Clin Endosc.
2021 Jul;54(4):534-541. 10.5946/ce.2021.071.
Acute Gastrointestinal Bleeding in COVID-19 Patients: A Systematic Review and Meta-Analysis
- Affiliations
-
- 1Department of Gastroenterology and Hepatology, Geisinger Medical Center, Danville, PA, USA
- 2Department of Internal Medicine, Capital Health Regional Medical Center, Trenton, NJ, USA
- 3Department of Surgery, Cleveland Clinic Foundation, Cleveland, OH, USA
- 4Department of Gastroenterology and Hepatology, The University of Texas, MD Anderson Cancer Center Houston, TX, USA
- 5Department of Gastroenterology and Hepatology, University of Tennessee at Memphis Health Sciences Center, Memphis, TN, USA
- KMID: 2518856
- DOI: http://doi.org/10.5946/ce.2021.071
Abstract
- Background/Aims
More than 100 million people to date have been affected by the coronavirus disease-2019 (COVID-19) pandemic. Patients with COVID-19 have a higher risk of bleeding complications. We performed a systematic review and meta-analysis to evaluate the outcomes of COVID-19 patients with signs and symptoms of acute gastrointestinal bleeding (GIB).
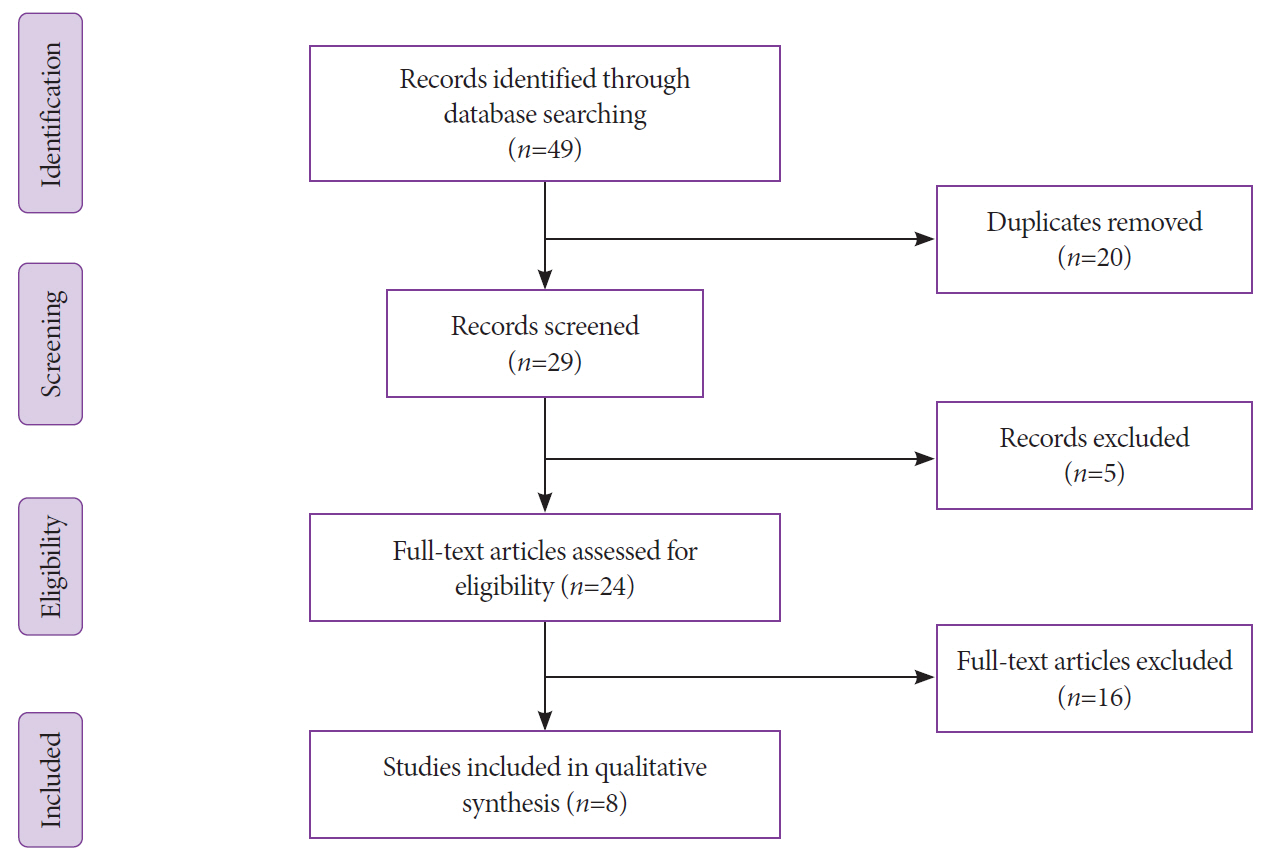
Methods
A systematic literature search was carried out for articles published until until November 11, 2020, in the Embase, MEDLINE, Web of Science, and Cochrane Library databases. We included studies on COVID-19 patients with signs and symptoms of GIB.
