Acute Crit Care.
2021 Aug;36(3):201-207. 10.4266/acc.2021.00402.
The Mount Sinai Hospital Institute for critical care medicine response to the COVID-19 pandemic
- Affiliations
-
- 1Institute for Critical Care Medicine, Icahn School of Medicine at Mount Sinai, New York, NY, USA
- 2Institute for Critical Care Medicine, Icahn School of Medicine at Mount Sinai, New York, NY, USA
- 3Department of Emergency Medicine, Icahn School of Medicine at Mount Sinai, New York, NY, USA
- 4Department of Anesthesiology, Perioperative, and Pain Medicine, Icahn School of Medicine at Mount Sinai, New York, NY, USA
- 5Division of Pulmonary Medicine, Icahn School of Medicine at Mount Sinai, New York, NY, USA
- 6Department of Neurosurgery, Icahn School of Medicine at Mount Sinai, New York, NY, USA
- 7Division of Cardiology, Icahn School of Medicine at Mount Sinai, New York, NY, USA
- KMID: 2519446
- DOI: http://doi.org/10.4266/acc.2021.00402
Abstract
- Background
The coronavirus disease 2019 (COVID-19) pandemic resulted in a surge of critically ill patients. This was especially true in New York City. We present a roadmap for hospitals and healthcare systems to prepare for a Pandemic.
Methods
This was a retrospective review of how Mount Sinai Hospital (MSH) was able to rapidly prepare to handle the pandemic. MSH, the largest academic hospital within the Mount Sinai Health System, rapidly expanded the intensive care unit (ICU) bed capacity, including creating new ICU beds, expanded the workforce, and created guidelines.
Results
MSH a 1,139-bed quaternary care academic referral hospital with 104 ICU beds expanded to 1,453 beds (27.5% increase) with 235 ICU beds (126% increase) during the pandemic peak in the first week of April 2020. From March to June 2020, with follow-up through October 2020, MSH admitted 2,591 COVID-19-positive patients, 614 to ICUs. Most admitted patients received noninvasive support including a non-rebreather mask, high flow nasal cannula, and noninvasive positive pressure ventilation. Among ICU patients, 68.4% (n=420) received mechanical ventilation; among the admitted ICU patients, 42.8% (n=263) died, and 47.8% (n=294) were discharged alive.
Conclusions
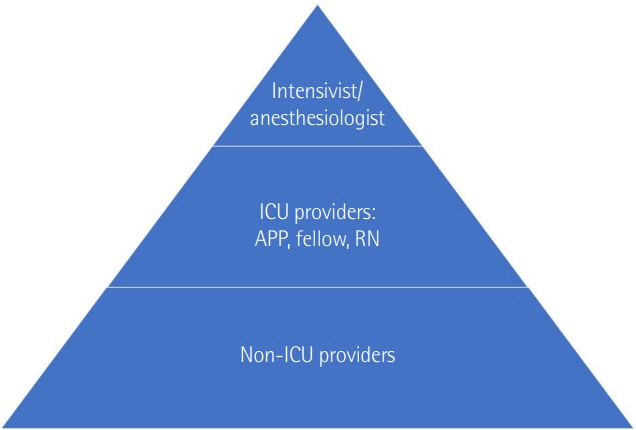
Flexible bed management initiatives; teamwork across multiple disciplines; and development and implementation of guidelines were critical accommodating the surge of critically ill patients. Non-ICU services and staff were deployed to augment the critical care work force and open new critical care units. This approach to rapidly expand bed availability and staffing across the system helped provide the best care for the patients and saved lives.
Keyword
Figure
Cited by 1 articles
-
Rapid communication for effective medical resource allocation in the COVID-19 pandemic
Kwangha Lee
Acute Crit Care. 2021;36(3):262-263. doi: 10.4266/acc.2021.01046.
Reference
-
1. Johns Hopkins University. Covid-19 dashboard by the center for systems [Internet]. Baltimore (MD): Johns Hopkins University;2020 [cited 2020 Apr 17]. Available from: https://www.covidtracker.com/.2. Halpern NA, Pastores SM. Critical care medicine beds, use, occupancy, and costs in the United States: a methodological review. Crit Care Med. 2015; 43:2452–9.3. Halpern NA, Tan KS, DeWitt M, Pastores SM. Intensivists in U.S. acute care hospitals. Crit Care Med. 2019; 47:517–25.
