J Korean Med Sci.
2021 Sep;36(36):e255. 10.3346/jkms.2021.36.e255.
The Comparison of Emergency Medical Service Responses to and Outcomes of Out-of-hospital Cardiac Arrest before and during the COVID-19 Pandemic in an Area of Korea
- Affiliations
-
- 1Department of Emergency Medicine, Gyeongsang National University College of Medicine, Gyeongsang National University Changwon Hospital, Changwon, Korea
- 2Department of Emergency Medicine, Dong-A University College of Medicine, Dong-A University Hospital, Busan, Korea
- 3Department of Emergency Medicine, University of Ulsan College of Medicine, Ulsan University Hospital, Ulsan, Korea
- 4Department of Emergency Medicine, Pusan National University College of Medicine, Pusan National University Yangsan Hospital, Busan, Korea
- 5Department of Emergency Medicine, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea
- 6Department of Emergency Medicine, Gyeongsang National University Hospital, Jinju, Korea
- 7Department of Emergency Medicine, Pusan National University College of Medicine, Pusan National University Hospital, Busan, Korea
- 8Department of Emergency Medicine, Inje University Haeundae Paik Hospital, Busan, Korea
- KMID: 2520111
- DOI: http://doi.org/10.3346/jkms.2021.36.e255
Abstract
- Background
Since the declaration of the coronavirus disease 2019 (COVID-19) pandemic, COVID-19 has affected the responses of emergency medical service (EMS) systems to cases of out-of-hospital cardiac arrest (OHCA). The purpose of this study was to identify the impact of the COVID-19 pandemic on EMS responses to and outcomes of adult OHCA in an area of South Korea.
Methods
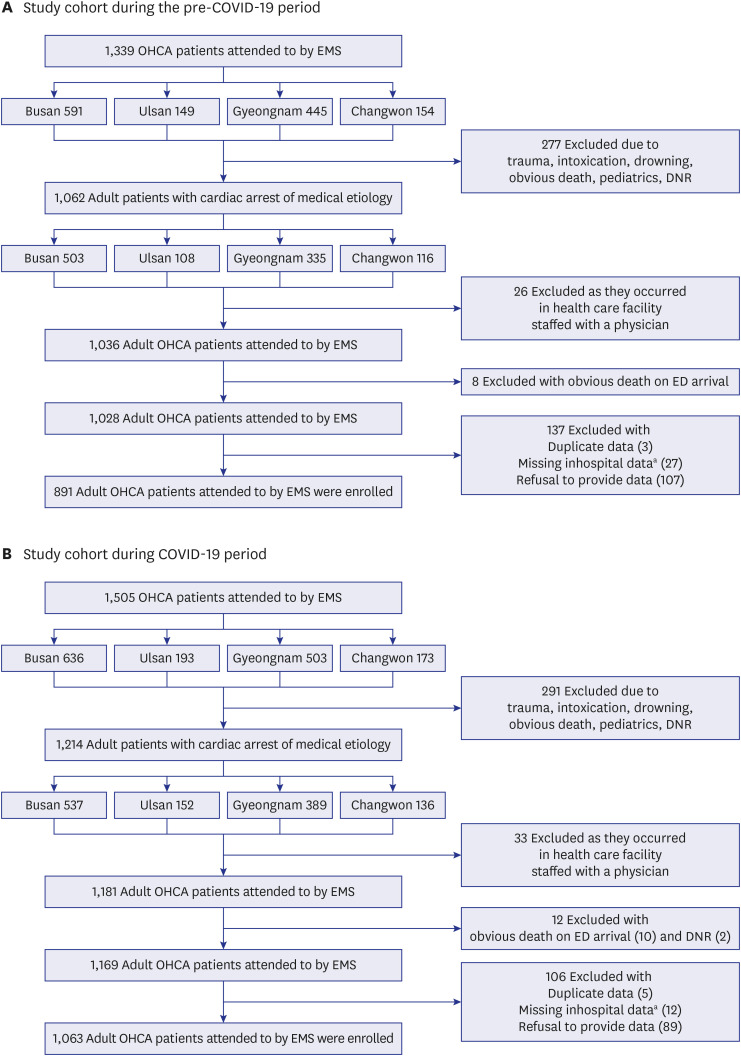
This was a retrospective observational study of adult OHCA patients attended by EMS providers comparing the EMS responses to and outcomes of adult OHCA during the COVID-19 pandemic to those during the pre-COVID-19 period. Propensity score matching was used to compare the survival rates, and logistic regression analysis was used to assess the impact of the COVID-19 pandemic on the survival of OHCA patients.