Results
Our search yielded 49 studies, of which eight with a collective 127 patients (86 males and 41 females) met our inclusion criteria. Conservative management alone was performed in 59% of the patients, endoscopic evaluation in 31.5%, and interventional radiology (IR) embolization in 11%. Peptic ulcer disease was the most common endoscopic finding, diagnosed in 47.5% of the patients. Pooled overall mortality was 19.1% (95% confidence interval [CI]; 12.7%-27.6%) and pooled mortality secondary to GIB was 3.5% (95% CI; 1.3%–9.1%). The pooled risk of rebleeding was 11.3% (95% CI; 6.8%–18.4%).
Conclusion
The majority of COVID-19 patients with GIB responded to conservative management, with a low mortality rate associated with GIB and the risk of rebleeding. Thus, we suggest limiting endoscopic and IR interventions to those with hemodynamic instability and those for whom conservative management was unsuccessful.
Figure
Reference
-
1. Grant MC, Geoghegan L, Arbyn M, et al. The prevalence of symptoms in 24,410 adults infected by the novel coronavirus (SARS-CoV-2; COVID-19): a systematic review and meta-analysis of 148 studies from 9 countries. PLoS One. 2020; 15:e0234765.
Article2. Suresh Kumar VC, Mukherjee S, Harne PS, et al. Novelty in the gut: a systematic review and meta-analysis of the gastrointestinal manifestations of COVID-19. BMJ Open Gastroenterol. 2020; 7:e000417.
Article3. Buscarini E, Manfredi G, Brambilla G, et al. GI symptoms as early signs of COVID-19 in hospitalised Italian patients. Gut. 2020; 69:1547–1548.
Article4. Peery AF, Crockett SD, Murphy CC, et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2018. Gastroenterology. 2019; 156:254–272.e11.
Article5. WHO Rapid Evidence Appraisal for COVID-19 Therapies (REACT) Working Group, Sterne JAC, Murthy S, et al. Association between administration of systemic corticosteroids and mortality among critically ill patients with COVID-19: a meta-analysis. JAMA. 2020; 324:1330–1341.6. Bilaloglu S, Aphinyanaphongs Y, Jones S, Iturrate E, Hochman J, Berger JS. Thrombosis in hospitalized patients with COVID-19 in a New York City Health System. JAMA. 2020; 324:799–801.
Article7. Pappa S, Ntella V, Giannakas T, Giannakoulis VG, Papoutsi E, Katsaounou P. Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav Immun. 2020; 88:901–907.
Article8. Gondi S, Beckman AL, Deveau N, et al. Personal protective equipment needs in the USA during the COVID-19 pandemic. Lancet. 2020; 395:e90–e91.
Article9. Laine L, Jensen DM. Management of patients with ulcer bleeding. Am J Gastroenterol. 2012; 107:345–360. quiz 361.
Article10. Strate LL, Gralnek IM. ACG clinical guideline: management of patients with acute lower gastrointestinal bleeding. Am J Gastroenterol. 2016; 111:459–474.
Article11. Buckholz A, Kaplan A, Jessurun J, De Jong Y, Crawford C. Microthrombosis associated with GI bleeding in COVID-19. Gastrointest Endosc. 2021; 93:263–264.
Article12. Carvalho A, Alqusairi R, Adams A, et al. SARS-CoV-2 gastrointestinal infection causing hemorrhagic colitis: implications for detection and transmission of COVID-19 disease. Am J Gastroenterol. 2020; 115:942–946.
Article13. Cho M, Liu W, Balzora S, et al. Clinical and intestinal histopathological findings in SARS-CoV-2/COVID-19 patients with hematochezia. Case Rep Gastroenterol. 2021; 15:408–417.
Article14. Gadiparthi C, Perisetti A, Sayana H, Tharian B, Inamdar S, Korman A. Gastrointestinal bleeding in patients with severe SARS-CoV-2. Am J Gastroenterol. 2020; 115:1283–1285.
Article15. Gulen M, Satar S. Uncommon presentation of COVID-19: gastrointestinal bleeding. Clin Res Hepatol Gastroenterol. 2020; 44:e72–e76.
