Ann Rehabil Med.
2021 Aug;45(4):294-303. 10.5535/arm.21037.
The Association Between Sagittal Plane Alignment and Disc Space Narrowing of Lumbar Spine in Farmers
- Affiliations
-
- 1Department of Rehabilitation Medicine, Kangwon National University School of Medicine, Chuncheon, Korea
- 2Center for Farmers’ Safety and Health and Department of Rehabilitation Medicine, Kangwon National University Hospital, Chuncheon, Korea
- 3Human Medical Imaging and Intervention Center, Seoul, Korea
- KMID: 2519636
- DOI: http://doi.org/10.5535/arm.21037
Abstract
Objective
To investigate whether lumbar lordosis (LL) and lumbar segmental lordosis (LSL) are related to sex, age, low back pain (LBP), and lumbar disc space narrowing (DSN).
Methods
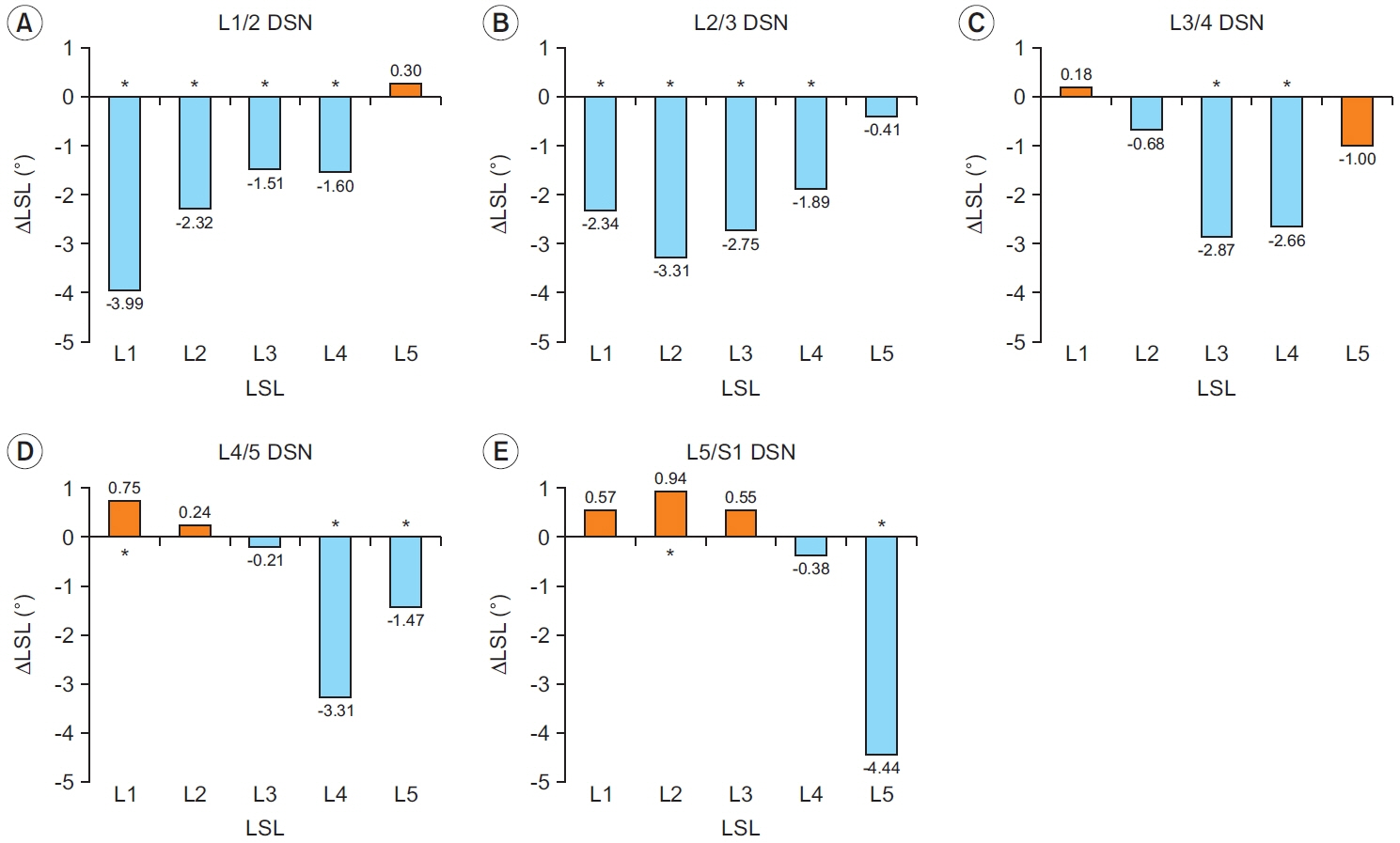
A total of 569 farmers were recruited. In lateral spine radiograph, LL (L1–L5) and LSL (L1, L2, L3, L4, and L5) were measured using Cobb’s method. The differences in LSL values (ΔLSL) according to the presence or absence of a DSN were calculated as LSLDSN – LSLnoDSN for each DSN level.
