Healthc Inform Res.
2021 Jul;27(3):231-240. 10.4258/hir.2021.27.3.231.
Simple Wearable Device to Reduce Stress When Delivering a Speech without Pre-training
- Affiliations
-
- 1Graduate School of Interdisciplinary Science and Engineering in Health Systems, Okayama University, Okayama, Japan
- 2Faculty of Health Sciences, Okayama University Medical School, Okayama, Japan
- KMID: 2519039
- DOI: http://doi.org/10.4258/hir.2021.27.3.231
Abstract
Objectives
There are many occasions in modern life when people must deliver presentations in front of audiences. Most people feel nervous before and while giving a speech. If there were a simple way to ease their stress, speakers would be able to perform better and their quality of life would improve. Consequently, this study aimed to alleviate the stress of speakers giving speeches by regulating breathing using a simple device.
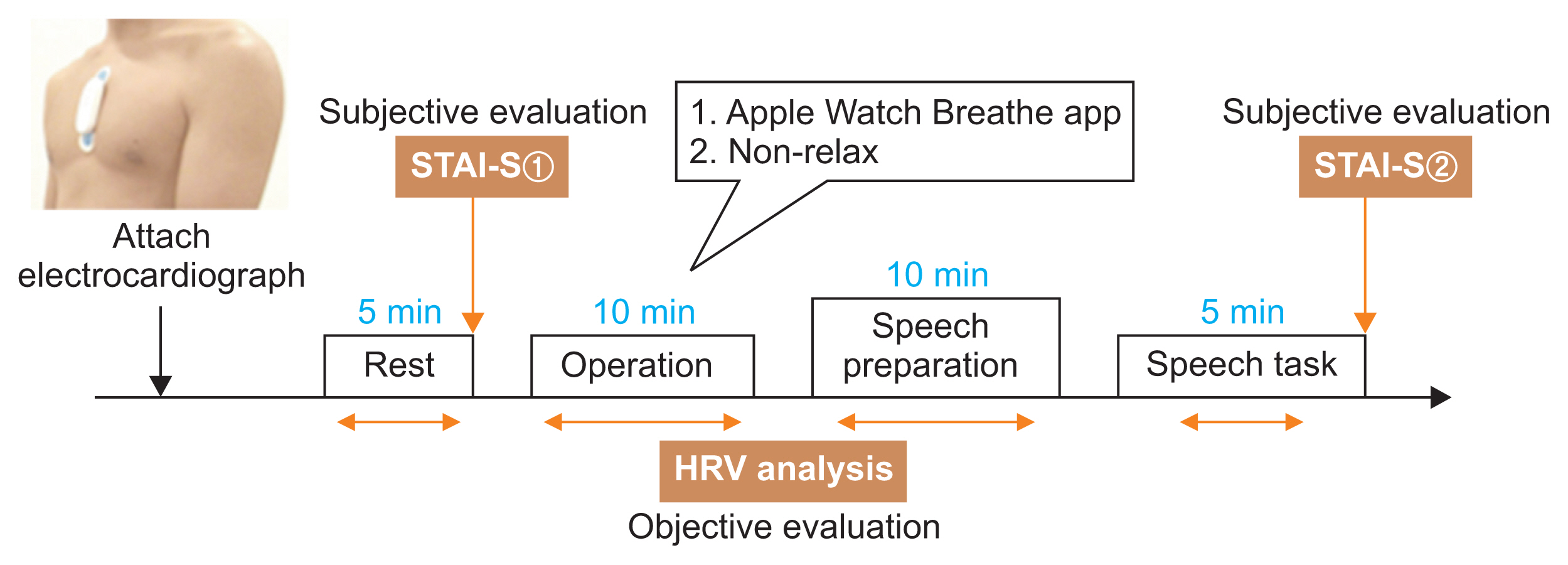
Methods
To achieve this goal, a popular device, the Apple Watch, was chosen. Twenty-eight participants were divided into two groups: the Breathe app group and the non-Breathe app group. The Breathe app group regulated their breathing using the Breathe app installed on an Apple Watch before speech preparation. The non-Breathe app group listened to an explanation of the experiment so that they could not undertake their own stress-easing strategies. Participants prepared speeches about themselves and delivered them in front of the researcher.
