Yeungnam Univ J Med.
2021 Jul;38(3):240-244. 10.12701/yujm.2020.00507.
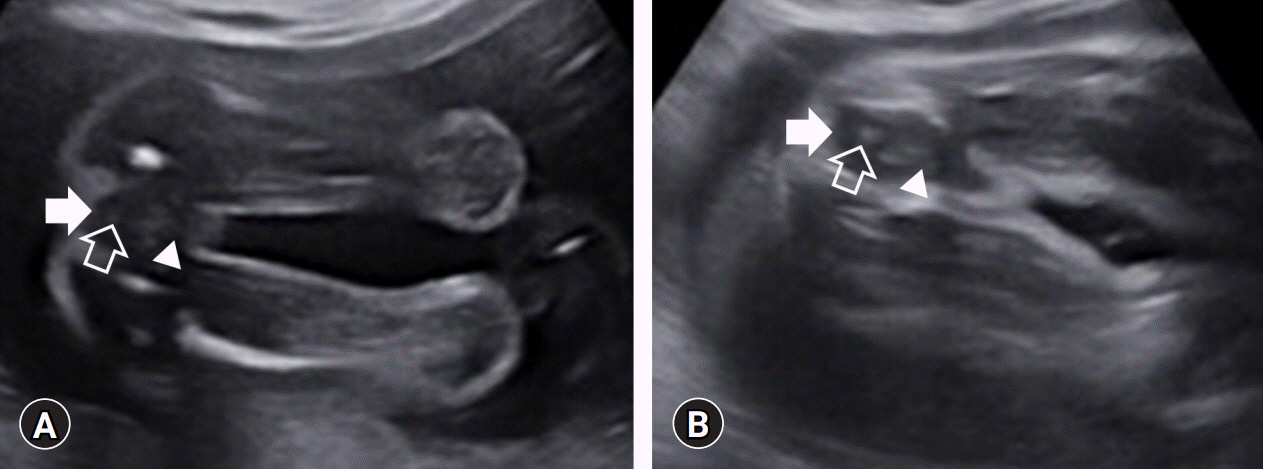
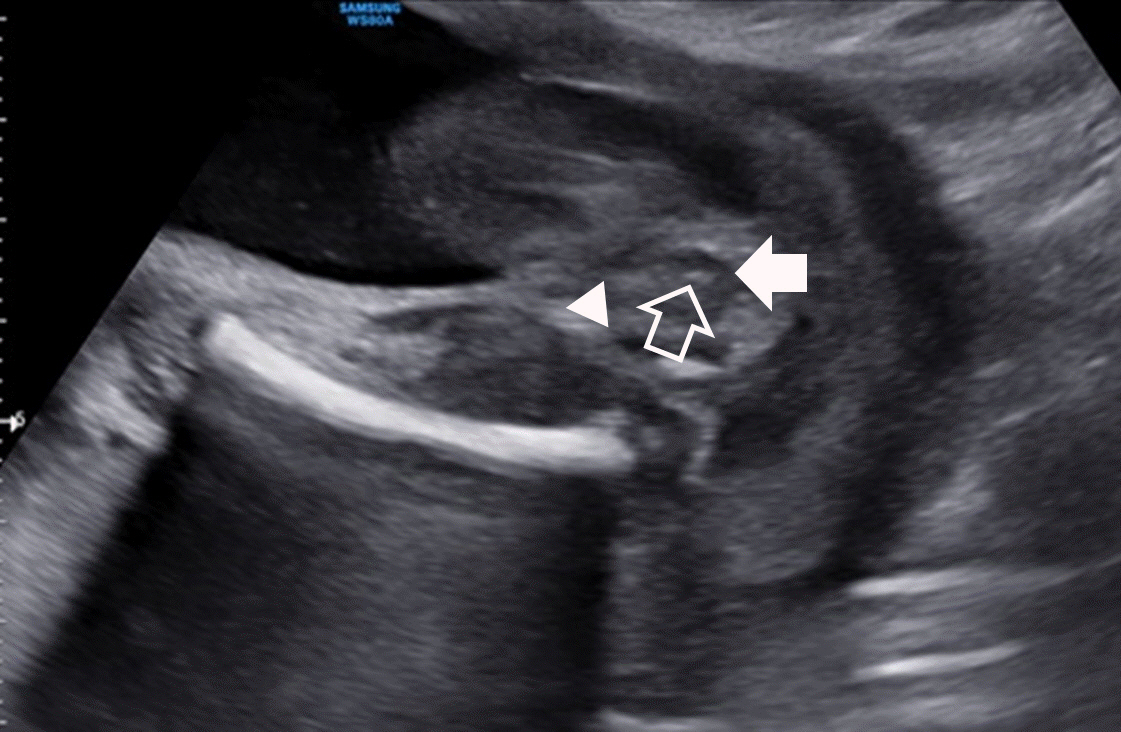
The diagnosis of an imperforate anus in female fetuses
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Kyungpook National University Hospital, Daegu, Korea
- 2Department of Obstetrics and Gynecology, Kyungpook National University Chilgok Hospital, Daegu, Korea
- 3Department of Obstetrics and Gynecology, School of Medicine, Kyungpook National University, Daegu, Korea
- 4Department of Pediatrics, Kyungpook National University Hospital, School of Medicine, Kyungpook National University, Daegu, Korea
- KMID: 2518667
- DOI: http://doi.org/10.12701/yujm.2020.00507
Abstract
- Imperforate anus is an anomaly caused by a defect in the development of the hindgut during early pregnancy. It is a relatively common congenital malformation and is more common in males. Although there are cases of a solitary imperforate anus, the condition is more commonly found as a part of a wider spectrum of other congenital anomalies. Although urgent reconstructive anorectal surgery is not necessary, immediate evaluation is important and urgent decompressive surgery may be required. Moreover, as there are often other anomalies that can affect management, prenatal diagnosis can help in optimizing perinatal care and prepare parents through prenatal counseling. In the past, imperforate anus was diagnosed by prenatal ultrasonography based on indirect signs such as bowel dilatation or intraluminal calcified meconium. Currently, it is diagnosed by directly checking the perineum with prenatal ultrasonography. Despite advances in ultrasound technology, accurate prenatal diagnosis is impossible in most cases and imperforate anus is detected after birth. Here, we present two cases of imperforate anus in female fetuses that were not diagnosed prenatally.
