Ann Surg Treat Res.
2021 Sep;101(3):181-186. 10.4174/astr.2021.101.3.181.
Prevalence and risk factors associated with depressive mood in Korean patients with fecal incontinence
- Affiliations
-
- 1Hwanggeumbit Surgery Clinic, Daegu, Korea
- 2Department of Surgery, Yeungnam University College of Medicine, Daegu, Korea
- 3Department of Psychiatry, Yeungnam University College of Medicine, Daegu, Korea
- KMID: 2519848
- DOI: http://doi.org/10.4174/astr.2021.101.3.181
Abstract
- Purpose
The study was aimed at assessing the prevalence of depression in individuals with fecal incontinence (FI) and the relationship between the symptoms of depression and the severity of objective test parameters.
Methods
Patients with FI for over 3 months were included in the study. The exclusion criteria were (1) diagnosis or treatment of the pelvic organ prolapse syndrome, (2) previous anorectal surgery, (3) inflammatory bowel disease, (4) previous diagnosis of psychiatric disorder, and (5) inability to read or understand the questionnaire themselves. The questionnaire included the Beck Depression Inventory-II (BDI-II) for measuring depression, and 142 patients were included for analysis.
Results
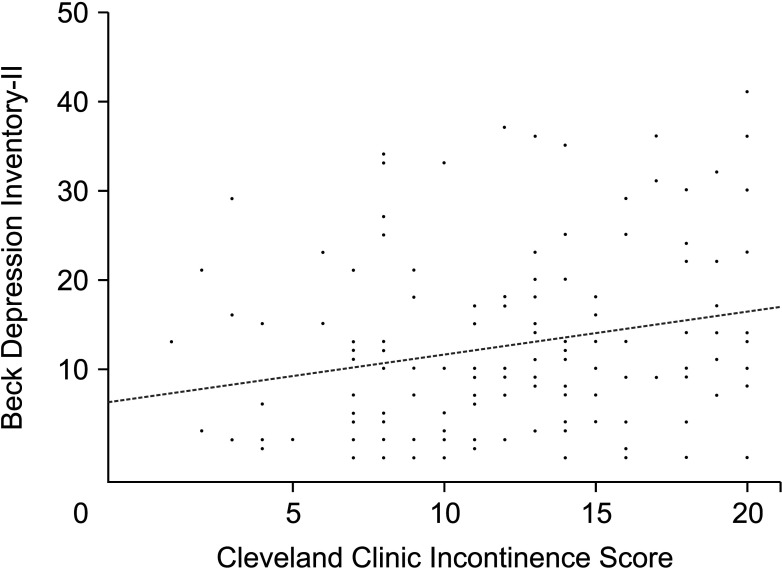
Of the 142 patients, 34 were males and 108 were females, with a mean age of 67.8 years. The mean duration of FI symptoms was 38.36 months (range, 3–600 months). The mean Cleveland Clinic Incontinence Score and BDI-II were 11.96 ± 4.76 and 12.46 ± 9.84, respectively. The Cleveland Clinic Incontinence Score showed a positive correlation with the BDI-II score (P = 0.005). Of the 142 patients, 99 showed minimal to mild BDI-II scores, and 43 showed moderate-to-severe BDI-II scores. The multivariable logistic regression analysis showed that health insurance status was related to the depression in FI patients.
Conclusion
Mood disorders related to FI are more affected by the severity of the subjective symptoms or the surrounding environment than the objective indicators derived from the test.
Figure
Reference
-
1. Rao SS. American College of Gastroenterology Practice Parameters Committee. Diagnosis and management of fecal incontinence. American College of Gastroenterology Practice Parameters Committee. Am J Gast roenterol. 2004; 99:1585–1604.2. Melville JL, Fan MY, Newton K, Fenner D. Fecal incontinence in US women: a population-based study. Am J Obstet Gynecol. 2005; 193:2071–2076. PMID: 16325618.
Article3. Ditah I, Devaki P, Luma HN, Ditah C, Njei B, Jaiyeoba C, et al. Prevalence, trends, and risk factors for fecal incontinence in United States adults, 2005-2010. Clin Gastroenterol Hepatol. 2014; 12:636–643. PMID: 23906873.
Article4. Nygaard I, Barber MD, Burgio KL, Kenton K, Meikle S, Schaffer J, et al. Prevalence of symptomatic pelvic floor disorders in US women. JAMA. 2008; 300:1311–1316. PMID: 18799443.
Article5. Wu JM, Hundley AF, Fulton RG, Myers ER. Forecasting the prevalence of pelvic floor disorders in US women: 2010 to 2050. Obstet Gynecol. 2009; 114:1278–1283. PMID: 19935030.6. Saldana Ruiz N, Kaiser AM. Fecal incontinence: challenges and solutions. World J Gastroenterol. 2017; 23:11–24. PMID: 28104977.7. Ghetti C, Lowder JL, Ellison R, Krohn MA, Moalli P. Depressive symptoms in women seeking surgery for pelvic organ prolapse. Int Urogynecol J. 2010; 21:855–860. PMID: 20333505.