Results
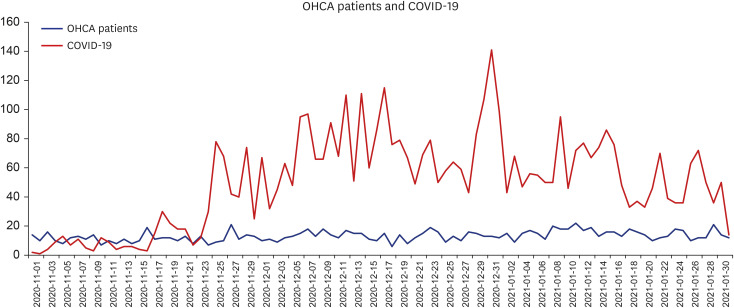
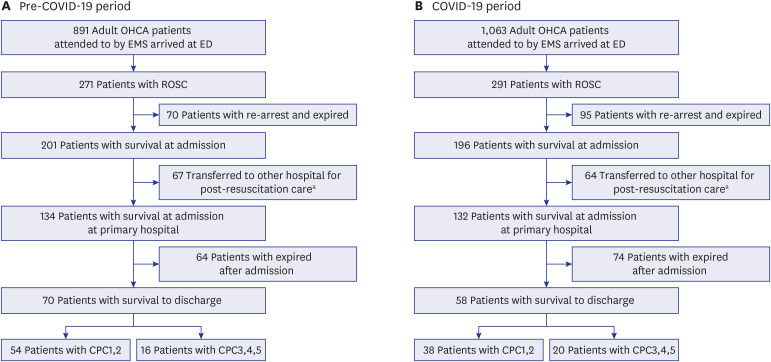
A total of 891 patients in the pre-COVID-19 group and 1,063 patients in the COVID-19 group were included in the final analysis. During the COVID-19 period, the EMS call time was shifted to a later time period (16:00–24:00, P < 0.001), and the presence of an initial shockable rhythm was increased (pre-COVID-19 vs. COVID-19, 7.97% vs. 11.95%, P = 0.004). The number of tracheal intubations decreased (5.27% vs. 1.22%, P < 0.001), and the use of mechanical chest compression devices (30.53% vs. 44.59%, P < 0.001) and EMS response time (median [quartile 1-quartile 3], 7 [5–10] vs. 8 [6–11], P < 0.001) increased. After propensity score matching, the survival at admission rate (22.52% vs. 18.24%, P = 0.025), survival to discharge rate (7.77% vs. 5.52%, P = 0.056), and favorable neurological outcome (5.97% vs. 3.49%, P < 0.001) decreased. In the propensity score matching analysis of the impact of COVID-19, odds ratios of 0.768 (95% confidence interval [CI], 0.592–0.995) for survival at admission and 0.693 (95% CI, 0.446–1.077) for survival to discharge were found.
Conclusion
During the COVID-19 period, there were significant changes in the EMS responses to OHCA. These changes are considered to be partly due to social distancing measures. As a result, the proportion of patients with an initial shockable rhythm in the COVID-19 period was greater than that in the pre-COVID-19 period, but the final survival rate and favorable neurological outcome were lower.
