Ann Hepatobiliary Pancreat Surg.
2021 Aug;25(3):414-418. 10.14701/ahbps.2021.25.3.414.
Dextroplantation of a reduced left lateral section graft in an infant undergoing living donor liver transplantation
- Affiliations
-
- 1Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Pediatrics, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2519301
- DOI: http://doi.org/10.14701/ahbps.2021.25.3.414
Abstract
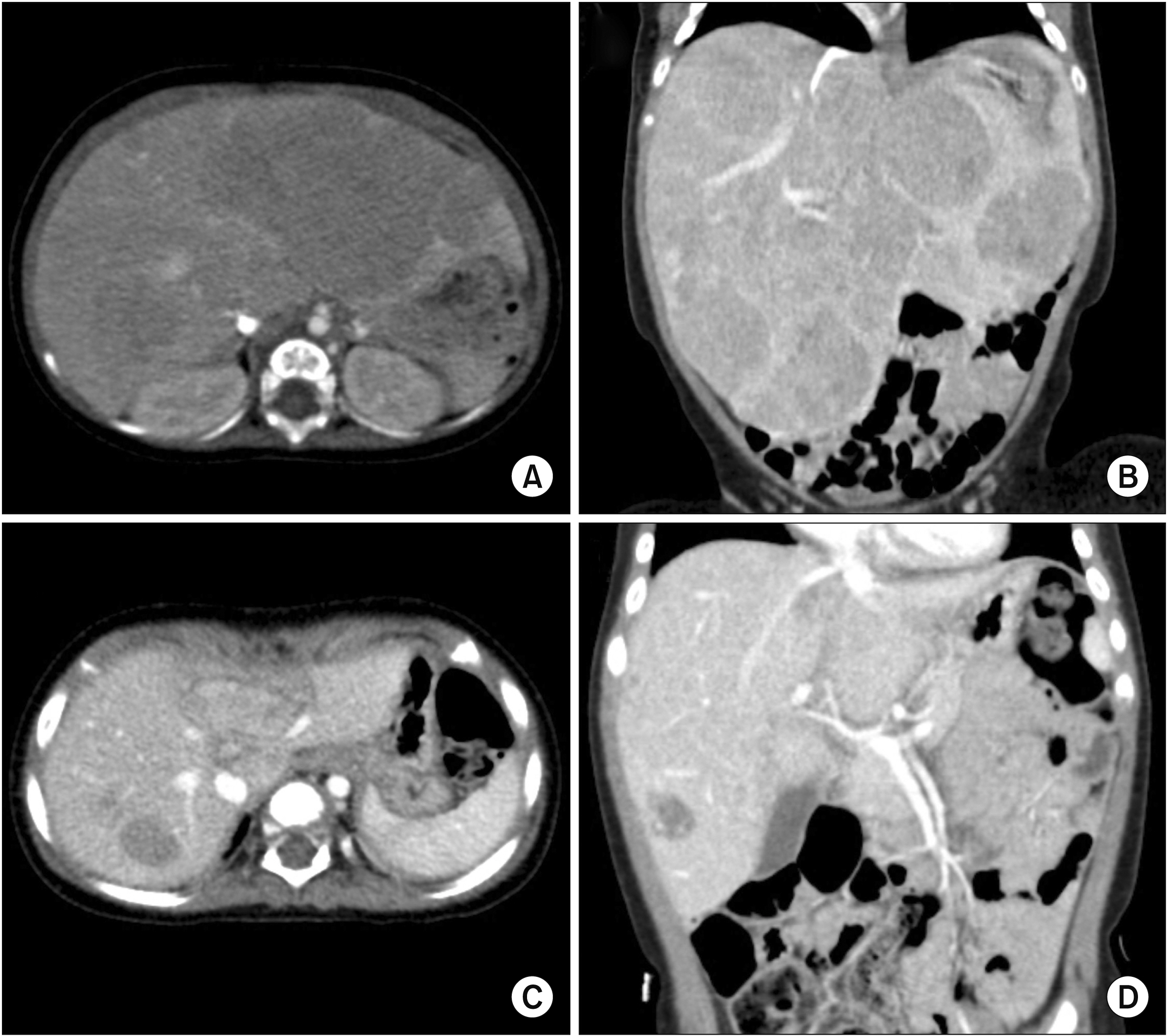
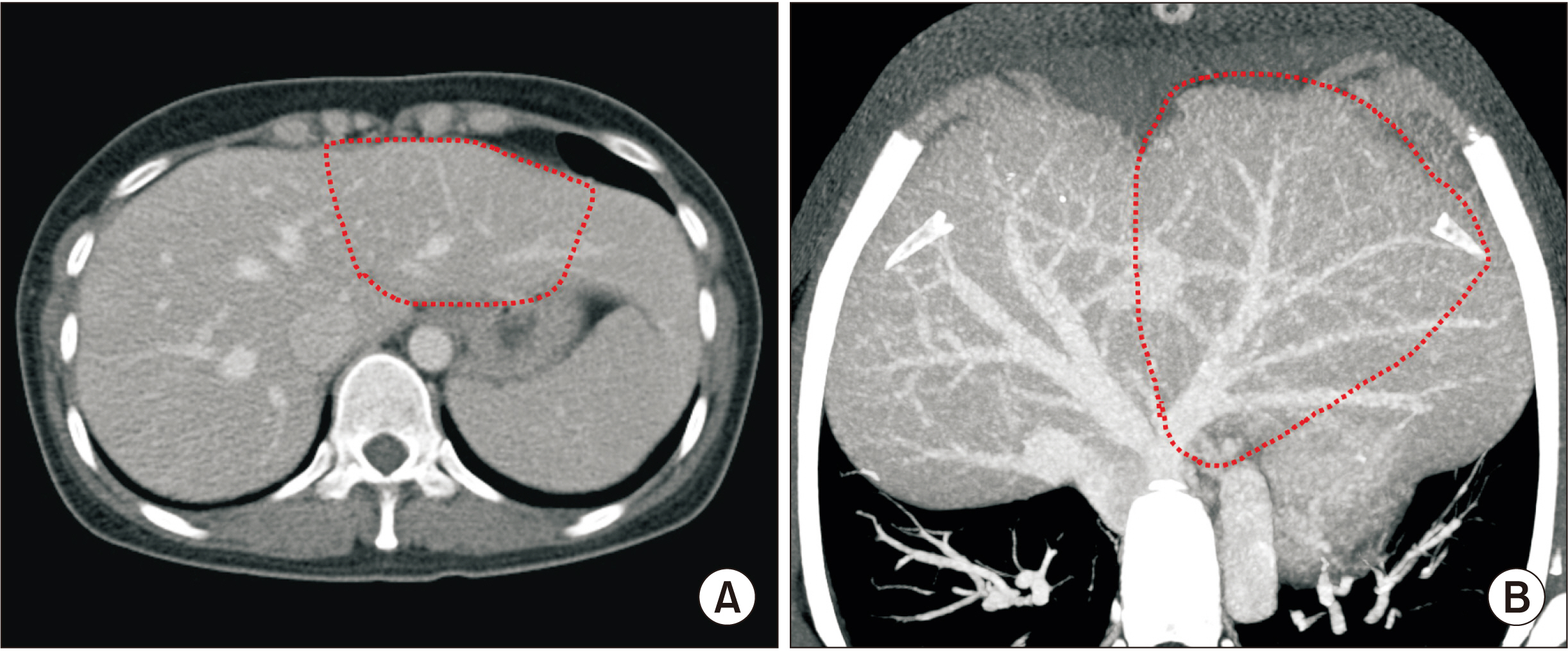
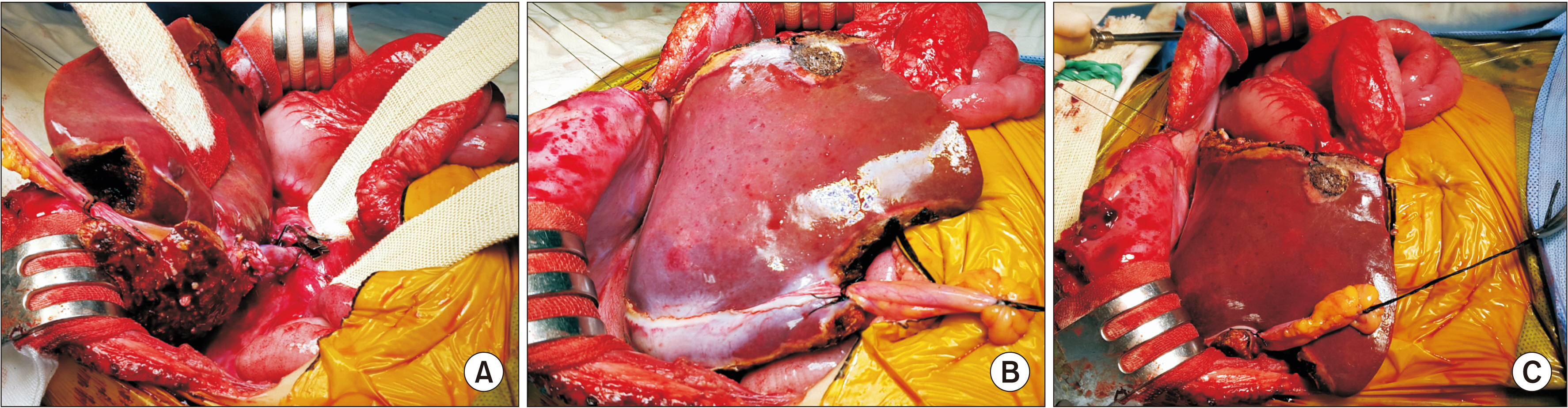
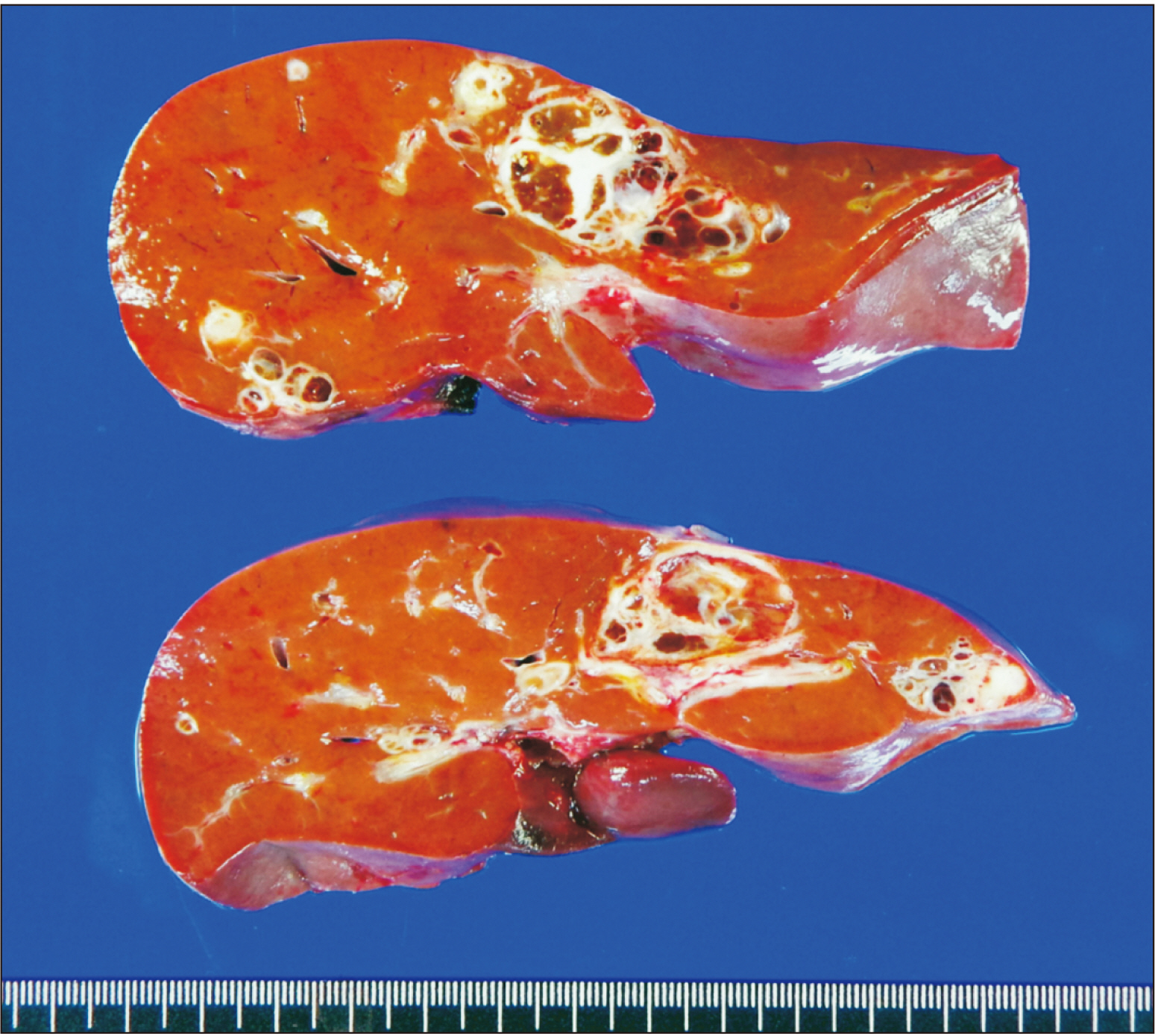
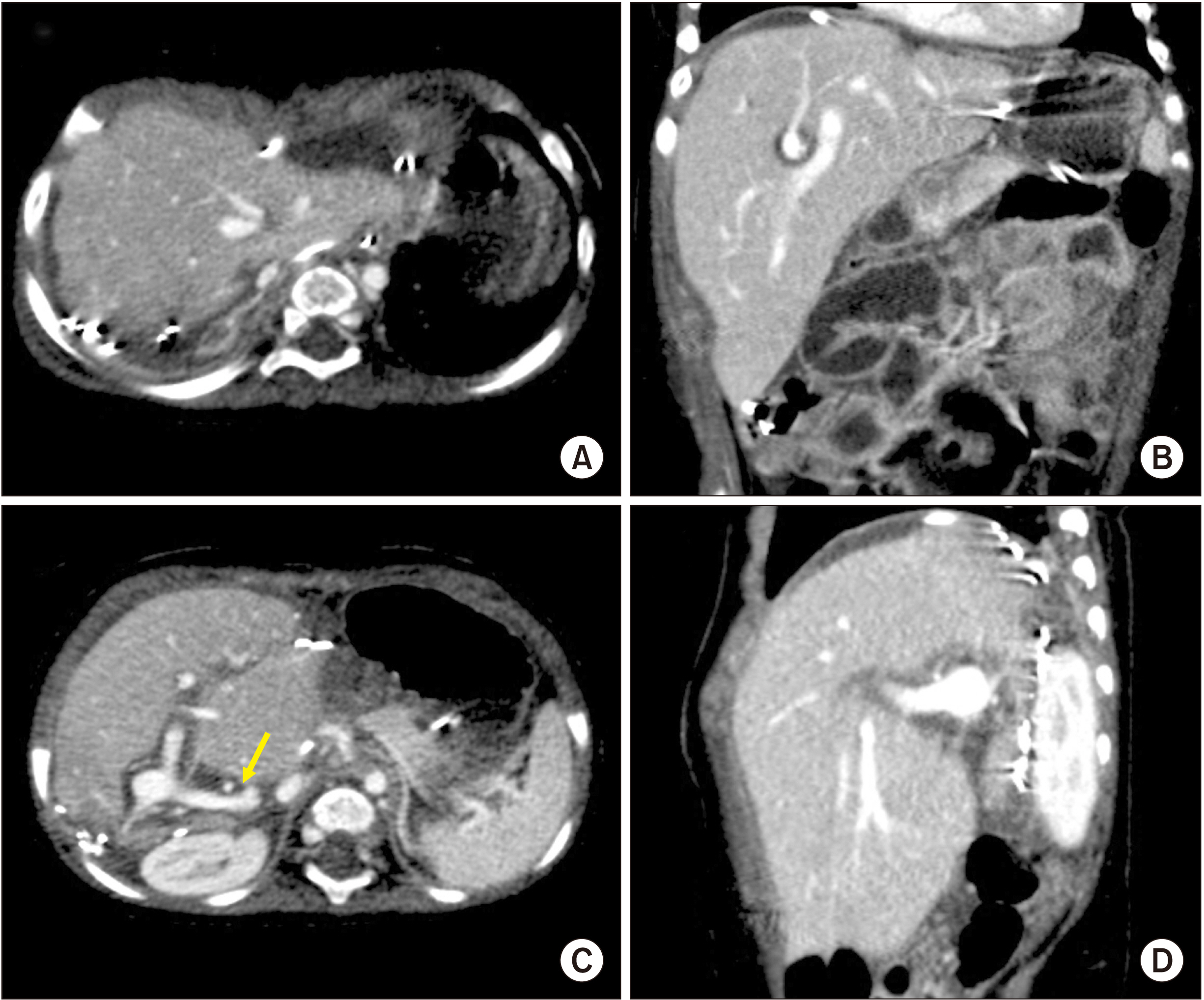