Article8. Mazi B, Kaddour O, Al-Badr A. Depression symptoms in women with pelvic floor dysfunction: a case-control study. Int J Womens Health. 2019; 11:143–148. PMID: 30863189.9. Ai F, Deng M, Mao M, Xu T, Zhu L. Depressive symptoms screening in postmenopausal women with symptomatic pelvic organ prolapse. Menopause. 2018; 25:314–319. PMID: 29040216.
Article10. Gosselink MP, Adusumilli S, Gorissen KJ, Fourie S, Tuynman JB, Jones OM, et al. Laparoscopic ventral rectopexy for fecal incontinence associated with high-grade internal rectal prolapse. Dis Colon Rectum. 2013; 56:1409–1414. PMID: 24201396.
Article11. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961; 4:561–571. PMID: 13688369.
Article12. Beck AT, Steer RA, Ball R, Ranieri W. Comparison of Beck Depression Inventories -IA and -II in psychiatric outpatients. J Pers Assess. 1996; 67:588–597. PMID: 8991972.13. Nelson R, Norton N, Cautley E, Furner S. Community-based prevalence of anal incontinence. JAMA. 1995; 274:559–561. PMID: 7629985.
Article14. Szurszewski JH, Holt PR, Schuster M. Proceedings of a workshop entitled “Neuromus cul a r func t ion and dysfunction of the gastrointestinal tract in aging”. Dig Dis Sci. 1989; 34:1135–1146. PMID: 2545427.15. Joh HK, Seong MK, Oh SW. Fecal incontinence in elderly Koreans. J Am Geriatr Soc. 2010; 58:116–121. PMID: 20002514.
Article16. Mion F, Garros A, Brochard C, Vitton V, Ropert A, Bouvier M, et al. 3D high-definition anorectal manometry: values obtained in asymptomatic volunteers, fecal incontinence and chronic constipation: results of a prospective multicenter study (NOMAD). Neurogastroenterol Motil. 2017; 29:e13049.
Article17. Read NW, Bartolo DC, Read MG. Differences in anal function in patients with incontinence to solids and in patients with incontinence to liquids. Br J Surg. 1984; 71:39–42. PMID: 6689968.
Article18. Felt-Bersma RJ, Klinkenberg-Knol EC, Meuwissen SG. Anorectal function investigations in incontinent and continent patients: differences and discriminatory value. Dis Colon Rectum. 1990; 33:479–486. PMID: 2351000.19. Read NW, Harford WV, Schmulen AC, Read MG, Santa Ana C, Fordtran JS. A clinical study of patients with fecal incont inence and diarrhea. Gastroenterology. 1979; 76:747–756. PMID: 422003.20. Sun WM, Read NW, Donnelly TC. Anorectal function in incontinent patients with cerebrospinal disease. Gastroenterology. 1990; 99:1372–1379. PMID: 2210244.
Article21. Hawkins AT, Olariu AG, Savitt LR, Gingipally S, Wakamatsu MM, Pulliam S, et al. Impact of rising grades of internal rectal intussusception on fecal continence and symptoms of constipation. Dis Colon Rectum. 2016; 59:54–61. PMID: 26651113.
Article22. Nivatvongs S, Stern HS, Fryd DS. The length of the anal canal. Dis Colon Rectum. 1981; 24:600–601. PMID: 7318624.
Article23. Zutshi M, Salcedo L, Hammel J, Hull T. Anal physiology testing in fecal incontinence: is it of any value? Int J Colorectal Dis. 2010; 25:277–282. PMID: 19902225.
Article24. Specht JK. 9 Myths of incontinence in older adults: both clinicians and the over-65 set need to know more. Am J Nurs. 2005; 105:58–68.25. Bouchoucha M, Devroede G, Rompteaux P, Bejou B, Sabate JM, Benamouzig R. Clinical and psychological correlates of soiling in adult patients with functional gastrointestinal disorders. Int J Colorectal Dis. 2018; 33:1793–1797. PMID: 29987361.
Article26. Erdem N, Chu FM. Management of overactive bladder and urge urinary incontinence in the elderly patient. Am J Med. 2006; 119(3 Suppl 1):29–36. PMID: 16483866.
Article27. Brown JS, Vittinghoff E, Wyman JF, Stone KL, Nevitt MC, Ensrud KE, et al. Urinary incontinence: does it increase risk for falls and fractures?: study of Osteoporotic Fractures Research Group. J Am Geriatr Soc. 2000; 48:721–725. PMID: 10894308.28. Lorant V, Deliège D, Eaton W, Robert A, Philippot P, Ansseau M. Socioeconomic inequalities in depression: a meta-analysis. Am J Epidemiol. 2003; 157:98–112. PMID: 12522017.
Article