Figure
Reference
-
1. Hartley DM, Perencevich EN. Public health interventions for COVID-19: emerging evidence and implications for an evolving public health crisis. JAMA. 2020; 323(19):1908–1909. PMID: 32275299.2. Lange SJ, Ritchey MD, Goodman AB, Dias T, Twentyman E, Fuld J, et al. Potential indirect effects of the COVID-19 pandemic on use of emergency departments for acute life-threatening conditions—United States, January–May 2020. Wiley Online Library; 2020. MMWR Morb Mortal Wkly Rep. 2020; 69(25):795–800. PMID: 32584802.3. Sung HK, Paik JH, Lee YJ, Kang S. Impact of the COVID-19 outbreak on emergency care utilization in patients with acute myocardial infarction: a nationwide population-based study. J Korean Med Sci. 2021; 36(16):e111. PMID: 33904263.
Article4. Yoon D, Kim KE, Lee JE, Kim M, Kim JH. Impact of the coronavirus disease 2019 (COVID-19) pandemic on medical use of military hospitals in Korea. J Korean Med Sci. 2021; 36(28):e204. PMID: 34282607.
Article5. Baldi E, Sechi GM, Mare C, Canevari F, Brancaglione A, Primi R, et al. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med. 2020; 383(5):496–498. PMID: 32348640.
Article6. Chan PS, Girotra S, Tang Y, Al-Araji R, Nallamothu BK, McNally B. Outcomes for out-of-hospital cardiac arrest in the United States during the coronavirus disease 2019 pandemic. JAMA Cardiol. 2021; 6(3):296–303. PMID: 33188678.
Article7. Deakin CD. The chain of survival: not all links are equal. Resuscitation. 2018; 126:80–82. PMID: 29471008.
Article8. Elmer J, Okubo M, Guyette FX, Martin-Gill C. Indirect effects of COVID-19 on OHCA in a low prevalence region. Resuscitation. 2020; 156:282–283. PMID: 32920116.
Article9. Uy-Evanado A, Chugh HS, Sargsyan A, Nakamura K, Mariani R, Hadduck K, et al. Out-of-hospital cardiac arrest response and outcomes during the COVID-19 pandemic. JACC Clin Electrophysiol. 2021; 7(1):6–11. PMID: 33478713.
Article10. Marijon E, Karam N, Jost D, Perrot D, Frattini B, Derkenne C, et al. Out-of-hospital cardiac arrest during the COVID-19 pandemic in Paris, France: a population-based, observational study. Lancet Public Health. 2020; 5(8):e437–e443. PMID: 32473113.
Article11. World Health Organization. (COVID-19) dashboard. Updated 2021. Accessed May 12, 2021. https://covid19.who.int/table.12. Statistics Korea. Statistical geographic information service. Updated 2021. Accessed May 12, 2021. https://sgis.kostat.go.kr/view/index.13. Ro YS, Shin SD, Song KJ, Hong SO, Kim YT, Lee DW, et al. Public awareness and self-efficacy of cardiopulmonary resuscitation in communities and outcomes of out-of-hospital cardiac arrest: a multi-level analysis. Resuscitation. 2016; 102:17–24. PMID: 26898411.
Article14. National Fire Agency. Updated 2021. Accessed May 12, 2021. https://www.nfa.go.kr/nfa/news/pressrelease/press/?boardId.15. Edelson DP, Sasson C, Chan PS, Atkins DL, Aziz K, Becker LB, et al. Interim guidance for basic and advanced life support in adults, children, and neonates with suspected or confirmed COVID-19: from the emergency cardiovascular care committee and get with the guidelines-resuscitation adult and pediatric task forces of the American Heart Association. Circulation. 2020; 141(25):e933–e943. PMID: 32270695.
Article16. Korea Disease Control and Prevention Agency. Updated 2021. Accessed May 12, 2021. http://www.kdca.go.kr/index.es?sid=a3.17. Mak M, Moulaert VR, Pijls RW, Verbunt JA. Measuring outcome after cardiac arrest: construct validity of Cerebral Performance Category. Resuscitation. 2016; 100:6–10. PMID: 26744101.
