ventricular mechanics in nonalcoholic fatty liver disease: a speckle-tracking echocardiography study. Eur J Gastroenterol Hepatol. 26:325–331. DOI: 10.1097/MEG.0000000000000008. PMID: 24161963.14. Petta S, Argano C, Colomba D, et al. 2015; Epicardial fat, cardiac geometry and cardiac function in patients with non-alcoholic fatty liver disease: association with the severity of liver disease. J Hepatol. 62:928–933. DOI: 10.1016/j.jhep.2014.11.030. PMID: 25445395.
Article15. Simon TG, Bamira DG, Chung RT, Weiner RB, Corey KE. 2017; Nonalcoholic steatohepatitis is associated with cardiac remodeling and dysfunction. Obesity (Silver Spring). 25:1313–1316. DOI: 10.1002/oby.21879. PMID: 28745025. PMCID: PMC5648006.
Article16. Chalasani N, Younossi Z, Lavine JE, et al. 2012; The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology. 55:2005–2023. DOI: 10.1002/hep.25762. PMID: 22488764.
Article17. Kleiner DE, Brunt EM, Van Natta M, et al. 2005; Nonalcoholic steatohepatitis clinical research network. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 41:1313–1321. DOI: 10.1002/hep.20701. PMID: 15915461.18. Nagueh SF, Smiseth OA, Appleton CP, et al. 2016; Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr. 29:277–314. DOI: 10.1016/j.echo.2016.01.011. PMID: 27037982.19. Jung JY, Park SK, Ryoo JH, et al. 2017; Effect of non-alcoholic fatty liver disease on left ventricular diastolic function and geometry in the Korean general population. Hepatol Res. 47:522–532. DOI: 10.1111/hepr.12770. PMID: 27379875.
Article20. Wijarnpreecha K, Lou S, Panjawatanan P, et al. 2018; Association between diastolic cardiac dysfunction and nonalcoholic fatty liver disease: a systematic review and meta-analysis. Dig Liver Dis. 50:1166–1175. DOI: 10.1016/j.dld.2018.09.004. PMID: 30292566.
Article21. Canada JM, Abbate A, Collen R, et al. 2019; Relation of hepatic fibrosis in nonalcoholic fatty liver disease to left ventricular diastolic function and exercise tolerance. Am J Cardiol. 123:466–473. DOI: 10.1016/j.amjcard.2018.10.027. PMID: 30502049. PMCID: PMC6331258.
Article22. Gaggini M, Morelli M, Buzzigoli E, DeFronzo RA, Bugianesi E, Gastaldelli A. 2013; Non-alcoholic fatty liver disease (NAFLD) and its connection with insulin resistance, dyslipidemia, atherosclerosis and coronary heart disease. Nutrients. 5:1544–1560. DOI: 10.3390/nu5051544. PMID: 23666091. PMCID: PMC3708335.
Article23. Francque SM, van der Graaff D, Kwanten WJ. 2016; Non-alcoholic fatty liver disease and cardiovascular risk: pathophysiological mechanisms and implications. J Hepatol. 65:425–443. DOI: 10.1016/j.jhep.2016.04.005. PMID: 27091791.
Article24. Belke DD, Betuing S, Tuttle MJ, et al. 2002; Insulin signaling coordinately regulates cardiac size, metabolism, and contractile protein isoform expression. J Clin Invest. 109:629–639. DOI: 10.1172/JCI0213946. PMID: 11877471. PMCID: PMC150890.
Article25. Lee YJ, Shim JY, Moon BS, et al. 2012; The relationship between arterial stiffness and nonalcoholic fatty liver disease. Dig Dis Sci. 57:196–203. DOI: 10.1007/s10620-011-1819-3. PMID: 21750929.
Article26. Zhou YY, Zhou XD, Wu SJ, et al. 2018; Nonalcoholic fatty liver disease contributes to subclinical atherosclerosis: a systematic review and meta-analysis. Hepatol Commun. 2:376–392. DOI: 10.1002/hep4.1155. PMID: 29619417. PMCID: PMC5880194.
Article27. Puchner SB, Lu MT, Mayrhofer T, et al. 2015; High-risk coronary plaque at coronary CT angiography is associated with nonalcoholic fatty liver disease, independent of coronary plaque and stenosis burden: results from the ROMICAT II trial. Radiology. 274:693–701. DOI: 10.1148/radiol.14140933. PMID: 25369449. PMCID: PMC4455680.
Article28. Targher G, Byrne CD, Lonardo A, Zoppini G, Barbui C. 2016; Non-alcoholic fatty liver disease and risk of incident cardiovascular disease: a meta-analysis. J Hepatol. 65:589–600. DOI: 10.1016/j.jhep.2016.05.013. PMID: 27212244.
Article29. Dulai PS, Singh S, Patel J, et al. 2017; Increased risk of mortality by fibrosis stage in nonalcoholic fatty liver disease: systematic review and meta-analysis. Hepatology. 65:1557–1565. DOI: 10.1002/hep.29085. PMID: 28130788. PMCID: PMC5397356.
Article30. Henson JB, Simon TG, Kaplan A, Osganian S, Masia R, Corey KE. 2020; Advanced fibrosis is associated with incident cardiovascular disease in patients with non-alcoholic fatty liver disease. Aliment Pharmacol Ther. 51:728–736. DOI: 10.1111/apt.15660. PMID: 32043602. PMCID: PMC7069774.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The crosstalk between insulin resistance and nonalcoholic fatty liver disease/metabolic dysfunction-associated fatty liver disease: a culprit or a consequence?
- Clinical and Histologic Features of Patients with Biopsy-Proven Metabolic Dysfunction-Associated Fatty Liver Disease
- Noninvasive serum biomarkers for liver steatosis in nonalcoholic fatty liver disease: Current and future developments
- The diagnosis of nonalcoholic fatty liver disease
- The Diagnosis of Nonalcoholic Fatty Liver Disease