Clin Endosc.
2021 Jul;54(4):555-562. 10.5946/ce.2020.229.
Diode Laser—Can It Replace the Electrical Current Used in Endoscopic Submucosal Dissection? (with Video)
- Affiliations
-
- 1Department of Internal Medicine, Soonchunhyang University College of Medicine, Cheonan, Korea
- 2Department of Internal Medicine, Hallym University College of Medicine, Chuncheon, Korea
- 3Department of Internal Medicine, Inha University School of Medicine, Incheon, Korea
- 4Department of Internal Medicine, Soonchunhyang University College of Medicine, Bucheon, Korea
- 5Department of Internal Medicine, Nowon Eulji Medical Center, Eulji University College of Medicine, Seoul, Korea
- 6Department of Internal Medicine, Dong-A University College of Medicine, Busan, Korea
- 7Department of Gastroenterology and Hepatology, College of Medicine, Kyung Hee University, Seoul, Korea
- 8Department of Internal Medicine, Chonnam National University Hwasun Hospital, Gwangju, Korea
- 9Department of Gastroenterology, Ajou University School of Medicine, Suwon, Korea
- 10Department of Internal Medicine, Chungnam National University Hospital, Daejeon, Korea
- 11Division of Gastroenterology, Department of Internal Medicine, CHA Bundang Medical Center, Seongnam, Korea
- KMID: 2518859
- DOI: http://doi.org/10.5946/ce.2020.229
Abstract
- Background/Aims
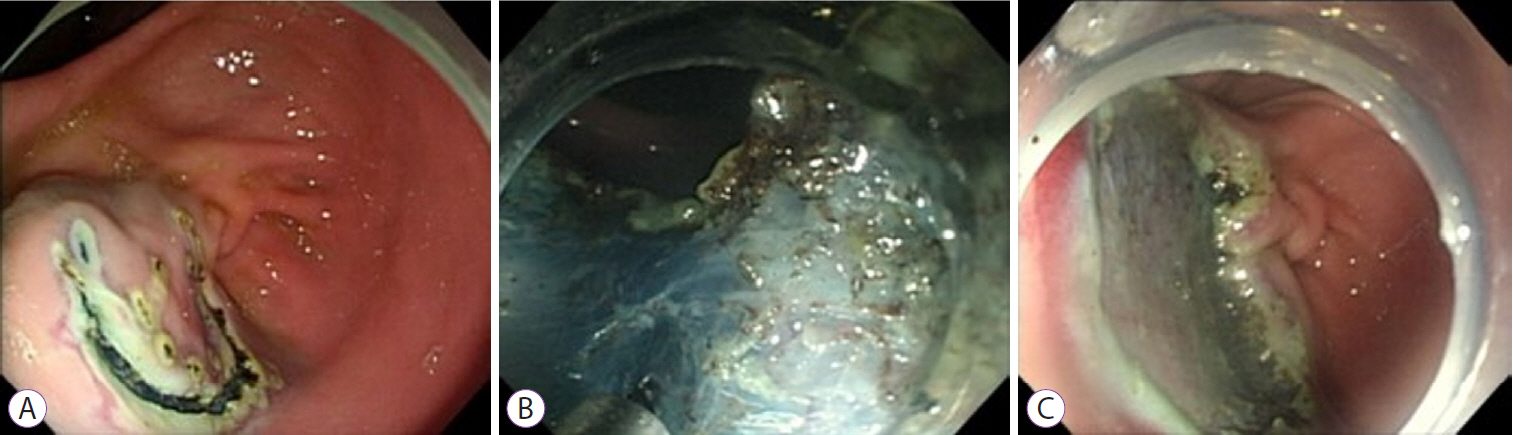
A new medical fiber-guided diode laser system (FDLS) is expected to offer high-precision cutting with simultaneous hemostasis. Thus, this study aimed to evaluate the feasibility of using the 1,940-nm FDLS to perform endoscopic submucosal dissection (ESD) in the gastrointestinal tract of an animal model.
Methods
In this prospective animal pilot study, gastric and colorectal ESD using the FDLS was performed in ex vivo and in vivo porcine models. The completeness of en bloc resection, the procedure time, intraprocedural bleeding, histological injuries to the muscularis propria (MP) layer, and perforation were assessed.
Results
The en bloc resection and perforation rates in the ex vivo study were 100% (10/10) and 10% (1/10), respectively; those in the in vivo study were 100% (4/4) and 0% for gastric ESD and 100% (4/4) and 25% (1/4) for rectal ESD, respectively. Deep MP layer injuries tended to occur more frequently in the rectal than in the gastric ESD cases, and no intraprocedural bleeding occurred in either group.
Conclusions
The 1,940-nm FDLS was capable of yielding high en bloc resection rates without intraprocedural bleeding during gastric and colorectal ESD in animal models.
Keyword
Figure
Reference
-
1. Bhatt A, Abe S, Kumaravel A, Vargo J, Saito Y. Indications and techniques for endoscopic submucosal dissection. Am J Gastroenterol. 2015; 110:784–791.
Article2. Belderbos TD, Leenders M, Moons LM, Siersema PD. Local recurrence after endoscopic mucosal resection of nonpedunculated colorectal lesions: systematic review and meta-analysis. Endoscopy. 2014; 46:388–402.
Article3. Ko BM. History and development of accessories for endoscopic submucosal dissection. Clin Endosc. 2017; 50:219–223.