Article18. Ball J, Nehme Z, Bernard S, Stub D, Stephenson M, Smith K. Collateral damage: Hidden impact of the COVID-19 pandemic on the out-of-hospital cardiac arrest system-of-care. Resuscitation. 2020; 156:157–163. PMID: 32961304.
Article19. Wallace SK, Abella BS, Shofer FS, Leary M, Agarwal AK, Mechem CC, et al. Effect of time of day on prehospital care and outcomes after out-of-hospital cardiac arrest. Circulation. 2013; 127(15):1591–1596. PMID: 23509060.
Article20. Lim D, Kim SC, Park SY, Rhu JH, Bae BK, Kim SH, et al. A survey on the perception of emergency medical services (EMS) providers and medical directors toward EMS provider's field skill proficiency. J Korean Soc Emerg Med. 2020; 31(4):401–419.21. Jung E, Park JH, Lee SY, Ro YS, Hong KJ, Song KJ, et al. Mechanical chest compression device for out-of-hospital cardiac arrest: a nationwide observational study. J Emerg Med. 2020; 58(3):424–431. PMID: 32178958.
Article22. Ageta K, Naito H, Yorifuji T, Obara T, Nojima T, Yamada T, et al. Delay in emergency medical service transportation responsiveness during the COVID-19 pandemic in a minimally affected region. Acta Med Okayama. 2020; 74(6):513–520. PMID: 33361871.23. Satty T, Ramgopal S, Elmer J, Mosesso VN, Martin-Gill C. EMS responses and non-transports during the COVID-19 pandemic. Am J Emerg Med. 2021; 42:1–8. PMID: 33429185.
Article24. Rajan S, Folke F, Hansen SM, Hansen CM, Kragholm K, Gerds TA, et al. Incidence and survival outcome according to heart rhythm during resuscitation attempt in out-of-hospital cardiac arrest patients with presumed cardiac etiology. Resuscitation. 2017; 114:157–163. PMID: 28087286.
Article25. Renkiewicz GK, Hubble MW, Wesley DR, Dorian PA, Losh MJ, Swain R, et al. Probability of a shockable presenting rhythm as a function of EMS response time. Prehosp Emerg Care. 2014; 18(2):224–230. PMID: 24400944.
Article26. Izawa J, Komukai S, Gibo K, Okubo M, Kiyohara K, Nishiyama C, et al. Pre-hospital advanced airway management for adults with out-of-hospital cardiac arrest: nationwide cohort study. BMJ. 2019; 364:l430. PMID: 30819685.
Article27. Brooks SC, Hassan N, Bigham BL, Morrison LJ. Mechanical versus manual chest compressions for cardiac arrest. Cochrane Database Syst Rev. 2014; (2):CD007260. PMID: 24574099.
Article28. Perkins GD, Lall R, Quinn T, Deakin CD, Cooke MW, Horton J, et al. Mechanical versus manual chest compression for out-of-hospital cardiac arrest (PARAMEDIC): a pragmatic, cluster randomised controlled trial. Lancet. 2015; 385(9972):947–955. PMID: 25467566.
Article29. Gates S, Quinn T, Deakin CD, Blair L, Couper K, Perkins GD. Mechanical chest compression for out of hospital cardiac arrest: systematic review and meta-analysis. Resuscitation. 2015; 94:91–97. PMID: 26190673.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Variance of the COVID-19 occurrence in the community: influence on the emergency medical service and the survival of out-of-hospital cardiac arrest patients
- The impact of COVID-19 through epidemiological changes in out-of-hospital cardiac arrest patients: a study in a single emergency medical center
- Epidemiology and Outcome of Out-of-Hospital Cardiac Arrests during the COVID-19 Pandemic in South Korea: A Systematic Review and Meta-Analyses
- Analysis of reasons for the termination of resuscitation in non-traumatic out-of-hospital cardiac arrests before and after the COVID-19 pandemic
- No frequency change of prehospital treatments by emergency medical services providers for traumatic cardiac arrest patients before and after the COVID-19 pandemic in Korea: an observational study