J Korean Neurosurg Soc.
2021 Sep;64(5):776-783. 10.3340/jkns.2020.0348.
Adolescent Idiopathic Scoliosis Treated by Posterior Spinal Segmental Instrumented Fusion : When Is Fusion to L3 Stable?
- Affiliations
-
- 1Department of Neurosurgery, Spine Center, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
- 2Department of Orthopaedic Surgery, Spine Service, Columbia University College of Physicians and Surgeons, New York, NY, USA
- 3Department of Orthopaedic Surgery, Seoul Bumin Hospital, Seoul, Korea
- 4Department of Orthopaedic Surgery, Washington University School of Medicine, St. Louis, MO, USA
- KMID: 2519704
- DOI: http://doi.org/10.3340/jkns.2020.0348
Abstract
Objective
: The purpose of this study was to identify risk factors for distal adding on (AO) or distal junctional kyphosis (DJK) in adolescent idiopathic scoliosis (AIS) treated by posterior spinal fusion (PSF) to L3 with a minimum 2-year follow-up.
Methods
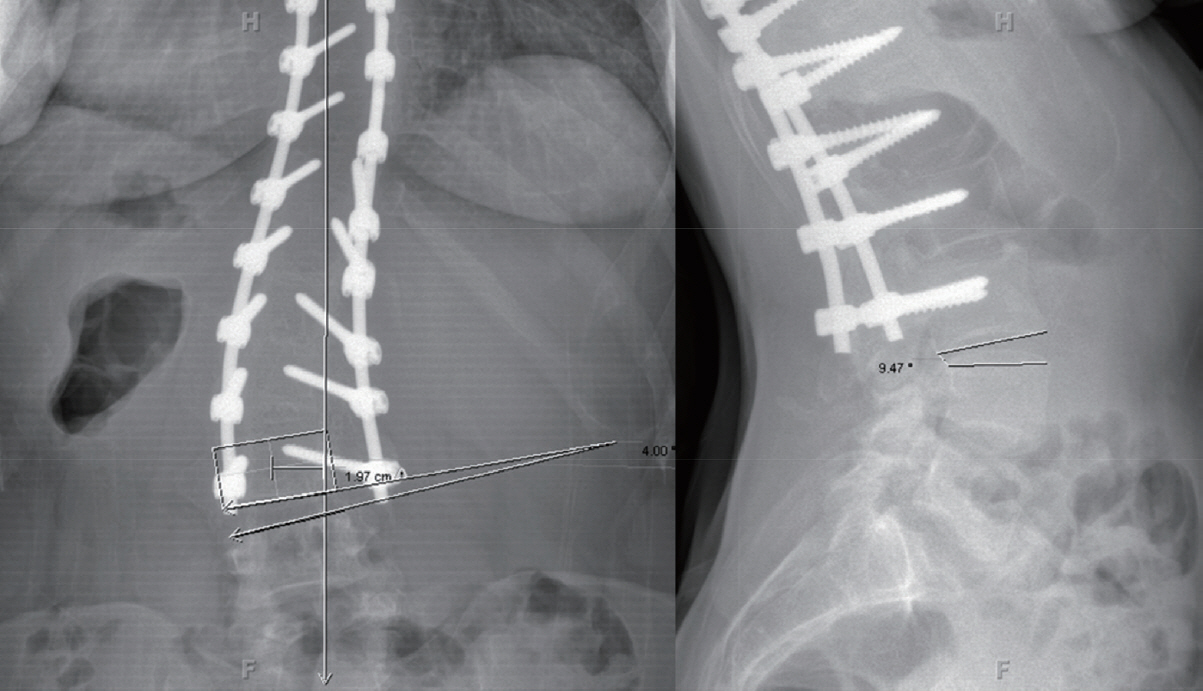
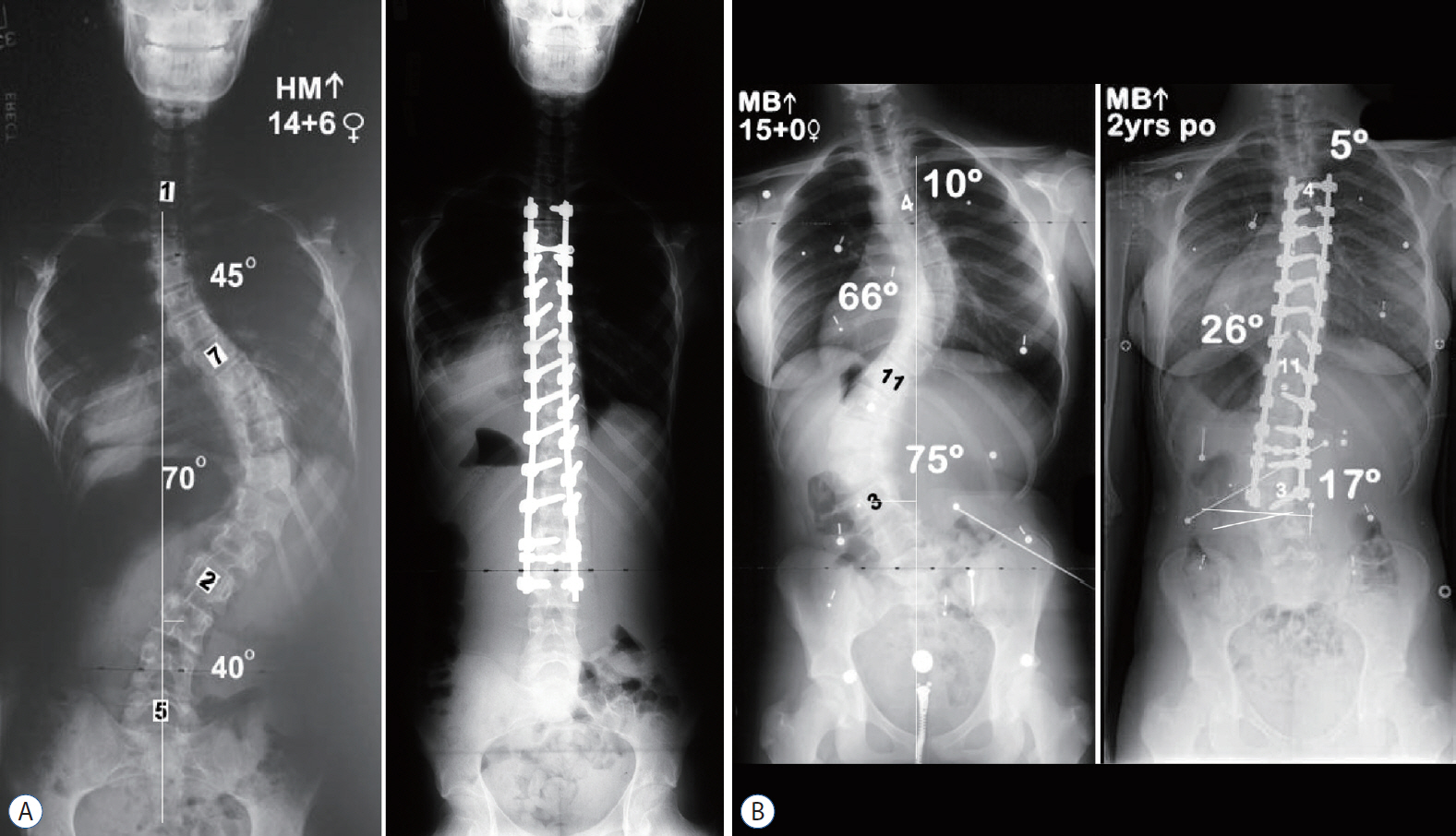
: AIS patients undergoing PSF to L3 by two senior surgeons from 2000–2010 were analyzed. Distal AO and DJK were deemed poor radiographic results and defined as >3 cm of deviation from L3 to the center sacral vertical line (CSVL), or >10° angle at L3–4 on the posterior anterior- or lateral X-ray at ultimate follow-up. New stable vertebra (SV) and neutral vertebra (NV) scores were defined for this study. The total stability (TS) score was the sum of the SV and NV scores.
Results
: Ten of 76 patients (13.1%) were included in the poor radiographic outcome group. The other 66 patients were included in the good radiographic outcome group. Lower Risser grade, more SV-3 (CSVL doesn’t touch the lowest instrumented vertebra [LIV]) on standing and side bending films, lesser NV and TS score, rigid L3–4 disc, more rotation and deviation of L3 were identified risk factors for AO or DJK. Age, number of fused vertebrae, curve correction, preoperative coronal/sagittal L3–4 disc angle did not differ significantly between the two groups. Multiple logistic regression results indicated that preoperative Risser grade 0, 1 (odds ratio [OR], 1.8), SV-3 at L3 in standing and side benders (OR, 2.1 and 2.8, respectively), TS score -5, -6 at L3 (OR, 4.4), rigid disc at L3–4 (OR, 3.1), LIV rotation >15° (OR, 2.9), and LIV deviation >2 cm from CSVL (OR, 2.2) were independent predictive factors. Although there was significant improvement of the of Scoliosis Research Society-22 average scores only in the good radiographic outcome group, there was no significant difference in the scores between the groups.
Conclusion
: The prevalence of AO or DJK at ultimate follow-up for AIS with LIV at L3 was 13.1%. To prevent AO or DJK following fusion to L3, we recommend that the CSVL touch L3 in both standing and side bending, TS score is -4 or less, the L3/4 disc is flexible, L3 is neutral (<15°) and ≤2 cm from the midline and the patient is ≥ Risser 2.
Keyword
Figure
Cited by 1 articles
-
Pediatric Spine Trauma
Sungjae An, Seung-Jae Hyun
J Korean Neurosurg Soc. 2022;65(3):361-369. doi: 10.3340/jkns.2021.0282.
Reference
-
References
1. Harrington PR. Treatment of scoliosis. Correction and internal fixation by spine instrumentation. J Bone Joint Surg Am. 44-A:591–610. 1962.2. Hasler CC, Hefti F, Büchler P. Coronal plane segmental flexibility in thoracic adolescent idiopathic scoliosis assessed by fulcrum-bending radiographs. Eur Spine J. 19:732–738. 2010.