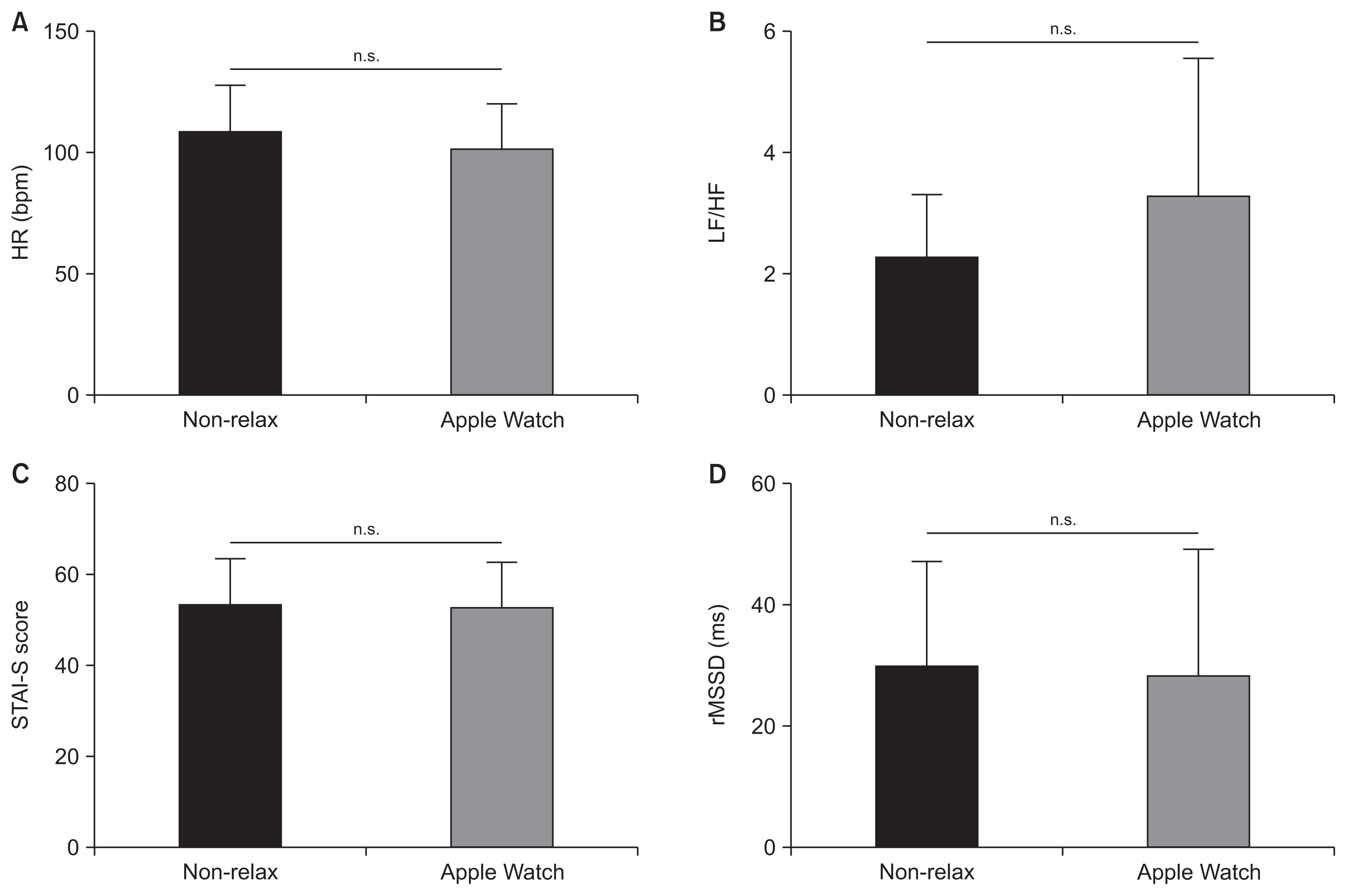
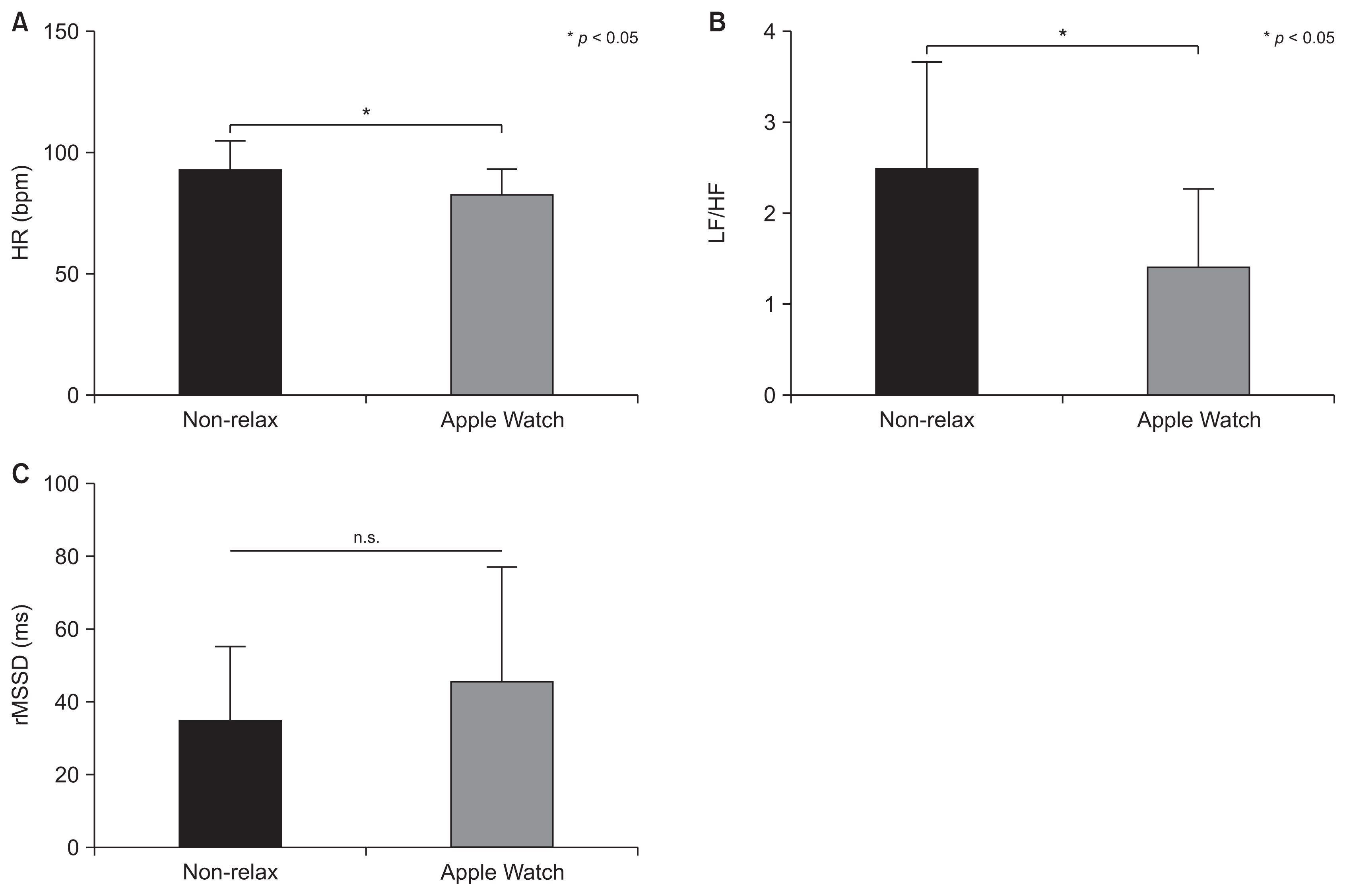
Results
The Breathe app exercise eased stress during the exercise itself and the preparation phase of the speech task based on participants’ cardiac activity. However, stress was not alleviated during speech delivery.
