Cancer Res Treat.
2021 Jul;53(3):784-794. 10.4143/crt.2020.1064.
Double Tract Reconstruction Reduces Reflux Esophagitis and Improves Quality of Life after Radical Proximal Gastrectomy for Patients with Upper Gastric or Esophagogastric Adenocarcinoma
- Affiliations
-
- 1Key Laboratory of Carcinogenesis and Translational Research (Ministry of Education/Beijing), Gastrointestinal Cancer Center, Peking University Cancer Hospital and Institute, Beijing, China
- KMID: 2518402
- DOI: http://doi.org/10.4143/crt.2020.1064
Abstract
- Purpose
The aim of the present study was to compare the difference between double tract reconstruction and esophagogastrostomy.
Materials and Methods
Patients who underwent radical proximal gastrectomy with esophagogastrostomy or double tract reconstruction were included in this study.
Results
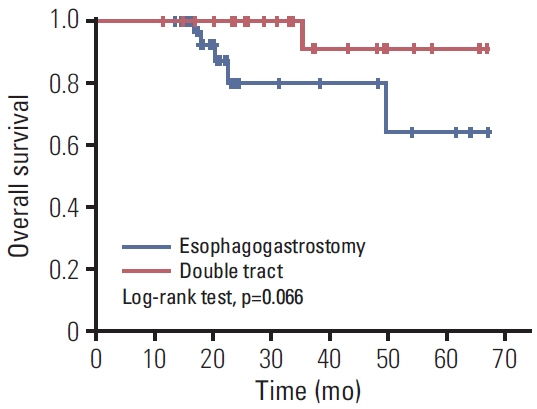
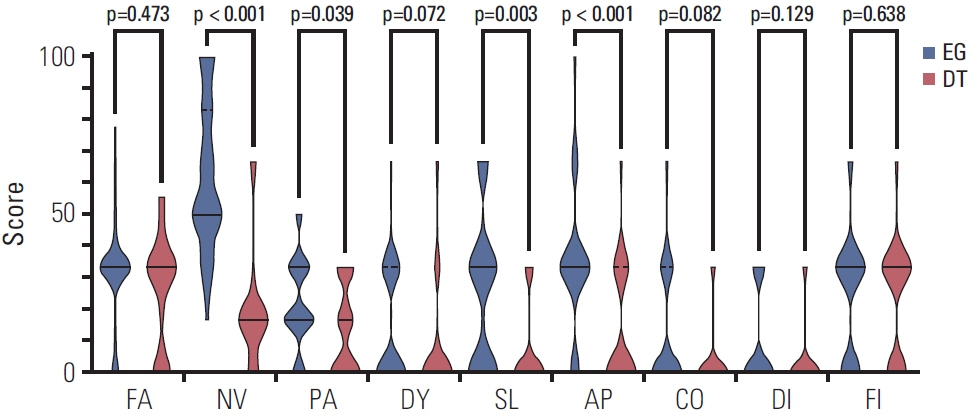
Sixty-four patients were included in this study and divided into two groups according to reconstruction method. The two groups were well balanced in perioperative safety and 3-year overall survival (OS). The rates of postoperative reflux esophagitis in the double tract reconstruction group and esophagogastrostomy group were 8.0% and 30.8%, respectively (p=0.032). Patients in the double tract reconstruction group had a better global health status (p < 0.001) and emotional functioning (p < 0.001), and complained less about nausea and vomiting (p < 0.001), pain (p=0.039), insomnia (p=0.003), and appetite loss (p < 0.001) based on the European Organization for Research and Treatment of Cancer (EORTC) QLQ-C30 questionnaire. Regarding the EORTC QLQ-STO22 questionnaire, patients in the double tract reconstruction group complained less about dysphagia (p=0.030), pain (p=0.008), reflux (p < 0.001), eating (p < 0.001), anxiety (p < 0.001), dry mouth (p=0.007), and taste (p=0.001). The multiple linear regression analysis showed that reconstruction method, postoperative complications, reflux esophagitis, and operation duration had a linear relationship with the global health status score.
Conclusion
Double tract reconstruction could better prevent reflux esophagitis and improve quality of life without scarifying perioperative safety or 3-year OS.
Figure
Reference
-
References
1. Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018; 68:394–424.
Article2. Wang A, Li Z, Wang Q, Bai Y, Ji X, Fu T, et al. Diagnostic value of negative enrichment and immune fluorescence in situ hybridization for intraperitoneal free cancer cells of gastric cancer. Chin J Cancer Res. 2019; 31:945–54.
Article3. Sun W, Deng J, Zhang N, Liu H, Liu J, Gu P, et al. Prognostic impact of D2-plus lymphadenectomy and optimal extent of lymphadenectomy in advanced gastric antral carcinoma: Propensity score matching analysis. Chin J Cancer Res. 2020; 32:51–61.
Article4. Haruta S, Shinohara H, Hosogi H, Ohkura Y, Kobayashi N, Mizuno A, et al. Proximal gastrectomy with exclusion of no. 3b lesser curvature lymph node dissection could be indicated for patients with advanced upper-third gastric cancer. Gastric Cancer. 2017; 20:528–35.
Article5. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2018 (5th edition). Gastric Cancer. 2021; 24:1–21.6. Hiki N, Nunobe S, Kubota T, Jiang X. Function-preserving gastrectomy for early gastric cancer. Ann Surg Oncol. 2013; 20:2683–92.
Article7. Takayama T, Matsumoto S, Wakatsuki K, Tanaka T, Migita K, Ito M, et al. Novel laparoscopic procedure for treating proximal early gastric cancer: laparoscopy-assisted pylorus-preserving nearly total gastrectomy. Surg Today. 2014; 44:2332–8.8. Yoo CH, Sohn BH, Han WK, Pae WK. Long-term results of proximal and total gastrectomy for adenocarcinoma of the upper third of the stomach. Cancer Res Treat. 2004; 36:50–5.
Article9. Kumagai K, Shimizu K, Yokoyama N, Aida S, Arima S, Aikou T, et al. Questionnaire survey regarding the current status and controversial issues concerning reconstruction after gastrectomy in Japan. Surg Today. 2012; 42:411–8.
Article10. Ichikawa D, Ueshima Y, Shirono K, Kan K, Shioaki Y, Lee CJ, et al. Esophagogastrostomy reconstruction after limited proximal gastrectomy. Hepatogastroenterology. 2001; 48:1797–801.11. Nakamura M, Nakamori M, Ojima T, Katsuda M, Iida T, Hayata K, et al. Reconstruction after proximal gastrectomy for early gastric cancer in the upper third of the stomach: an analysis of our 13-year experience. Surgery. 2014; 156:57–63.
Article12. Wang S, Lin S, Wang H, Yang J, Yu P, Zhao Q, et al. Reconstruction methods after radical proximal gastrectomy: a systematic review. Medicine (Baltimore). 2018; 97:e0121.13. Ahn SH, Jung DH, Son SY, Lee CM, Park DJ, Kim HH. Laparoscopic double-tract proximal gastrectomy for proximal early gastric cancer. Gastric Cancer. 2014; 17:562–70.
Article14. Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma: 3rd English edition. Gastric Cancer. 2011; 14:101–12.15. Ji X, