Diabetes Metab J.
2021 Jul;45(4):569-577. 10.4093/dmj.2020.0103.
Metabolic Syndrome Severity Score for Predicting Cardiovascular Events: A Nationwide Population-Based Study from Korea
- Affiliations
-
- 1Yonsei University Wonju College of Medicine, Wonju, Korea
- 2Department of Biostatistics, Yonsei University Wonju College of Medicine, Wonju, Korea
- 3Department of Precision Medicine & Biostatistics, Yonsei University Wonju College of Medicine, Wonju, Korea
- 4Big Data Streering Department, National Health Insurance Service, Wonju, Korea
- 5Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea
- 6Division of Endocrinology and Metabolism, Department of Internal Medicine, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea
- KMID: 2518899
- DOI: http://doi.org/10.4093/dmj.2020.0103
Abstract
- Background
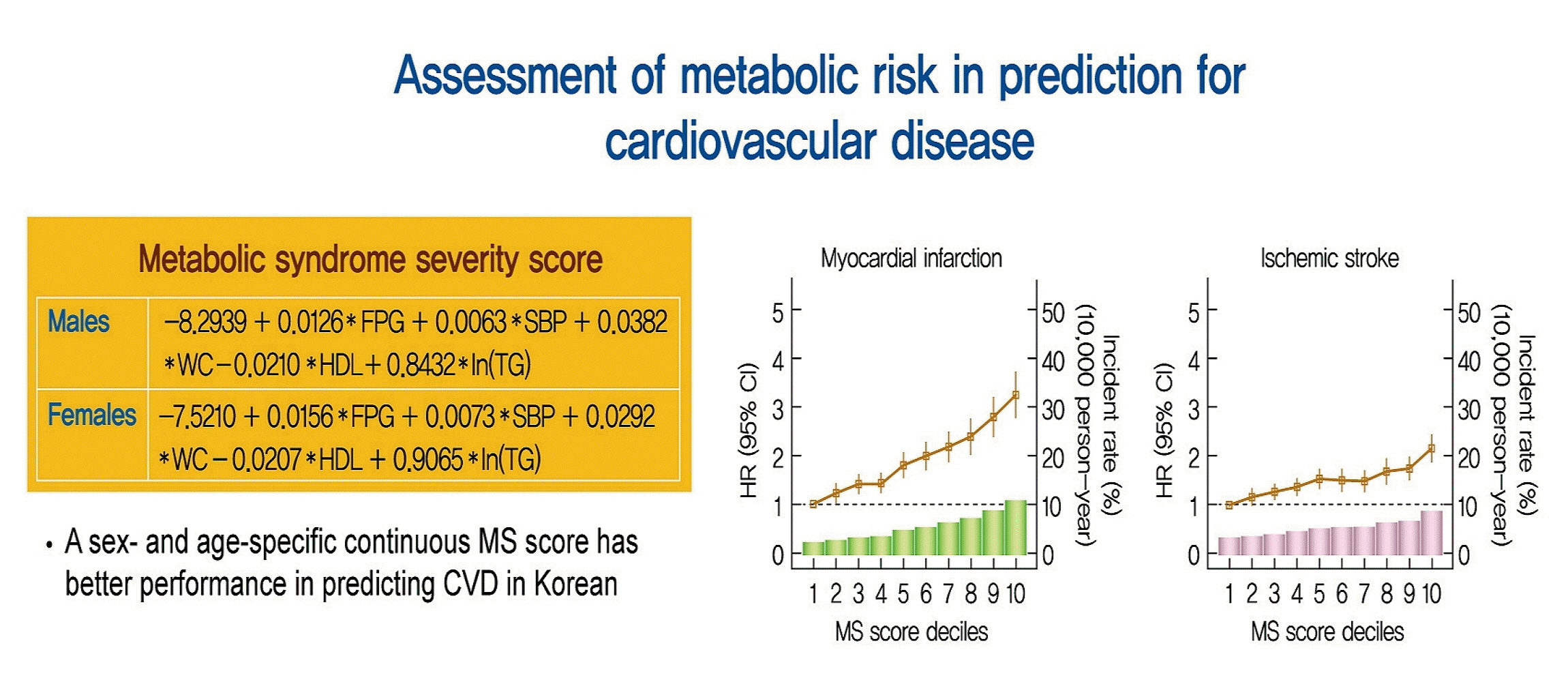
Recently, a metabolic syndrome severity score (MS score) using a dataset of the Korea National Health and Nutrition Examination Surveys has been developed. We aimed to determine whether the newly developed score is a significant predictor of cardiovascular (CV) events among the Korean population.
Methods
From the Korean National Health Insurance System, 2,541,364 (aged 40 to 59 years) subjects with no history of CV events (ischemic stroke or myocardial infarction [MI]), who underwent health examinations from 2009 to 2011 and were followed up until 2014 to 2017, were identified. Cox proportional hazard model was employed to investigate the association between MS score and CV events. Model performance of MS score for predicting CV events was compared to that of conventional metabolic syndrome diagnostic criteria (Adult Treatment Program III [ATP-III]) using the Akaike information criterion and the area under the receiver operating characteristic curve.
Results
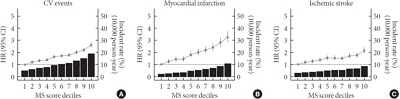
Over a median follow-up of 6 years, 15,762 cases of CV events were reported. MS score at baseline showed a linear association with incident CV events. In the multivariable-adjusted model, the hazard ratios (95% confidence intervals) comparing the highest versus lowest quartiles of MS score were 1.48 (1.36 to 1.60) for MI and 1.89 (1.74 to 2.05) for stroke. Model fitness and performance of the MS score in predicting CV events were superior to those of ATP-III.
Conclusion
The newly developed age- and sex-specific continuous MS score for the Korean population is an independent predictor of ischemic stroke and MI in Korean middle-aged adults even after adjusting for confounding factors.
Figure
Cited by 1 articles
-
Harnessing Metabolic Indices as a Predictive Tool for Cardiovascular Disease in a Korean Population without Known Major Cardiovascular Event
Hyun-Jin Kim, Byung Sik Kim, Yonggu Lee, Sang Bong Ahn, Dong Wook Kim, Jeong-Hun Shin
Diabetes Metab J. 2024;48(3):449-462. doi: 10.4093/dmj.2023.0197.
Reference
-
1. Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002; 288:2709–16.
Article2. Gurka MJ, Guo Y, Filipp SL, DeBoer MD. Metabolic syndrome severity is significantly associated with future coronary heart disease in type 2 diabetes. Cardiovasc Diabetol. 2018; 17:17.
Article3. DeBoer MD, Gurka MJ. Clinical utility of metabolic syndrome severity scores: considerations for practitioners. Diabetes Metab Syndr Obes. 2017; 10:65–72.
Article4. Huh JH, Yadav D, Kim JS, Son JW, Choi E, Kim SH, et al. An association of metabolic syndrome and chronic kidney disease from a 10-year prospective cohort study. Metabolism. 2017; 67:54–61.
Article5. Ford ES. Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: a summary of the evidence. Diabetes Care. 2005; 28:1769–78.
Article6. Soldatovic I, Vukovic R, Culafic D, Gajic M, Dimitrijevic-Sreckovic V. siMS score: simple method for quantifying metabolic syndrome. PLoS One. 2016; 11:e0146143.
Article7. Huh JH, Lee JH, Moon JS, Sung KC, Kim JY, Kang DR. Metabolic syndrome severity score in Korean adults: analysis of the 2010-2015 Korea National Health and Nutrition Examination Survey. J Korean Med Sci. 2019; 34:e48.