Article4. Horikawa Y, Fushimi S, Sato S. Hemorrhage control during gastric endoscopic submucosal dissection: techniques using uncovered knives. JGH Open. 2020; 4:4–10.
Article5. Goto O, Fujishiro M, Oda I, et al. A multicenter survey of the management after gastric endoscopic submucosal dissection related to postoperative bleeding. Dig Dis Sci. 2012; 57:435–439.
Article6. Park YM, Cho E, Kang HY, Kim JM. The effectiveness and safety of endoscopic submucosal dissection compared with endoscopic mucosal resection for early gastric cancer: a systematic review and metaanalysis. Surg Endosc. 2011; 25:2666–2677.
Article7. Jang JS, Choi SR, Graham DY, et al. Risk factors for immediate and delayed bleeding associated with endoscopic submucosal dissection of gastric neoplastic lesions. Scand J Gastroenterol. 2009; 44:1370–1376.
Article8. Reumkens A, Rondagh EJ, Bakker CM, Winkens B, Masclee AA, Sanduleanu S. Post-colonoscopy complications: a systematic review, time trends, and meta-analysis of population-based studies. Am J Gastroenterol. 2016; 111:1092–1101.
Article9. Kichler A, Jang S. Endoscopic hemostasis for non-variceal upper gastrointestinal bleeding: new frontiers. Clin Endosc. 2019; 52:401–406.
Article10. Noguchi T, Hazama H, Nishimura T, Morita Y, Awazu K. Enhancement of the safety and efficacy of colorectal endoscopic submucosal dissection using a CO2 laser. Lasers Med Sci. 2020; 35:421–427.11. Obata D, Morita Y, Kawaguchi R, et al. Endoscopic submucosal dissection using a carbon dioxide laser with submucosally injected laser absorber solution (porcine model). Surg Endosc. 2013; 27:4241–4249.
Article12. Saccomandi P, Quero G, Costamagna G, Diana M, Marescaux J. Effects of Nd:YAG laser for the controlled and localized treatment of early gastrointestinal tumors: preliminary in vivo study. Annu Int Conf IEEE Eng Med Biol Soc. 2017; 2017:4533–4536.
Article13. Cho JH, Cho JY, Kim MY, et al. Endoscopic submucosal dissection using a thulium laser: preliminary results of a new method for treatment of gastric epithelial neoplasia. Endoscopy. 2013; 45:725–728.
Article14. Tang J, Ye S, Ji X, Li J, Liu F. Comparison of synchronous dual wavelength diode laser versus conventional endo-knives for esophageal endoscopic submucosal dissection: an animal study. Surg Endosc. 2018; 32:5037–5043.
Article15. Tanaka S, Kashida H, Saito Y, et al. Japan gastroenterological endoscopy society guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc. 2020; 32:219–239.
Article16. Kato M, Gromski M, Jung Y, Chuttani R, Matthes K. The learning curve for endoscopic submucosal dissection in an established experimental setting. Surg Endosc. 2013; 27:154–161.
Article17. Yoshida M, Kakushima N, Mori K, et al. Learning curve and clinical outcome of gastric endoscopic submucosal dissection performed by trainee operators. Surg Endosc. 2017; 31:3614–3622.
Article18. Rönnow CF, Uedo N, Toth E, Thorlacius H. Endoscopic submucosal dissection of 301 large colorectal neoplasias: outcome and learning curve from a specialized center in Europe. Endosc Int Open. 2018; 6:E1340–E1348.
Article19. Iacopini F, Saito Y, Bella A, et al. Colorectal endoscopic submucosal dissection: predictors and neoplasm-related gradients of difficulty. Endosc Int Open. 2017; 5:E839–E846.
Article20. Oka S, Tanaka S, Kaneko I, et al. Advantage of endoscopic submucosal dissection compared with EMR for early gastric cancer. Gastrointest Endosc. 2006; 64:877–883.
Article21. Zhang J, Li J, Wang X, Shi C, Tu M, Shi G. Efficacy and safety of 1470- nm diode laser enucleation of the prostate in individuals with benign prostatic hyperplasia continuously administered oral anticoagulants or antiplatelet drugs. Urology. 2020; 138:129–133.22. Aktas AR, Celik O, Ozkan U, et al. Comparing 1470- and 980-nm diode lasers for endovenous ablation treatments. Lasers Med Sci. 2015; 30:1583–1587.
Article23. Kang K, Kim H, Kim JH, et al. The feasibility of 1940-nm diode laser in tonsillectomy. Medical Lasers. 2016; 5:77–82.
Article24. Khoder WY, Sroka R, Siegert S, Stief CG, Becker AJ. Outcome of laser-assisted laparoscopic partial nephrectomy without ischaemia for peripheral renal tumours. World J Urol. 2012; 30:633–638.
Article25. Guney M, Tunc B, Gulsoy M. Investigating the ablation efficiency of a 1940-nm thulium fibre laser for intraoral surgery. Int J Oral Maxillofac Surg. 2014; 43:1015–1021.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- History and Development of Accessories for Endoscopic Submucosal Dissection
- The Current Status of Endoscopic Submucosal Dissection
- Treatment of Early Gastric Cancer: Endoscopic Submucosal Dissection with LASER
- Papillary Adenocarcinoma
- Comparison of Photocoagulation with the Argon and Diode Laser in Rabbit Eyes