Results
In male, the lateral spine radiograph showed significantly greater L4-LSL and L5-LSL and smaller L1-LSL and L2-LSL compared to female. LLs in the 50–59 and ≥60 years age groups were significantly smaller compared to those in the <50 years age group. In subjects with LBP, LL and L4-LSL were significantly smaller than in those without. The ΔLSLs at the disc level with DSN showed the greatest decrease: L1-ΔLSL (Δ-3.99°), L2-ΔLSL (Δ-3.31°), L3-ΔLSL (Δ-2.87°), L4-ΔLSL (Δ-3.31°), and L5-ΔLSL (Δ-4.44°) in L1/2, L2/3, L3/4, L4/5, and L5/S1 DSN, respectively. Conversely, distant ΔLSLs were inversely increased: L1-LSL (Δ0.75°) with L4/5 DSN and L2-LSL (Δ0.94°) with L5/S1 DSN.
Conclusion
Sagittal plane alignment was significantly associated with sex, age, LBP, and DSN. LSLs around the levels of DSN were decreased, and there was compensational increase of LSL distant to the DSN to maintain the overall LL.
Figure
Cited by 1 articles
-
The Relationship Between Low Back Pain and Sagittal Spinal Alignment and Back Muscle Mass in Korean Fishery Workers
Minjung Kook, Insuh Kim, Jeongyeon Seo, Hyundong Kim, Heesung Nam, Nami Han
Ann Rehabil Med. 2023;47(6):459-467. doi: 10.5535/arm.23075.
Reference
-
1. Filler AG. Emergence and optimization of upright posture among hominiform hominoids and the evolutionary pathophysiology of back pain. Neurosurg Focus. 2007; 23:E4.
Article2. Legaye J, Duval-Beaupere G. Sagittal plane alignment of the spine and gravity: a radiological and clinical evaluation. Acta Orthop Belg. 2005; 71:213–20.3. de Schepper EI, Damen J, van Meurs JB, Ginai AZ, Popham M, Hofman A, et al. The association between lumbar disc degeneration and low back pain: the influence of age, gender, and individual radiographic features. Spine (Phila Pa 1976). 2010; 35:531–6.4. Luoma K, Riihimaki H, Luukkonen R, Raininko R, Viikari-Juntura E, Lamminen A. Low back pain in relation to lumbar disc degeneration. Spine (Phila Pa 1976). 2000; 25:487–92.
Article5. Tsuji T, Matsuyama Y, Sato K, Hasegawa Y, Yimin Y, Iwata H. Epidemiology of low back pain in the elderly: correlation with lumbar lordosis. J Orthop Sci. 2001; 6:307–11.6. Chun SW, Lim CY, Kim K, Hwang J, Chung SG. The relationships between low back pain and lumbar lordosis: a systematic review and meta-analysis. Spine J. 2017; 17:1180–91.
Article7. Barrey C, Darnis A. Current strategies for the restoration of adequate lordosis during lumbar fusion. World J Orthop. 2015; 6:117–26.
Article8. Endo K, Suzuki H, Tanaka H, Kang Y, Yamamoto K. Sagittal spinal alignment in patients with lumbar disc herniation. Eur Spine J. 2010; 19:435–8.
Article9. Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976). 2005; 30:346–53.
Article10. Abbas J, Hamoud K, May H, Hay O, Medlej B, Masharawi Y, et al. Degenerative lumbar spinal stenosis and lumbar spine configuration. Eur Spine J. 2010; 19:1865–73.
Article11. Murata Y, Takahashi K, Hanaoka E, Utsumi T, Yamagata M, Moriya H. Changes in scoliotic curvature and lordotic angle during the early phase of degenerative lumbar scoliosis. Spine (Phila Pa 1976). 2002; 27:2268–73.
Article12. Quint U, Wilke HJ. Grading of degenerative disk disease and functional impairment : imaging versus patho-anatomical findings. Eur Spine J. 2008; 17:1705–13.13. Jackson RP, McManus AC. Radiographic analysis of sagittal plane alignment and balance in standing volunteers and patients with low back pain matched for age, sex, and size: a prospective controlled clinical study. Spine (Phila Pa 1976). 1994; 19:1611–8.14. Skaf GS, Ayoub CM, Domloj NT, Turbay MJ, El-Zein C, Hourani MH. Effect of age and lordotic angle on the level of lumbar disc herniation. Adv Orthop. 2011; 2011:950576.
Article15. Vialle R, Levassor N, Rillardon L, Templier A, Skalli W, Guigui P. Radiographic analysis of the sagittal alignment and balance of the spine in asymptomatic subjects. J Bone Joint Surg Am. 2005; 87:260–7.
Article16. Murrie VL, Dixon AK, Hollingworth W, Wilson H, Doyle TA. Lumbar lordosis: study of patients with and without low back pain. Clin Anat. 2003; 16:144–7.
