Ann Surg Treat Res.
2021 Aug;101(2):111-119. 10.4174/astr.2021.101.2.111.
Diverting ileostomy itself may not increase the rate of postoperative readmission related to dehydration after low anterior resection
- Affiliations
-
- 1Center for Colorectal Cancer, Research Institute and Hospital, National Cancer Center, Goyang, Korea
- 2Biostatistics Collaboration Team, Research Institute and Hospital, National Cancer Center, Goyang, Korea
- KMID: 2519004
- DOI: http://doi.org/10.4174/astr.2021.101.2.111
Abstract
- Purpose
This study was performed to evaluate the risk of readmission in the first year after low anterior resection (LAR) for patients with rectal cancer and to identify the contributing factors for readmission related to dehydration specifically.
Methods
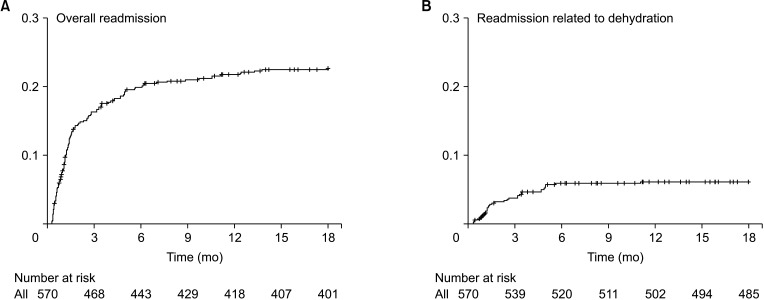
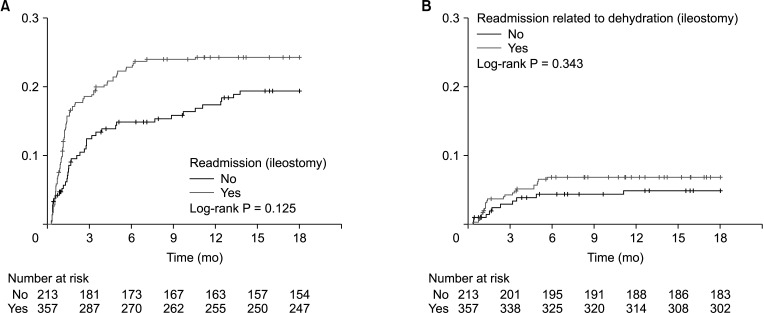
This was a retrospective analysis of 570 patients who underwent LAR for rectal cancer at National Cancer Center, Republic of Korea. A diverting loop ileostomy was performed in 357 (62.6%) of these patients. Readmission was defined as an unplanned visit to the emergency room or admission to the ward. The reasons for readmission were reviewed and compared between the ileostomy (n = 357) and no-ileostomy (n = 213) groups. The risk factors for readmission and readmission due to dehydration were analyzed using multivariable logistic and Cox proportional hazard model.
Results
Dehydration was the most common cause of readmission in both groups (ileostomy group, 6.7%, and no-ileostomy group, 4.7%, P = 0.323). On multivariable analysis, risk factors for readmission were an estimated intraoperative blood loss of ≥400 mL (odds ratio [OR], 1.757; 95% confidence interval [CI], 1.058–2.918; P = 0.029), and postoperative chemotherapy (OR, 2.914; 95% CI, 1.824–4.653; P < 0.001). On multivariable analysis, postoperative chemotherapy, and not a diverting loop ileostomy, was an independent risk factor for dehydration-related readmission (OR, 5.102; 95% CI, 1.772–14.688; P = 0.003).
Conclusion
The most common cause of readmission after LAR for rectal cancer was dehydration, as reported previously. Postoperative chemotherapy, not the creation of a diverting ileostomy, was identified as the risk factor associated with readmission related to dehydration.
Keyword
Figure
Reference
-
1. Mrak K, Jagoditsch M, Eberl T, Klingler A, Tschmelitsch J. Long-term quality of life in pouch patients compared with stoma patients following rectal cancer surgery. Colorectal Dis. 2011; 13:e403–e410. PMID: 21812896.
Article2. Paun BC, Cassie S, MacLean AR, Dixon E, Buie WD. Postoperative complications following surgery for rectal cancer. Ann Surg. 2010; 251:807–818. PMID: 20395841.
Article3. Bennis M, Parc Y, Lefevre JH, Chafai N, Attal E, Tiret E. Morbidity risk factors after low anterior resection with total mesorectal excision and coloanal anastomosis: a retrospective series of 483 patients. Ann Surg. 2012; 255:504–510. PMID: 22281734.4. Kim CH, Lee J, Kwak HD, Lee SY, Ju JK, Kim HR. Tailored treatment of anastomotic leak after rectal cancer surgery according to the presence of a diverting stoma. Ann Surg Treat Res. 2020; 99:171–179. PMID: 32908849.
Article5. Hallböök O, Sjödahl R. Anastomotic leakage and functional outcome after anterior resection of the rectum. Br J Surg. 1996; 83:60–62. PMID: 8653367.
Article6. Tan WS, Tang CL, Shi L, Eu KW. Meta-analysis of defunctioning stomas in low anterior resection for rectal cancer. Br J Surg. 2009; 96:462–472. PMID: 19358171.