Conclusions
Based on the experimental setting and results of this study, together with the findings of previous studies, introducing pre-training sessions and performing stress-easing tasks before and/or during a speech, such as sending vibrations to participants’ wearable devices, might be an effective way to reduce stress when delivering speeches immediately after the breath-regulating task.
Figure
Reference
-
References
1. Yerkes RM, Dodson JD. The relation of strength of stimulus to rapidity of habit-formation. J Comp Neurol Psychol. 1908; 18(5):459–82.
Article2. Owens M, Stevenson J, Hadwin JA, Norgate R. Anxiety and depression in academic performance: an exploration of the mediating factors of worry and working memory. Sch Psychol Int. 2012; 33(4):433–49.
Article3. Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory. Palo Alto (CA): Consulting Psychologists Press;1983.4. Lehrer PM, Woolfolk RL, Sime WE. Principles and practice of stress management. 3rd ed. New York (NY): Guilford Press;2007.5. Krisanaprakornkit T, Krisanaprakornkit W, Piyavhatkul N, Laopaiboon M. Meditation therapy for anxiety disorders. Cochrane Database Syst Rev. 2006; (1):CD004998.
Article6. Wells R, Outhred T, Heathers JA, Quintana DS, Kemp AH. Matter over mind: a randomised-controlled trial of single-session biofeedback training on performance anxiety and heart rate variability in musicians. PLoS One. 2012; 7(10):e46597.
Article7. Burns JL, Labbe E, Arke B, Capeless K, Cooksey B, Steadman A, et al. The effects of different types of music on perceived and physiological measures of stress. J Music Ther. 2002; 39(2):101–16.
Article8. Labbe E, Schmidt N, Babin J, Pharr M. Coping with stress: the effectiveness of different types of music. Appl Psychophysiol Biofeedback. 2007; 32(3–4):163–8.
Article9. Savov V, Wu D. Apple maintains lead after smartwatches defy global sales slump [Internet]. New York (NY): Bloomberg.com;2020. [cited at 2021 Jun 29]. Available from https://www.bloomberg.com/news/articles/2020-05-07/apple-maintains-lead-after-smartwatches-defy-global-sales-slump .10. Stanford University School of Medicine. Apple Heart Study demonstrates ability of wearable technology to detect atrial fibrillation [Internet]. Stanford (CA): Stanford University;2019. [cited at 2021 Apr]. Available from http://med.stanford.edu/news/all-news/2019/03/apple-heart-study-demonstrates-ability-of-wearable-technology.html .11. Kirk SE. Comparison of the Apple Watch, Fitbit Surge, and Actigraph GT9X link in measuring energy expenditure, steps, distance, and heart rate [thesis]. Cleveland (OH): Cleveland State University;2016.12. El-Amrawy F, Nounou MI. Are currently available wearable devices for activity tracking and heart rate monitoring accurate, precise, and medically beneficial? Healthc Inform Res. 2015; 21(4):315–20.
Article13. Shcherbina A, Mattsson CM, Waggott D, Salisbury H, Christle JW, Hastie T, et al. Accuracy in wrist-worn, sensor-based measurements of heart rate and energy expenditure in a diverse cohort. J Pers Med. 2017; 7(2):3.
Article14. Wallen MP, Gomersall SR, Keating SE, Wisloff U, Coombes JS. Accuracy of heart rate watches: implications for weight management. PLoS One. 2016; 11(5):e0154420.
Article15. Costa J, Guimbretiere F, Jung MF, Choudhury T. Boostmeup: Improving cognitive performance in the moment by unobtrusively regulating emotions with a smartwatch. Proc ACM Interact Mob Wearable Ubiquitous Technol. 2019; 3(2):1–23.16. Azevedo RT, Bennett N, Bilicki A, Hooper J, Markopoulou F, Tsakiris M. The calming effect of a new wearable device during the anticipation of public speech. Sci Rep. 2017; 7(1):2285.
