Korean Circ J.
2021 Sep;51(9):766-780. 10.4070/kcj.2021.0213.
Heart Failure Is Associated with Increased Risk of Long-Term Venous Thromboembolism
- Affiliations
-
- 1State Key Laboratory of Cardiovascular Disease, Heart Failure Center, Fuwai Hospital, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Beijing, China
- 2Department of Cardiology, The Affiliated Hospital at Shunde, Southern Medical University (the First People's Hospital of Shunde), Foshan, China
- 3State Key Laboratory of Organ Failure Research, Department of Cardiology, Nanfang Hospital, Southern Medical University, Guangzhou, China
- KMID: 2519837
- DOI: http://doi.org/10.4070/kcj.2021.0213
Abstract
- Background and Objectives
Venous thromboembolism (VTE), consisting of deep vein thrombosis (DVT) and pulmonary embolism (PE), is highly prevalent in in-hospital HF patients and contributes to worse prognoses. However, the risk of VTE in out-patients with HF in long-term period is controversial. This study aimed to evaluate the associations between HF and the risk of VTE in a long-term follow-up duration.
Methods
We searched for studies investigating the risk of VTE, PE, and DVT in patients with HF before April 15, 2020, in PubMed, MEDLINE, and Embase databases. Cohort studies and post hoc analysis of RCTs were eligible for inclusion if they reported relative risk of VTE, DVT or PE in patients with HF in more than 3-month follow-up period.
Results
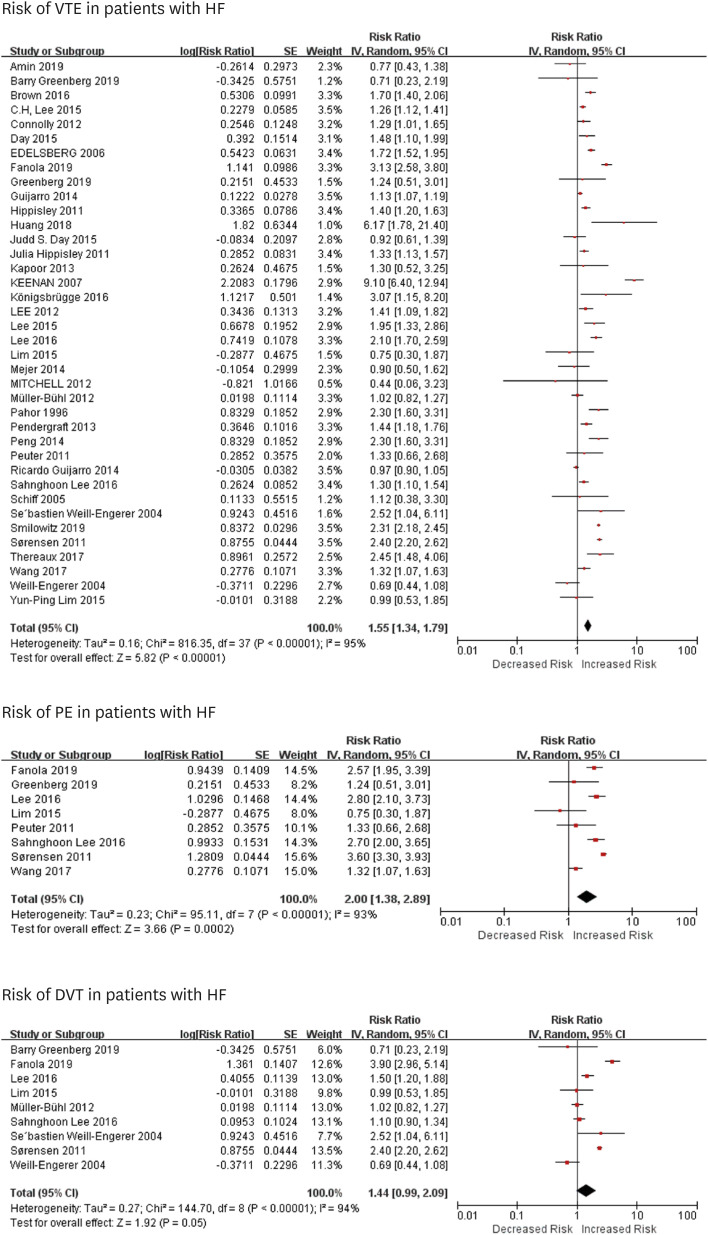
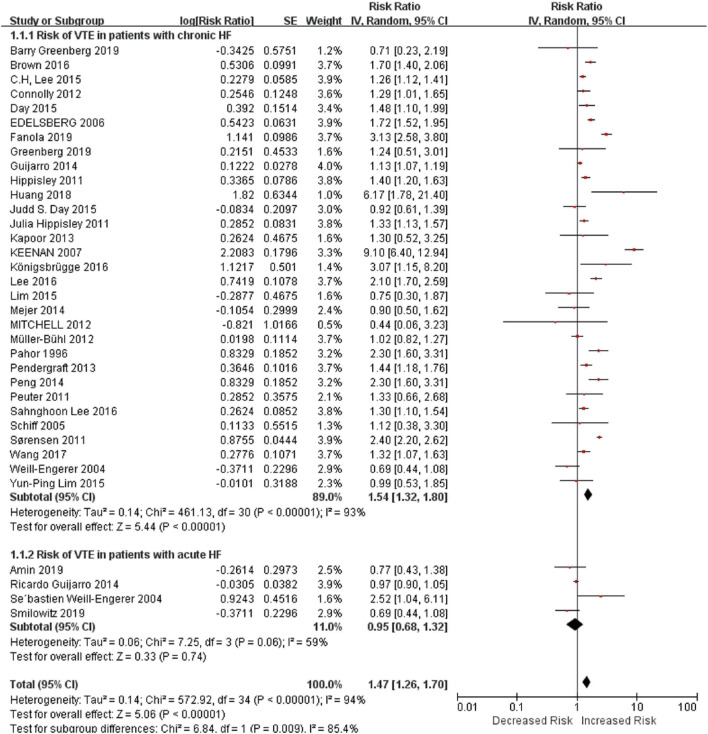
We identified 31 studies that enrolled over 530,641 HF patients. Overall, patients with HF were associated with an increased risk of VTE (risk ratio [RR]=1.57, 95% confidence interval [CI]=1.34–1.84) and PE (RR=2.00, 95% CI=1.38–2.89). However, the risk of DVT was not significantly increased in HF patients (RR=1.33, 95% CI=0.67–2.63). Subgroup analysis showed that patients with chronic HF (RR=1.54, 95% CI=1.32–1.80) had a higher risk of VTE than those with acute HF (RR=0.95, 95% CI=0.68–1.32).