Article3. Kim CW, Hyun SJ, Kim KJ. Surgical impact on global sagittal alignment and health-related quality of life following cervical kyphosis correction surgery: systematic review. Neurospine. 17:497–504. 2020.
Article4. Kim YJ, Fischer CR, Lenke LG, Bridwell KH, Boachie-Adjei O, Clement JL, et al. Optimal lowest instrumented vertebra to avoid adding‐on or distal junctional kyphosis for thoracic adolescent idiopathic scoliosis. In : Scoliosis Research Society 46th Annual Meeting; 2011 Sep 14-17; Louisville, KY. Podium presentation 88.5. King HA, Moe JH, Bradford DS, Winter RB. The selection of fusion levels in thoracic idiopathic scoliosis. J Bone Joint Surg Am. 65:1302–1313. 1983.
Article6. Lee SH, Hyun SJ, Jain A. Cervical sagittal alignment: literature review and future directions. Neurospine. 17:478–496. 2020.
Article7. Lenke LG, Betz RR, Harms J, Bridwell KH, Clements DH, Lowe TG, et al. Adolescent idiopathic scoliosis: a new classification to determine extent of spinal arthrodesis. J Bone Joint Surg Am. 83:1169–1181. 2001.8. Lenke LG, Braun JT, Bridwell KH, Dimar JR, Dobbs M, Glassman S, et al. Reliability analysis of end, neutral, stable, and lowest instrumented vertebrae selection in adolescent idiopathic scoliosis: Surgeon versus digital software determination. In : 12th International Meeting on Advanced Spine Techniques; 2005 Jul 7-9; Banff, Canada. Podium presentation 46.9. Lenke LG, Bridwell KH, Baldus C, Blanke K, Schoenecker PL. Ability of Cotrel-Dubousset instrumentation to preserve distal lumbar motion segments in adolescent idiopathic scoliosis. J Spinal Disord. 6:339–350. 1993.
Article10. Lenke LG, Newton PO, Lehman RA, Kelly MP, Clements DH, Errico TJ, et al. Radiographic results of selecting the touched vertebra as the lowest instrumented vertebra in Lenke 1A AIS curves at a minimum five-year follow up. In : Scoliosis Research Society 49th Annual Meeting; 2014 Sep 11-13; Anchorage, AK. Podium presentation 5.11. Park BJ, Hyun SJ, Wui SH, Jung JM, Kim KJ, Jahng TA. Surgical outcomes and complications following all posterior approach for spinal deformity associated with neurofibromatosis type-1. J Korean Neurosurg Soc. 63:738–746. 2020.
Article12. Perdriolle R, Vidal J. Morphology of scoliosis: three-dimensional evolution. Orthopedics. 10:909–915. 1987.
Article13. Qin X, Sun W, Xu L, Liu Z, Qiu Y, Zhu Z. Selecting the last “substantially” touching vertebra as lowest instrumented vertebra in Lenke type 1A curve: radiographic outcomes with a minimum of 2-year follow-up. Spine (Phila Pa 1976). 41:E742–E750. 2016.14. Suk SI, Lee SM, Chung ER, Kim JH, Kim WJ, Sohn HM. Determination of distal fusion level with segmental pedicle screw fixation in single thoracic idiopathic scoliosis. Spine (Phila Pa 1976). 28:484–491. 2003.
Article15. Wang Y, Hansen ES, Høy K, Wu C, Bünger CE. Distal adding-on phenomenon in Lenke 1A scoliosis: risk factor identification and treatment strategy comparison. Spine (Phila Pa 1976). 36:1113–1122. 2011.16. Wui SH, Hyun SJ, Kang B, Kim KJ, Jahng TA, Kim HJ. Bicortical screw purchase at upper instrumented vertebra (UIV) can cause UIV fracture after adult spinal deformity surgery: a finite element analysis study. Neurospine. 17:377–383. 2020.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Commentary on “The Incidence of Adding-On or Distal Junctional Kyphosis in Adolescent Idiopathic Scoliosis Treated by Anterior Spinal Fusion to L3 Was Significantly Higher Than by Posterior Spinal Fusion to L3”
- The Incidence of Adding-On or Distal Junctional Kyphosis in Adolescent Idiopathic Scoliosis Treated by Anterior Spinal Fusion to L3 Was Significantly Higher Than by Posterior Spinal Fusion to L3
- Indications of Proximal Thoracic Curve Fusion in Thoracic Adolescent Idiopathic Scoliosis(AIS): Recognition and Treatment of Double Thoracic Curve Pattern in Adolescent Idiopathic Scoliosis Treated with Segmental Instrumentation
- The Influence of Segmental Pedicle Screw Fixation on Distal Fusion Level in KingType I Adolescent Idiopathic Scoliosis(AIS)
- Selection of Fusion Level for Adolescent Idiopathic Scoliosis Surgery : Selective Fusion versus Postoperative Decompensation