Nutr Res Pract.
2021 Aug;15(4):516-527. 10.4162/nrp.2021.15.4.516.
Relationship between psychological distress and the adherence to the Korean healthy eating index (KHEI): the Korea National Health and Nutrition Examination Survey (KNHANES) 2013 and 2015
- Affiliations
-
- 1Department of Family Medicine, Inje University Ilsan Paik Hospital, Goyang 10380, Korea
- 2Department of Family Medicine, Center for Obesity, Metabolism, and Nutrition, Dongguk University Ilsan Hospital, Goyang 10326, Korea
- KMID: 2518764
- DOI: http://doi.org/10.4162/nrp.2021.15.4.516
Abstract
- BACKGROUND/OBJECTIVES
This study examined the association of depressive symptoms, stress perception, and suicidal ideation with overall dietary quality using the newly developed Korean healthy eating index (KHEI).
SUBJECTS/METHODS
This study included 9,607 adults (3,939 men and 5,668 women, ≥ 19 years) who participated in the 6th Korea National Health and Nutrition Examination Survey 2013 and 2015. The KHEI scores were calculated using the food frequency questionnaire data. Survey logistic regression analyses were performed to analyze the association between psychiatric distress and dietary quality.
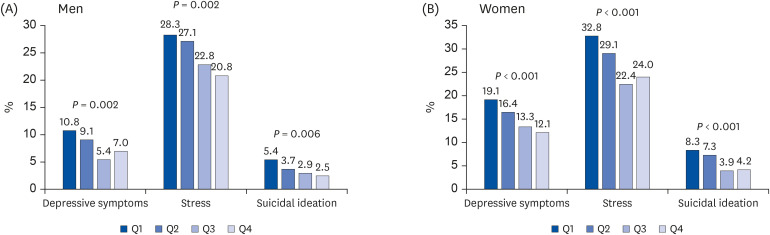
RESULTS
The percentage of subjects with experience of depressive mood, higher stress perception, and suicidal ideation was 8.2%, 25.0%, and 3.7% in men and 15.4%, 27.3%, and 6.0% in women, respectively. The mean KHEI score was 61.5 ± 0.29 in men and 64.8 ± 0.24 in women (P < 0.001). The present study found a difference in the adherence to specific dietary components of the KHEI between sexes. Men experiencing depressive symptoms were less likely to eat meat, fish, eggs, and beans, while depressed women showed lower vegetable intake. Both men and women with suicidal ideation showed a lower intake of vegetables. The men with stress had a lower breakfast eating score than those without stress (7.21 vs. 6.77, P = 0.016). The multivariate-adjusted odds ratios for depressive symptoms, stress perception, and the suicidal idea in women with the highest quartile of KHEI scores compared to the lowest quartile was 0.69 (95% confidence interval, 0.51–0.92), 0.73 (0.58–0.82), and 0.52 (0.33–0.82), respectively and significant dose-response associations were observed (P for trends < 0.05 for all). On the other hand, these associations were not observed in men after adjusting for the confounding variables (P for trends > 0.05 for all).
CONCLUSIONS
Poor adherence to dietary recommendations is associated with psychological distress, especially in women.
Keyword
Figure
Reference
-
1. Ministry of Health & Welfare. Epidemiological Survey of Mental Disorders in Korea. Sejong: Ministry of Health & Welfare;2016.2. Organisation for Economic Co-operation and Development. Suicide rates [Internet]. Paris: Organisation for Economic Co-operation and Development;2016. cited 2020 June 5. Available from: https://data.oecd.org/healthstat/suicide-rates.htm.3. Nicolaou M, Colpo M, Vermeulen E, Elstgeest LE, Cabout M, Gibson-Smith D, Knuppel A, Sini G, Schoenaker D, Mishra GD, et al. Association of a priori dietary patterns with depressive symptoms: a harmonised meta-analysis of observational studies. Psychol Med. 2020; 50:1872–1883. PMID: 31409435.4. Lassale C, Batty GD, Baghdadli A, Jacka F, Sánchez-Villegas A, Kivimäki M, Akbaraly T. Healthy dietary indices and risk of depressive outcomes: a systematic review and meta-analysis of observational studies. Mol Psychiatry. 2019; 24:965–986. PMID: 30254236.5. Park SJ, Kim MS, Lee HJ. The association between dietary pattern and depression in middle-aged Korean adults. Nutr Res Pract. 2019; 13:316–322. PMID: 31388408.
Article6. Park SH, Han SH, Chang KJ. Comparison of nutrient intakes by nutritional anemia and the association between nutritional anemia and chronic diseases in Korean elderly: based on the 2013–2015 Korea National Health and Nutrition Examination Survey Data. Nutr Res Pract. 2019; 13:543–554. PMID: 31814930.
Article7. Yook SM, Park SH, Moon HK, Kim K, Shim J, Hwang JY. Development of Korean healthy eating index for adults using the Korea National Health and Nutrition Examination Survey data. J Nutr Health. 2015; 48:419–429.