- Graft size matching is essential for successful liver transplantation in infant recipients. We present our technique of graft dextroplantation used in an infant who underwent living donor liver transplantation (LDLT) using a reduced left lateral section (LLS) graft. The patient was an 11-month-old female infant weighing 7.8 kg with hepatoblastoma. She was partially responsive to systemic chemotherapy. Thus, LDLT was performed to treat the tumor. The living donor was a 34-year-old mother of the patient. After non-anatomical size reduction, the weight of the reduced LLS graft was 235 g, with a graft-to-recipient weight ratio of 3.0%. Recipient hepatectomy was performed according to the standard procedures of pediatric LDLT. At the beginning of graft implantation, the graft was temporarily placed at the abdomen to determine the implantation location. The graft portal vein was anastomosed with an interposed external iliac vein homograft. As the liver graft was not too large and it was partially accommodated in the right subphrenic fossa, thus the abdominal wall wound was primarily closed. The patient recovered uneventfully. An imaging study revealed deep accommodation of the graft within the right subphrenic fossa. The patient has been doing well for six months without any vascular complications. This case suggests that dextroplantation of a reduced LLS graft can be a useful technical option for LDLT in infant patients.
Keyword
Figure
Cited by 1 articles
-
Living donor liver transplantation with graft dextro-rotation and vein interposition in a pediatric patient with congenital absence of the portal vein
Jung-Man Namgoong, Shin Hwang, Gil-Chun Park, Sang-Hoon Kim, Kyung Mo Kim, Seak Hee Oh
Ann Liver Transplant. 2023;3(1):35-43. doi: 10.52604/alt.23.0004.
Reference
-
1. Kasahara M, Sakamoto S, Sasaki K, Uchida H, Kitajima T, Shigeta T, et al. 2017; Living donor liver transplantation during the first 3 months of life. Liver Transpl. 23:1051–1057. DOI: 10.1002/lt.24743. PMID: 28220684.
Article2. Kanazawa H, Sakamoto S, Fukuda A, Uchida H, Hamano I, Shigeta T, et al. 2013; Living-donor liver transplantation with hyperreduced left lateral segment grafts: a single-center experience. Transplantation. 95:750–754. DOI: 10.1097/TP.0b013e31827a93b4. PMID: 23503505.3. Kasahara M, Sakamoto S, Shigeta T, Uchida H, Hamano I, Kanazawa H, et al. 2013; Reducing the thickness of left lateral segment grafts in neonatal living donor liver transplantation. Liver Transpl. 19:226–228. DOI: 10.1002/lt.23572. PMID: 23172804.
Article4. Kasahara M, Sakamoto S, Umeshita K, Uemoto S. 2014; Effect of graft size matching on pediatric living-donor liver transplantation in Japan. Exp Clin Transplant. 12 Suppl 1:1–4. DOI: 10.6002/ect.25Liver.L5. PMID: 24635782.