Article7. Tsikitis VL, Larson DW, Poola VP, Nelson H, Wolff BG, Pemberton JH, et al. Postoperative morbidity with diversion after low anterior resection in the era of neoadjuvant therapy: a single institution experience. J Am Coll Surg. 2009; 209:114–118. PMID: 19651071.
Article8. Bax TW, McNevin MS. The value of diverting loop ileostomy on the high-risk colon and rectal anastomosis. Am J Surg. 2007; 193:585–588. PMID: 17434360.
Article9. Mala T, Nesbakken A. Morbidity related to the use of a protective stoma in anterior resection for rectal cancer. Colorectal Dis. 2008; 10:785–788. PMID: 18190612.
Article10. Thalheimer A, Bueter M, Kortuem M, Thiede A, Meyer D. Morbidity of temporary loop ileostomy in patients with colorectal cancer. Dis Colon Rectum. 2006; 49:1011–1017. PMID: 16598401.
Article11. Giannakopoulos GF, Veenhof AA, van der Peet DL, Sietses C, Meijerink WJ, Cuesta MA. Morbidity and complications of protective loop ileostomy. Colorectal Dis. 2009; 11:609–612. PMID: 19175642.
Article12. Chude GG, Rayate NV, Patris V, Koshariya M, Jagad R, Kawamoto J, et al. Defunctioning loop ileostomy with low anterior resection for distal rectal cancer: should we make an ileostomy as a routine procedure?: a prospective randomized study. Hepatogastroenterology. 2008; 55:1562–1567. PMID: 19102343.13. Chow A, Tilney HS, Paraskeva P, Jeyarajah S, Zacharakis E, Purkayastha S. The morbidity surrounding reversal of defunctioning ileostomies: a systematic review of 48 studies including 6,107 cases. Int J Colorectal Dis. 2009; 24:711–723. PMID: 19221766.
Article14. Mansfield SD, Jensen C, Phair AS, Kelly OT, Kelly SB. Complications of loop ileostomy closure: a retrospective cohort analysis of 123 patients. World J Surg. 2008; 32:2101–2106. PMID: 18563482.
Article15. Saha AK, Tapping CR, Foley GT, Baker RP, Sagar PM, Burke DA, et al. Morbidity and mortality after closure of loop ileostomy. Colorectal Dis. 2009; 11:866–871. PMID: 19175627.
Article16. Wong KS, Remzi FH, Gorgun E, Arrigain S, Church JM, Preen M, et al. Loop ileostomy closure after restorative proctocolectomy: outcome in 1,504 patients. Dis Colon Rectum. 2005; 48:243–250. PMID: 15714246.
Article17. Rathnayake MM, Kumarage SK, Wijesuriya SR, Munasinghe BN, Ariyaratne MH, Deen KI. Complications of loop ileostomy and ileostomy closure and their implications for extended enterostomal therapy: a prospective clinical study. Int J Nurs Stud. 2008; 45:1118–1121. PMID: 18082164.
Article18. Shabbir J, Britton DC. Stoma complications: a literature overview. Colorectal Dis. 2010; 12:958–964. PMID: 19604288.
Article19. Salvadalena G. Incidence of complications of the stoma and peristomal skin among individuals with colostomy, ileostomy, and urostomy: a systematic review. J Wound Ostomy Continence Nurs. 2008; 35:596–607. PMID: 19018200.20. Fazio VW, Tjandra JJ. Prevention and management of ileostomy complications. J ET Nurs. 1992; 19:48–53. PMID: 1558860.
Article21. Azimuddin K, Rosen L, Reed JF 3rd, Stasik JJ, Riether RD, Khubchandani IT. Readmissions after colorectal surgery cannot be predicted. Dis Colon Rectum. 2001; 44:942–946. PMID: 11496073.
Article22. Kariv Y, Wang W, Senagore AJ, Hammel JP, Fazio VW, Delaney CP. Multivariable analysis of factors associated with hospital readmission after intestinal surgery. Am J Surg. 2006; 191:364–371. PMID: 16490548.
Article23. Snow N, Bergin KT, Horrigan TP. Readmission of patients to the surgical intensive care unit: patient profiles and possibilities for prevention. Crit Care Med. 1985; 13:961–964. PMID: 4053645.24. Doumouras AG, Tsao MW, Saleh F, Hong D. A population-based comparison of 30-day readmission after surgery for colon and rectal cancer: how are they different? J Surg Oncol. 2016; 114:354–360. PMID: 27334402.
Article25. O'Connell EP, Healy V, Fitzpatrick F, Higgins CA, Burke JP, McNamara DA. Predictors of readmission following proctectomy for rectal cancer. Dis Colon Rectum. 2019; 62:703–710. PMID: 30762598.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Single port–assisted diverting ileostomy formation for anastomotic leakage after low anterior resection
- The Relationship Between High-Output Stomas, Postoperative Ileus, and Readmission After Rectal Cancer Surgery With Diverting Ileostomy
- Predisposing factors for high output stoma in patients with a diverting loop ileostomy after colorectal surgeries
- The Role of Diverting Stoma After an Ultra-low Anterior Resection for Rectal Cancer
- Risk factors of stoma re-creation after closure of diverting ileostomy in patients with rectal cancer who underwent low anterior resection or intersphincteric resection with loop ileostomy