Article8. Kwon AR, Yoon YS, Min KP, Lee YK, Jeon JH. Eating alone and metabolic syndrome: a population-based Korean National Health and Nutrition Examination Survey 2013–2014. Obes Res Clin Pract. 2018; 12:146–157. PMID: 29066025.
Article9. Lee J, Lee C, Min J, Kang DW, Kim JY, Yang HI, Park J, Lee MK, Lee MY, Park I, et al. Development of the Korean global physical activity questionnaire: reliability and validity study. Glob Health Promot. 2020; 27:44–55. PMID: 31375056.
Article10. Chun MY. Validity and reliability of Korean version of international physical activity questionnaire short form in the elderly. Korean J Fam Med. 2012; 33:144–151. PMID: 22787536.
Article11. Korea Centers for Disease Control and Prevention. Analytic Guidelines of the Fifth Korea National Health and Nutrition Examination Survey. Cheongju: Korea Centers for Disease Control and Prevention;2014.12. Rahmani J, Milajerdi A, Dorosty-Motlagh A. Association of the alternative healthy eating index (AHEI-2010) with depression, stress and anxiety among Iranian military personnel. J R Army Med Corps. 2018; 164:87–91. PMID: 28918388.
Article13. Abshire DA, Lennie TA, Chung ML, Biddle MJ, Barbosa-Leiker C, Moser DK. Body mass index category moderates the relationship between depressive symptoms and diet quality in overweight and obese rural-dwelling adults. J Rural Health. 2018; 34:377–387. PMID: 28686799.
Article14. Sánchez-Villegas A, Henríquez-Sánchez P, Ruiz-Canela M, Lahortiga F, Molero P, Toledo E, Martínez-González MA. A longitudinal analysis of diet quality scores and the risk of incident depression in the SUN project. BMC Med. 2015; 13:197. PMID: 26377327.
Article15. Appelhans BM, Whited MC, Schneider KL, Ma Y, Oleski JL, Merriam PA, Waring ME, Olendzki BC, Mann DM, Ockene IS, et al. Depression severity, diet quality, and physical activity in women with obesity and depression. J Acad Nutr Diet. 2012; 112:693–698. PMID: 22709773.
Article16. Errisuriz VL, Delfausse L, Villatoro AP, McDaniel MD, Esparza L, Parra-Medina D. Depression and physical activity affect diet quality of foreign-born Latina women living on the U.S.-Mexico border. Nutrients. 2019; 11:1254.
Article17. Quehl R, Haines J, Lewis SP, Buchholz AC. Food and mood: diet quality is inversely associated with depressive symptoms in female university students. Can J Diet Pract Res. 2017; 78:124–128. PMID: 28333547.
Article18. De Vriendt T, Clays E, Huybrechts I, De Bourdeaudhuij I, Moreno LA, Patterson E, Molnár D, Mesana MI, Beghin L, Widhalm K, et al. European adolescents' level of perceived stress is inversely related to their diet quality: the healthy lifestyle in Europe by nutrition in adolescence study. Br J Nutr. 2012; 108:371–380. PMID: 22054044.
Article19. Isasi CR, Parrinello CM, Jung MM, Carnethon MR, Birnbaum-Weitzman O, Espinoza RA, Penedo FJ, Perreira KM, Schneiderman N, Sotres-Alvarez D, et al. Psychosocial stress is associated with obesity and diet quality in Hispanic/Latino adults. Ann Epidemiol. 2015; 25:84–89. PMID: 25487969.
Article20. Widaman AM, Witbracht MG, Forester SM, Laugero KD, Keim NL. Chronic stress is associated with indicators of diet quality in habitual breakfast skippers. J Acad Nutr Diet. 2016; 116:1776–1784. PMID: 27161025.
Article21. Elstgeest LEM, Winkens LHH, Penninx BWJH, Brouwer IA, Visser M. Associations of depressive symptoms and history with three a priori diet quality indices in middle-aged and older adults. J Affect Disord. 2019; 249:394–403. PMID: 30822662.
Article22. St-Pierre M, Sinclair I, Elgbeili G, Bernard P, Dancause KN. Relationships between psychological distress and health behaviors among Canadian adults: differences based on gender, income, education, immigrant status, and ethnicity. SSM Popul Health. 2019; 7:100385. PMID: 31193063.
Article23. Sapranaviciute-Zabazlajeva L, Luksiene D, Virviciute D, Bobak M, Tamosiunas A. Link between healthy lifestyle and psychological well-being in Lithuanian adults aged 45–72: a cross-sectional study. BMJ Open. 2017; 7:e014240.
Article24. Brown CS, Kola-Palmer S, Dhingra K. Gender differences and correlates of extreme dieting behaviours in US adolescents. J Health Psychol. 2015; 20:569–579. PMID: 25903244.
Article25. Gibson-Smith D, Bot M, Brouwer IA, Visser M, Penninx BWJH. Diet quality in persons with and without depressive and anxiety disorders. J Psychiatr Res. 2018; 106:1–7. PMID: 30240962.
Article26. Xiao Y, Romanelli M, Lindsey MA. A latent class analysis of health lifestyles and suicidal behaviors among US adolescents. J Affect Disord. 2019; 255:116–126. PMID: 31150941.