Article16. Guotao L, Xingpeng Z, Zhihui D, Huirui W. SARS-CoV-2 infection presenting with hematochezia. Med Mal Infect. 2020; 50:293–296.
Article17. Li X, Huang S, Lu J, et al. Upper gastrointestinal bleeding caused by SARS-CoV-2 infection. Am J Gastroenterol. 2020; 115:1541–1542.
Article18. Marchi G, Vianello A, Crisafulli E, et al. Cytomegalovirus-induced gastrointestinal bleeding and pancreatitis complicating severe COVID-19 pneumonia: a paradigmatic case. Mediterr J Hematol Infect Dis. 2020; 12:e2020060.
Article19. Zhang L-B, Pang R-R, Qiao Q-H, et al. Successful recovery of COVID-19-associated recurrent diarrhea and gastrointestinal hemorrhage using convalescent plasma. Mil Med Res. 2020; 7:45.
Article20. Mauro A, De Grazia F, Lenti MV, et al. Upper gastrointestinal bleeding in COVID-19 inpatients: incidence and management in a multicenter experience from Northern Italy. Clin Res Hepatol Gastroenterol. 2020; 101521.
Article21. Martin TA, Wan DW, Hajifathalian K, et al. Gastrointestinal bleeding in patients with coronavirus disease 2019: a matched case-control study. Am J Gastroenterol. 2020; 115:1609–1616.
Article22. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009; 6:e1000097.
Article23. Shalimar null, Vaishnav M, Elhence A, et al. Outcome of conservative therapy in coronavirus disease-2019 patients presenting with gastrointestinal bleeding. J Clin Exp Hepatol. 2021; 11:327–333.
Article24. Holzwanger EA, Bilal M, Stallwood CG, Sterling MJ, Yacavone RF. Acute lower gastrointestinal bleeding during the COVID-19 pandemic - less is more! Endoscopy. 2020; 52:816–817.
Article25. Ierardi AM, Del Giudice C, Coppola A, et al. Gastrointestinal hemorrhages in patients with COVID-19 managed with transarterial embolization. Am J Gastroenterol. 2021; 116:838–840.
Article26. Cavaliere K, Levine C, Wander P, Sejpal DV, Trindade AJ. Management of upper GI bleeding in patients with COVID-19 pneumonia. Gastrointest Endosc. 2020; 92:454–455.
Article27. Barrett LF, Lo KB, Stanek SR, Walter JW. Self-limited gastrointestinal bleeding in COVID-19. Clin Res Hepatol Gastroenterol. 2020; 44:e77–e80.
Article28. Melazzini F, Lenti MV, Mauro A, De Grazia F, Di Sabatino A. Peptic ulcer disease as a common cause of bleeding in patients with coronavirus disease 2019. Am J Gastroenterol. 2020; 115:1139–1140.
Article29. Lin L, Jiang X, Zhang Z, et al. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut. 2020; 69:997–1001.
Article30. Klok FA, Kruip MJHA, van der Meer NJM, et al. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020; 191:145–147.
Article31. RECOVERY Collaborative Group, Horby P, Lim WS, et al. Dexamethasone in hospitalized patients with COVID-19. N Engl J Med. 2021; 384:693–704.
Article32. Plummer MP, Blaser AR, Deane AM. Stress ulceration: prevalence, pathology and association with adverse outcomes. Crit Care. 2014; 18:213.
Article33. PEPTIC Investigators for the Australian and New Zealand Intensive Care Society Clinical Trials Group; Alberta Health Services Critical Care Strategic Clinical Network; the Irish Critical Care Trials Group, et al. Effect of stress ulcer prophylaxis with proton pump inhibitors vs histamine-2 receptor blockers on in-hospital mortality among ICU patients receiving invasive mechanical ventilation: the PEPTIC randomized clinical trial. JAMA. 2020; 323:616–626.34. Massironi S, Viganò C, Dioscoridi L, et al. Endoscopic findings in patients infected with 2019 novel coronavirus in lombardy, Italy. Clin Gastroenterol Hepatol. 2020; 18:2375–2377.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Prevalence of Post-Traumatic Stress Disorder in the General Population during the COVID-19 Pandemic: A Systematic Review and Single-Arm Meta-Analysis
- Trends of Meta-analysis in Upper Gastrointestinal Diseases
- Predictors of Mortality in Patients with COVID-19: A Systematic Review and Meta-analysis
- Depression in pregnant and postpartum women during COVID-19 pandemic: systematic review and meta-analysis
- The role of vitamin D deficiency on COVID-19: a systematic review and meta-analysis of observational studies