Article8. Gurka MJ, Lilly CL, Oliver MN, DeBoer MD. An examination of sex and racial/ethnic differences in the metabolic syndrome among adults: a confirmatory factor analysis and a resulting continuous severity score. Metabolism. 2014; 63:218–25.
Article9. Andersen LB, Harro M, Sardinha LB, Froberg K, Ekelund U, Brage S, et al. Physical activity and clustered cardiovascular risk in children: a cross-sectional study (The European Youth Heart Study). Lancet. 2006; 368:299–304.
Article10. Brage S, Wedderkopp N, Ekelund U, Franks PW, Wareham NJ, Andersen LB, et al. Features of the metabolic syndrome are associated with objectively measured physical activity and fitness in Danish children: the European Youth Heart Study (EYHS). Diabetes Care. 2004; 27:2141–8.
Article11. Batey LS, Goff DC Jr, Tortolero SR, Nichaman MZ, Chan W, Chan FA, et al. Summary measures of the insulin resistance syndrome are adverse among Mexican-American versus non-Hispanic white children: the Corpus Christi Child Heart Study. Circulation. 1997; 96:4319–25.12. Katzmarzyk PT, Perusse L, Malina RM, Bergeron J, Despres JP, Bouchard C. Stability of indicators of the metabolic syndrome from childhood and adolescence to young adulthood: the Quebec Family Study. J Clin Epidemiol. 2001; 54:190–5.13. DeBoer MD, Gurka MJ, Woo JG, Morrison JA. Severity of metabolic syndrome as a predictor of cardiovascular disease between childhood and adulthood: the Princeton Lipid Research Cohort Study. J Am Coll Cardiol. 2015; 66:755–7.14. Seong SC, Kim YY, Park SK, Khang YH, Kim HC, Park JH, et al. Cohort profile: the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open. 2017; 7:e016640.
Article15. Kim MK, Han K, Kim HS, Park YM, Kwon HS, Yoon KH, et al. Cholesterol variability and the risk of mortality, myocardial infarction, and stroke: a nationwide population-based study. Eur Heart J. 2017; 38:3560–6.
Article16. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005; 112:2735–52.17. Lee SY, Park HS, Kim DJ, Han JH, Kim SM, Cho GJ, et al. Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabetes Res Clin Pract. 2007; 75:72–80.
Article18. Huh JH, Ahn SG, Kim YI, Go T, Sung KC, Choi JH, et al. Impact of longitudinal changes in metabolic syndrome status over 2 years on 10-year incident diabetes mellitus. Diabetes Metab J. 2019; 43:530–8.
Article19. de Ferranti S, Mozaffarian D. The perfect storm: obesity, adipocyte dysfunction, and metabolic consequences. Clin Chem. 2008; 54:945–55.
Article20. DeBoer MD. Obesity, systemic inflammation, and increased risk for cardiovascular disease and diabetes among adolescents: a need for screening tools to target interventions. Nutrition. 2013; 29:379–86.
Article21. Guo Y, Musani SK, Sims M, Pearson TA, DeBoer MD, Gurka MJ. Assessing the added predictive ability of a metabolic syndrome severity score in predicting incident cardiovascular disease and type 2 diabetes: the Atherosclerosis Risk in Communities Study and Jackson Heart Study. Diabetol Metab Syndr. 2018; 10:42.
Article22. Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001; 24:683–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Harnessing Metabolic Indices as a Predictive Tool for Cardiovascular Disease in a Korean Population without Known Major Cardiovascular Event
- Letter: Triglyceride-Glucose Index Predicts Cardiovascular Outcome in Metabolically Unhealthy Obese Population: A Nationwide Population-Based Cohort Study (J Obes Metab Syndr 2022;31:178-86)
- Understanding Cardiovascular-Kidney-Metabolic Syndrome and the Necessity of a Multidisciplinary Approach
- Relationship between Metabolic Syndrome and Triglyceride/High-density Lipoprotein Cholesterol Ratio
- Metabolic syndrome induced by anticancer treatment in childhood cancer survivors