Article5. Mizuta K, Yasuda Y, Egami S, Sanada Y, Wakiya T, Urahashi T, et al. 2010; Living donor liver transplantation for neonates using segment 2 monosubsegment graft. Am J Transplant. 10:2547–2552. DOI: 10.1111/j.1600-6143.2010.03274.x. PMID: 20977646.
Article6. Namgoong JM, Hwang S, Song GW, Kim DY, Ha TY, Jung DH, et al. 2020; Pediatric liver transplantation with hyperreduced left lateral segment graft. Ann Hepatobiliary Pancreat Surg. 24:503–512. DOI: 10.14701/ahbps.2020.24.4.503. PMID: 33234754. PMCID: PMC7691208.
Article7. Namgoong JM, Hwang S, Kim DY, Song GW, Ahn CS, Kim KM, et al. 2020; Pediatric split liver transplantation using a hyperreduced left lateral segment graft in an infant weighing 4 kg. Korean J Transplant. 34:204–209. DOI: 10.4285/kjt.2020.34.3.204.
Article8. Moon SB, Moon JI, Kwon CH, Kim SJ, Seo JM, Joh JW, et al. 2011; Graft rotation and late portal vein complications in pediatric living donor liver transplantation using left-sided grafts: long-term computed tomography observations. Liver Transpl. 17:717–722. DOI: 10.1002/lt.22262. PMID: 21618693.
Article9. Ahn SW, Yi NJ, Kim HC, Ahn HY, Hong SK, Lee JM, et al. 2021; Dextroplantation of left liver graft in infants. Liver Transpl. 27:222–230. DOI: 10.1002/lt.25883. PMID: 32897624.
Article10. Raices M, Czerwonko ME, Ardiles V, Boldrini G, D'Agostino D, Marcó Del Pont J, et al. 2019; Short- and long-term outcomes after live-donor transplantation with hyper-reduced liver grafts in low-weight pediatric recipients. J Gastrointest Surg. 23:2411–2420. DOI: 10.1007/s11605-019-04188-y. PMID: 30887299.
Article11. Sakamoto S, Kanazawa H, Shigeta T, Uchida H, Sasaki K, Hamano I, et al. 2014; Technical considerations of living donor hepatectomy of segment 2 grafts for infants. Surgery. 156:1232–1237. DOI: 10.1016/j.surg.2014.05.003. PMID: 24909347.
Article12. Namgoong JM, Hwang S, Park GC, Ahn CS, Kim KH, Kim KM, et al. 2021; Outflow vein venoplasty of left lateral section graft for living donor liver transplantation in infant recipients. Pediatr Transplant. 25:e13970. DOI: 10.1111/petr.13970. PMID: 33433048.
Article13. Hwang S, Kim DY, Ahn CS, Moon DB, Kim KM, Park GC, et al. 2013; Computational simulation-based vessel interposition reconstruction technique for portal vein hypoplasia in pediatric liver transplantation. Transplant Proc. 45:255–258. DOI: 10.1016/j.transproceed.2012.05.090. PMID: 23375311.
Article14. Hasegawa T, Kimura T, Sasaki T, Okada A. 2002; Living-related liver transplantation for biliary atresia associated with polysplenia syndrome. Pediatr Transplant. 6:78–81. DOI: 10.1034/j.1399-3046.2002.1c045.x. PMID: 11906647.
Article15. Kwon H, Kwon H, Hong JP, Han Y, Park H, Song GW, et al. 2015; Use of cryopreserved cadaveric arterial allograft as a vascular conduit for peripheral arterial graft infection. Ann Surg Treat Res. 89:51–54. DOI: 10.4174/astr.2015.89.1.51. PMID: 26131446. PMCID: PMC4481033.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dextroplantation of a reduced left lateral section graft in an infant undergoing living donor liver transplantation
- Pediatric liver transplantation using hyper-reduced left lateral section and monosegment graft for infant patients: A collective review of Korean experience
- Left at right heterotopic implantation of left liver graft in adult-to-adult living donor liver transplantation: the technical concern for decision-making
- Split liver transplantation for one adult and one pediatric recipient: A collective review of Korean experience
- Tailored techniques of graft outflow vein reconstruction in pediatric liver transplantation at Asan Medical Center