Article4. Halpern NA, Tan KS. United States resource availability for COVID-19 [Internet]. Mount Prospect (IL): Society of Critical Care Medicine;2020 [cited 2020 Apr 17]. Available from: https://sccm.org/getattachment/Blog/March-2020/United-States-Resource-Availability-for-COVID-19/United-States-Resource-Availability-for-COVID-19.pdf?lang=en-US.5. Kumaraiah D, Yip N, Ivascu N, Hill L. Innovative ICU physician care models: Covid-19 pandemic at NewYork-Presbyterian. NEJM Catal Innov Care Deliv. 2020; 1.6. Farmer JC, Wax RS MD, Baldisseri MR. Preparing your ICU for disaster response [Internet]. Mount Prospect (IL): Society of Critical Care Medicine;2020 [cited 2020 Apr 17]. Available from: https://www.sccm.org/getattachment/Disaster/PreparingforDisasterResponse.pdf?lang=en-US.7. Halpern NA, Kaplan LJ, Rausen M, Yang JJ. Configuring ICUs in the COVID-19 Era. Mount Prospect (IL): Society of Critical Care Medicine;2020.8. Scholten EL, Beitler JR, Prisk GK, Malhotra A. Treatment of ARDS with prone positioning. Chest. 2017; 151:215–24.
Article9. Cherian SV, Kumar A, Akasapu K, Ashton RW, Aparnath M, Malhotra A. Salvage therapies for refractory hypoxemia in ARDS. Respir Med. 2018; 141:150–8.
Article10. Kumar P, Kattan O, Broome B, Singhal S. Reassessing Covid-19 needs: how providers can reexamine their surge capacity, supply availability, workforce readiness, and financial resiliency. NEJM Catal Innov Care Deliv. 2020; 1.11. Kim MK, Rabinowitz LG, Nagula S, Dunn A, Chalil J, Tao Xu, et al. A primer for clinician deployment to the medicine floors from an epicenter of Covid-19. NEJM Catal Innov Care Deliv. 2020; 1.12. Alhazzani W, Møller MH, Arabi YM, Loeb M, Gong MN, Fan E, et al. Surviving Sepsis Campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Intensive Care Med. 2020; 46:854–87.
Article13. Evan S, Leibner M, Elvera L, Baron M, Ronak S, Shah M, et al. Critical care simulation education program during the COVID-19 pandemic. J Patient Saf Forthcoming. 2021.14. Christian MD, Wax R, Lazar N. Critical care during a pandemic: final report of the Ontario health plan for an influenza pandemic (OHPIP) working group on adult critical care admission, discharge and triage criteria. Toronto, Ontario, Canada: Toronto, Ontario Health System;2006.15. Mount Sinai. Faculty and staff education during COVID-19 [Internet]. New York (NY): Mount Sinai;2020 [cited 2020 May 27]. https://www.mountsinai.org/about/covid19/staff-resources/critical-care-education.16. Caputo KM, Byrick R, Chapman MG, Orser BJ, Orser BA. Intubation of SARS patients: infection and perspectives of healthcare workers. Can J Anaesth. 2006; 53:122–9.
Article17. Peng PW, Ho PL, Hota SS. Outbreak of a new coronavirus: what anaesthetists should know. Br J Anaesth. 2020; 124:497–501.
Article18. Zucco , Liana , Levy N, Ketchandji D, Aziz M, Ramachandran SK. An Update on the Perioperative Considerations for COVID-19 Severe Acute Respiratory Syndrome Coronavirus-2 (SARS-CoV-2) [Internet]. Rochester (MN): Anesthesia Patient Safety Foundation;2020 [cited 2021 Aug 24]. Available from: https://www.apsf.org/article/an-update-on-the-perioperative-considerations-for-covid-19-severe-acute-respiratory-syndrome-coronavirus-2-sars-cov-2/.
Article19. Ranney ML, Griffeth V, Jha AK. Critical supply shortages: the need for ventilators and personal protective equipment during the COVID-19 pandemic. N Engl J Med. 2020; 382:e41.20. Respiratory care committee of Chinese Thoracic Society. Expert consensus on preventing nosocomial transmission during respiratory care for critically ill patients infected by 2019 novel coronavirus pneumonia. Zhonghua Jie He Hu Xi Za Zhi. 2020; 17:E020.21. Hui DS, Chow BK, Lo T, Tsang OT, Ko FW, Ng SS, et al. Exhaled air dispersion during high-flow nasal cannula therapy versus CPAP via different masks. Eur Respir J. 2019; 53:1802339.
Article22. Apfelbaum JL, Hagberg CA, Caplan RA, Blitt CD, Connis RT, Nickinovich DG, et al. Practice guidelines for management of the difficult airway: an updated report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway. Anesthesiology. 2013; 118:251–70.23. Association of Anaesthetists. Anaesthetic management of patients during a COVID-19 outbreak [Internet]. London: Association of Anaesthetists;2020 [cited 2020 May 27]. Available from: https://anaesthetists.org/Home/Resources-publications/Anaesthetic-Management-of-Patients-During-a-COVID-19-Outbreak.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Rapid deployment of an emergency department-intensive care unit for the COVID-19 pandemic
- New York City Vascular Surgeons during the COVID-19 Pandemic
- The fourth wave: vaccination status and intensive care unit mortality at a large hospital system in New York City
- Patient Perception of Telehealth Services for Breast and Gynecologic Oncology Care during the COVID-19 Pandemic: A Single Center Surveybased Study
- Age-Related Morbidity and Mortality among Patients with COVID-19