Conclusions
In conclusion, HF was an independent risk for VTE and PE but not DVT in a longterm follow-up period. Patients with chronic HF were prone to suffer from VTE than acute HF.
Keyword
Figure
Cited by 1 articles
-
Venous Thromboembolism in Heart Failure Patients: Building Evidence towards Better Care and the Need for Precision
Seung-Pyo Lee
Korean Circ J. 2021;51(9):781-783. doi: 10.4070/kcj.2021.0244.
Reference
-
1. Ambrosy AP, Fonarow GC, Butler J, et al. The global health and economic burden of hospitalizations for heart failure: lessons learned from hospitalized heart failure registries. J Am Coll Cardiol. 2014; 63:1123–1133. PMID: 24491689.2. Hao G, Wang X, Chen Z, et al. Prevalence of heart failure and left ventricular dysfunction in China: the China Hypertension Survey, 2012-2015. Eur J Heart Fail. 2019; 21:1329–1337. PMID: 31746111.
Article3. Khera R, Dharmarajan K, Krumholz HM. Rising mortality in patients with heart failure in the United States: facts versus fiction. JACC Heart Fail. 2018; 6:610–612. PMID: 29914774.4. Alikhan R, Cohen AT, Combe S, et al. Prevention of venous thromboembolism in medical patients with enoxaparin: a subgroup analysis of the MEDENOX study. Blood Coagul Fibrinolysis. 2003; 14:341–346. PMID: 12945875.5. Cohen AT, Davidson BL, Gallus AS, et al. Efficacy and safety of fondaparinux for the prevention of venous thromboembolism in older acute medical patients: randomised placebo controlled trial. BMJ. 2006; 332:325–329. PMID: 16439370.
Article6. Tang L, Wu YY, Lip GY, Yin P, Hu Y. Heart failure and risk of venous thromboembolism: a systematic review and meta-analysis. Lancet Haematol. 2016; 3:e30–44. PMID: 26765646.
Article7. Klein L, O'connell JB. Thromboembolic risk in the patient with heart failure. Curr Treat Options Cardiovasc Med. 2007; 9:310–317. PMID: 17761116.