Article17. Costa J, Adams AT, Jung MF, Guimbretiere F, Choudhury T. EmotionCheck: leveraging bodily signals and false feedback to regulate our emotions. In : Proceedings of the 2016 ACM International Joint Conference on Pervasive and Ubiquitous Computing (UbiComp); 2016 Sep 12–16; Heidelberg, Germany. p. 758–69.18. Vaschillo EG, Vaschillo B, Lehrer PM. Characteristics of resonance in heart rate variability stimulated by biofeedback. Appl Psychophysiol Biofeedback. 2006; 31(2):129–42.
Article19. Kirschbaum C, Pirke KM, Hellhammer DH. The 'Trier Social Stress Test': a tool for investigating psychobiological stress responses in a laboratory setting. Neuropsychobiology. 1993; 28(1–2):76–81.20. Malik M, Thomas Bigger J, John Camm A, Kleiger RE, Malliani A, Moss AJ, Schwartz PJ. Heart rate variability: standards of measurement, physiological interpretation, and clinical use. Eur Heart J. 1996; 17(3):354–81.
Article21. Hidano T, Fukuhara M, Iwawaki S, Soga S, Spielberger CD. State-Trait Anxiety Inventory–Form JYZ. Tokyo, Japan: Jitsumu Kyoiku Shuppan Co. Ltd;2000.22. Hayano J, Mukai S, Sakakibara M, Okada A, Takata K, Fujinami T. Effects of respiratory interval on vagal modulation of heart rate. Am J Physiol. 1994; 267(1 Pt 2):H33–40.
Article23. Saboul D, Pialoux V, Hautier C. The impact of breathing on HRV measurements: implications for the longitudinal follow-up of athletes. Eur J Sport Sci. 2013; 13(5):534–42.
Article24. Dickerson SS, Kemeny ME. Acute stressors and cortisol responses: a theoretical integration and synthesis of laboratory research. Psychol Bull. 2004; 130(3):355–91.
Article25. Blum J, Rockstroh C, Goritz AS. Heart rate variability biofeedback based on slow-paced breathing with immersive virtual reality nature scenery. Front Psychol. 2019; 10:2172.
Article26. Prinsloo GE, Rauch HL, Lambert MI, Muench F, Noakes TD, Derman WE. The effect of short duration heart rate variability (HRV) biofeedback on cognitive performance during laboratory induced cognitive stress. Appl Cogn Psychol. 2011; 25(5):792–801.
Article27. Yu B, Feijs L, Funk M, Hu J. Breathe with touch: a tactile interface for breathing assistance system. Abascal J, Barbosa S, Fetter M, Gross T, Palanque P, Winckler M, editors. Human-Computer Interaction – INTERACT. 2015. Cham, Switzerland: Springer;2015. p. 45–52.
Article28. Gatchel RJ, Proctor JD. Effectiveness of voluntary heart rate control in reducing speech anxiety. J Consult Clin Psychol. 1976; 44(3):381–9.
Article29. Bhandari R, Parnandi A, Shipp E, Ahmed B, Gutierrez-Osuna R. Music-based respiratory biofeedback in visually-demanding tasks. In : Proceedings of the 15th International Conference on New Interfaces for Musical Expression (NIME); 2015 May 31–Jun 3; Baton Rouge, LA. p. 78–82.30. Zhou Y, Murata A, Watanabe J. The calming effect of heartbeat vibration. In : Proceedings of 2020 IEEE Haptics Symposium (HAPTICS); 2020 Mar 28–31; Crystal city, VA. p. 677–83.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Can Fitness Trackers Track Sleep?
- Modest Effects of NeurofeedbackAssisted Meditation Using a Wearable Device on Stress Reduction: A Randomized, Double-Blind, and Controlled Study
- Study on the Voiding Detection System Using Wearable Device
- Quantified Self-Using Consumer Wearable Device: Predicting Physical and Mental Health
- Training Programs for Improving Speech Perception in Noise: A Review