Article27. Nanri A, Mizoue T, Poudel-Tandukar K, Noda M, Kato M, Kurotani K, Goto A, Oba S, Inoue M, Tsugane S. Japan Public Health Center-based Prospective Study Group. Dietary patterns and suicide in Japanese adults: the Japan public health center-based prospective study. Br J Psychiatry. 2013; 203:422–427. PMID: 24115342.
Article28. Zhang J, Li Y, Torres ME. How does a suicide attempter eat differently from others? Comparison of macronutrient intakes. Nutrition. 2005; 21:711–717. PMID: 15925296.
Article29. Perera S, Eisen RB, Bhatt M, Dennis BB, Bawor M, El-Sheikh W, DeJesus J, Rangarajan S, Sholer H, Iordan E, et al. Exploring metabolic factors and health behaviors in relation to suicide attempts: a case-control study. J Affect Disord. 2018; 229:386–395. PMID: 29331698.
Article30. Głąbska D, Guzek D, Groele B, Gutkowska K. Fruit and vegetable intake and mental health in adults: a systematic review. Nutrients. 2020; 12:115.
Article31. Francis HM, Stevenson RJ, Chambers JR, Gupta D, Newey B, Lim CK. A brief diet intervention can reduce symptoms of depression in young adults - A randomised controlled trial. PLoS One. 2019; 14:e0222768. PMID: 31596866.
Article32. Almogbel E, Aladhadh AM, Almotyri BH, Alhumaid AF, Rasheed N. Stress associated alterations in dietary behaviours of undergraduate students of Qassim university, Saudi Arabia. Open Access Maced J Med Sci. 2019; 7:2182–2188. PMID: 31456849.
Article33. Barrington WE, Beresford SA, McGregor BA, White E. Perceived stress and eating behaviors by sex, obesity status, and stress vulnerability: findings from the vitamins and lifestyle (VITAL) study. J Acad Nutr Diet. 2014; 114:1791–1799. PMID: 24828150.
Article34. Ahmed F, Al-Radhwan L, Al-Azmi GZS, Al-Beajan M. Association between stress and dietary behaviours among undergraduate students in Kuwait: gender differences. J Nutr Health Sci. 2014; 1:1–8.
Article35. Habhab S, Sheldon JP, Loeb RC. The relationship between stress, dietary restraint, and food preferences in women. Appetite. 2009; 52:437–444. PMID: 19135112.
Article36. Ferrer-Cascales R, Sánchez-SanSegundo M, Ruiz-Robledillo N, Albaladejo-Blázquez N, Laguna-Pérez A, Zaragoza-Martí A. Eat or skip breakfast? The important role of breakfast quality for health-related quality of life, stress and depression in Spanish adolescents. Int J Environ Res Public Health. 2018; 15:1781.
Article37. Richards G, Smith AP. Breakfast and energy drink consumption in secondary school children: breakfast omission, in isolation or in combination with frequent energy drink use, is associated with stress, anxiety, and depression cross-sectionally, but not at 6-month follow-up. Front Psychol. 2016; 7:106. PMID: 26903914.
Article38. Adjibade M, Lemogne C, Julia C, Hercberg S, Galan P, Assmann KE, Kesse-Guyot E. Prospective association between adherence to dietary recommendations and incident depressive symptoms in the French NutriNet-Santé cohort. Br J Nutr. 2018; 120:290–300. PMID: 29789039.
Article39. Molendijk M, Molero P, Ortuño Sánchez-Pedreño F, Van der Does W, Angel Martínez-González M. Diet quality and depression risk: a systematic review and dose-response meta-analysis of prospective studies. J Affect Disord. 2018; 226:346–354. PMID: 29031185.
Article40. Jacka FN, O'Neil A, Opie R, Itsiopoulos C, Cotton S, Mohebbi M, Castle D, Dash S, Mihalopoulos C, Chatterton ML, et al. A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial). BMC Med. 2017; 15:23. PMID: 28137247.
Article41. Gigantesco A, Morosini P. Development, reliability and factor analysis of a self-administered questionnaire which originates from the World Health Organization's composite international diagnostic interview - short form (CIDI-SF) for assessing mental disorders. Clin Pract Epidemol Ment Health. 2008; 4:8.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Development of the Korean Healthy Eating Index for adults, based on the Korea National Health and Nutrition Examination Survey
- Association between diet quality and type of meal companion: the 2013–2015 Korea National Health and Nutrition Examination Survey (KNHANES)
- Status of Korean Healthy Eating Index and Associated Factors in Elderly with a Focus on Health Habits, Mental Health, and Nutritional Status: Data from the 2016∼2018 Korea National Health and Nutrition Examination Survey
- Association between the Korean Healthy Eating Index and Serum Vitamin D Level in Korean Adults: 2013–2015 Korea National Health and Nutrition Examination Survey
- Benefits of adherence to the Korea Healthy Eating Index on the risk factors and incidence of the metabolic syndrome: analysis of the 7th (2016–2018) Korea National Health and Nutrition Examination Survey