Article8. Fanola CL, Norby FL, Shah AM, et al. Incident heart failure and long-term risk for venous thromboembolism. J Am Coll Cardiol. 2020; 75:148–158. PMID: 31948643.9. Greenberg B, Neaton JD, Anker SD, et al. Association of rivaroxaban with thromboembolic events in patients with heart failure, coronary disease, and sinus rhythm: a post hoc analysis of the COMMANDER HF trial. JAMA Cardiol. 2019; 4:515–523. PMID: 31017637.10. Lim YP, Lin CL, Hung DZ, Ma WC, Lin YN, Kao CH. Increased risk of deep vein thrombosis and pulmonary thromboembolism in patients with organophosphate intoxication: a nationwide prospective cohort study. Medicine (Baltimore). 2015; 94:e341. PMID: 25569651.11. Stroup DF, Berlin JA, Morton SC, et al. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. 2000; 283:2008–2012. PMID: 10789670.12. Huang Y, Cai X, Mai W, Li M, Hu Y. Association between prediabetes and risk of cardiovascular disease and all cause mortality: systematic review and meta-analysis. BMJ. 2016; 355:i5953. PMID: 27881363.
Article13. Deeks JJ, Higgins JP, Altman DG. Chapter 10. Analysing data and undertaking meta-analyses. Higgins JP, Thomas J, Chandler J, editors. Cochrane Handbook for Systematic Reviews of Interventions. London: Cochrane Collaboration;2019. p. 241–284. DOI: 10.1002/9781119536604.ch10.14. Ng TM, Tsai F, Khatri N, Barakat MN, Elkayam U. Venous thromboembolism in hospitalized patients with heart failure: incidence, prognosis, and prevention. Circ Heart Fail. 2010; 3:165–173. PMID: 20086221.15. Heit JA. Epidemiology of venous thromboembolism. Nat Rev Cardiol. 2015; 12:464–474. PMID: 26076949.
Article16. Rokosh RS, Ranganath N, Yau P, et al. High prevalence and mortality associated with upper extremity deep venous thrombosis in hospitalized patients at a tertiary care center. Ann Vasc Surg. 2020; 65:55–65. PMID: 31669473.
Article17. Citla Sridhar D, Abou-Ismail MY, Ahuja SP. Central venous catheter-related thrombosis in children and adults. Thromb Res. 2020; 187:103–112. PMID: 31981840.
Article18. Yang H, Chen F, Jiao H, et al. Management of tunneled-cuffed catheter-related right atrial thrombosis in hemodialysis patients. J Vasc Surg. 2018; 68:1491–1498. PMID: 29804743.
Article19. Suratkal V, Ahmed A. Right atrial thrombus and challenges in its management. J Assoc Physicians India. 2018; 66:65–68. PMID: 31313553.20. Zghaib T, Bourfiss M, van der Heijden JF, et al. Atrial dysfunction in arrhythmogenic right ventricular cardiomyopathy. Circ Cardiovasc Imaging. 2018; 11:e007344. PMID: 30354672.
Article21. Long B, Robertson J, Koyfman A, Brady W. Left ventricular assist devices and their complications: a review for emergency clinicians. Am J Emerg Med. 2019; 37:1562–1570. PMID: 31072684.
Article22. Beemath A, Stein PD, Skaf E, Al Sibae MR, Alesh I. Risk of venous thromboembolism in patients hospitalized with heart failure. Am J Cardiol. 2006; 98:793–795. PMID: 16950187.
Article23. Darze ES, Latado AL, Guimarães AG, et al. Incidence and clinical predictors of pulmonary embolism in severe heart failure patients admitted to a coronary care unit. Chest. 2005; 128:2576–2580. PMID: 16236926.
Article24. Rogers C, Bush N. Heart failure: pathophysiology, diagnosis, medical treatment guidelines, and nursing management. Nurs Clin North Am. 2015; 50:787–799. PMID: 26596665.25. Ponikowski P, Voors AA, Anker SD, et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016; 37:2129–2200. PMID: 27206819.26. Harjola VP, Mullens W, Banaszewski M, et al. Organ dysfunction, injury and failure in acute heart failure: from pathophysiology to diagnosis and management. A review on behalf of the Acute Heart Failure Committee of the Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur J Heart Fail. 2017; 19:821–836. PMID: 28560717.
Article27. Goldhaber SZ. Venous thromboembolism in heart failure patients: pathophysiology, predictability, prevention. J Am Coll Cardiol. 2020; 75:159–162. PMID: 31948644.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Long-haul Air Travel; One of the Venous Thromboembolism Risk Factors
- Clinical Year in Review of Venous Thromboembolism
- Knowledge, Awareness and Risk of Occurrence of Venous Thromboembolism of Perinatal Women
- A case of huge thrombi in right atrium for taking bed rest after percutaneous coronary intervention
- Acute Pulmonary Embolism due to Thrombus-in-Transit in the Right Atrium During Bipolar Endoprosthesis of the Hip