Figure
Reference
-
References
1. Cuschieri A; EUROCAT Working Group. Anorectal anomalies associated with or as part of other anomalies. Am J Med Genet. 2002; 110:122–30.
Article2. Brantberg A, Blaas HG, Haugen SE, Isaksen CV, Eik-Nes SH. Imperforate anus: a relatively common anomaly rarely diagnosed prenatally. Ultrasound Obstet Gynecol. 2006; 28:904–10.
Article3. Cho S, Moore SP, Fangman T. One hundred three consecutive patients with anorectal malformations and their associated anomalies. Arch Pediatr Adolesc Med. 2001; 155:587–91.
Article4. Stoll C, Alembik Y, Dott B, Roth MP. Associated malformations in patients with anorectal anomalies. Eur J Med Genet. 2007; 50:281–90.
Article5. Lee MY, Won HS, Shim JY, Lee PR, Kim A, Lee BS, et al. Sonographic determination of type in a fetal imperforate anus. J Ultrasound Med. 2016; 35:1285–91.
Article6. Black CT, Sherman JO. The association of low imperforate anus and Down’s syndrome. J Pediatr Surg. 1989; 24:92–4.
Article7. Torres R, Levitt MA, Tovilla JM, Rodriguez G, Peña A. Anorectal malformations and Down’s syndrome. J Pediatr Surg. 1998; 33:194–7.
Article8. Bean WJ, Calonje MA, Aprill CN, Geshner J. Anal atresia: a prenatal ultrasound diagnosis. J Clin Ultrasound. 1978; 6:111–2.
Article9. Taipale P, Rovamo L, Hiilesmaa V. First-trimester diagnosis of imperforate anus. Ultrasound Obstet Gynecol. 2005; 25:187–8.
Article10. Harris RD, Nyberg DA, Mack LA, Weinberger E. Anorectal atresia: prenatal sonographic diagnosis. AJR Am J Roentgenol. 1987; 149:395–400.
Article11. Hearn-Stebbins B, Sherer DM, Abramowicz JS, Hess HM, Woods JR Jr. Prenatal sonographic features associated with an imperforate anus and rectourethral fistula. J Clin Ultrasound. 1991; 19:508–12.
Article12. Bronshtein M, Zimmer EZ. Early sonographic detection of fetal intestinal obstruction and possible diagnostic pitfalls. Prenat Diagn. 1996; 16:203–6.
Article13. Grant T, Newman M, Gould R, Schey W, Perry R, Brandt T. Intraluminal colonic calcifications associated with anorectal atresia: prenatal sonographic detection. J Ultrasound Med. 1990; 9:411–3.
Article14. Mandell J, Lillehei CW, Greene M, Benacerraf BR. The prenatal diagnosis of imperforate anus with rectourinary fistula: dilated fetal colon with enterolithiasis. J Pediatr Surg. 1992; 27:82–4.
Article15. Shalev E, Weiner E, Zuckerman H. Prenatal ultrasound diagnosis of intestinal calcifications with imperforate anus. Acta Obstet Gynecol Scand. 1983; 62:95–6.
Article16. Lubusky M, Prochazka M, Dhaifalah I, Horak D, Geierova M, Santavy J. Fetal enterolithiasis: prenatal sonographic and MRI diagnosis in two cases of urorectal septum malformation (URSM) sequence. Prenat Diagn. 2006; 26:345–9.
Article17. Shimotake T, Higuchi K, Tsuda T, Aoi S, Iwai N. Infrared spectrophotometry of intraluminal meconium calculi in a neonate with imperforate anus and rectourethral fistula. J Pediatr Surg. 2006; 41:1173–6.
Article18. Guzman ER, Ranzini A, Day-Salvatore D, Weinberger B, Spigland N, Vintzileos A. The prenatal ultrasonographic visualization of imperforate anus in monoamniotic twins. J Ultrasound Med. 1995; 14:547–51.
Article19. Ochoa JH, Chiesa M, Vildoza RP, Wong AE, Sepulveda W. Evaluation of the perianal muscular complex in the prenatal diagnosis of anorectal atresia in a high-risk population. Ultrasound Obstet Gynecol. 2012; 39:521–7.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Two Experiences of Operation about Urogenital Anomalies Associated with Congenital Imperforate Anus
- Urogenital anomalies associated with imperforative anus
- A Case of Congenital Colonic Atresia Associated with Imperforate Anus
- A case of successful vaginal delivery in a patient with a repair of an imperforate anus
- Ultrasound measurement of pouch to perineum distance as a guide in determination of high or low imperforate anus