Article17. Amonoo-Kuofi HS. Changes in the lumbosacral angle, sacral inclination and the curvature of the lumbar spine during aging. Acta Anat (Basel). 1992; 145:373–7.
Article18. Takeda N, Kobayashi T, Atsuta Y, Matsuno T, Shirado O, Minami A. Changes in the sagittal spinal alignment of the elderly without vertebral fractures: a minimum 10-year longitudinal study. J Orthop Sci. 2009; 14:748–53.
Article19. Fernand R, Fox DE. Evaluation of lumbar lordosis: a prospective and retrospective study. Spine (Phila Pa 1976). 1985; 10:799–803.20. Been E, Kalichman L. Lumbar lordosis. Spine J. 2014; 14:87–97.
Article21. Harrison DE, Harrison DD, Cailliet R, Janik TJ, Holland B. Radiographic analysis of lumbar lordosis: centroid, Cobb, TRALL, and Harrison posterior tangent methods. Spine (Phila Pa 1976). 2001; 26:E235–42.22. Cho IY, Park SY, Park JH, Kim TK, Jung TW, Lee HM. The effect of standing and different sitting positions on lumbar lordosis: radiographic study of 30 healthy volunteers. Asian Spine J. 2015; 9:762–9.
Article23. Lord MJ, Small JM, Dinsay JM, Watkins RG. Lumbar lordosis: effects of sitting and standing. Spine (Phila Pa 1976). 1997; 22:2571–4.24. Dunn G. Design and analysis of reliability studies. Stat Methods Med Res. 1992; 1:123–57.25. Mimura M, Panjabi MM, Oxland TR, Crisco JJ, Yamamoto I, Vasavada A. Disc degeneration affects the multidirectional flexibility of the lumbar spine. Spine (Phila Pa 1976). 1994; 19:1371–80.
Article26. Kim D. Effect of musculoskeletal pain of care workers on job satisfaction. J Phys Ther Sci. 2018; 30:164–8.
Article27. Baron S, Hales T, Hurrell J. Evaluation of symptom surveys for occupational musculoskeletal disorders. Am J Ind Med. 1996; 29:609–17.
Article28. Been E, Barash A, Marom A, Kramer PA. Vertebral bodies or discs: which contributes more to human-like lumbar lordosis? Clin Orthop Relat Res. 2010; 468:1822–9.
Article29. Ghezelbash F, Shirazi-Adl A, Arjmand N, El-Ouaaid Z, Plamondon A, Meakin JR. Effects of sex, age, body height and body weight on spinal loads: sensitivity analyses in a subject-specific trunk musculoskeletal model. J Biomech. 2016; 49:3492–501.
Article30. Hay O, Dar G, Abbas J, Stein D, May H, Masharawi Y, et al. The lumbar lordosis in males and females, revisited. PLoS One. 2015; 10:e0133685.
Article31. Whitcome KK, Shapiro LJ, Lieberman DE. Fetal load and the evolution of lumbar lordosis in bipedal hominins. Nature. 2007; 450:1075–8.
Article32. Masharawi Y, Dar G, Peleg S, Steinberg N, Medlej B, May H, et al. A morphological adaptation of the thoracic and lumbar vertebrae to lumbar hyperlordosis in young and adult females. Eur Spine J. 2010; 19:768–73.
Article33. Dammers R, Koehler PJ. Lumbar disc herniation: level increases with age. Surg Neurol. 2002; 58:209–13.
Article34. Schwab F, Lafage V, Boyce R, Skalli W, Farcy JP. Gravity line analysis in adult volunteers: age-related correlation with spinal parameters, pelvic parameters, and foot position. Spine (Phila Pa 1976). 2006; 31:E959–67.35. Lamartina C, Berjano P. Classification of sagittal imbalance based on spinal alignment and compensatory mechanisms. Eur Spine J. 2014; 23:1177–89.
Article36. Adams MA, Mannion AF, Dolan P. Personal risk factors for first-time low back pain. Spine (Phila Pa 1976). 1999; 24:2497–505.
Article37. Pavlov PW, Meijers H, van Limbeek J, Jacobs WC, Lemmens JA, Obradov-Rajic M, et al. Good outcome and restoration of lordosis after anterior lumbar interbody fusion with additional posterior fixation. Spine (Phila Pa 1976). 2004; 29:1893–1900.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Change in Sagittal Plane of the Lumbar Spine in Patients with Anterior Lumbar Interbody Fusion and Pedicle Instrumentation and its Influencing Factors
- Associations Between Trunk Muscle/Fat Composition, Narrowing Lumbar Disc Space, and Low Back Pain in Middle-Aged Farmers: A Cross-Sectional Study
- Radiological Assessment of Morphological Changes of Lumbar Spine: From First to 9th Decade of Life
- Comparative study of the intervertebral spaces in the normal and the disc patients
- Analysis of the Sagittal Alignment of Normal Spines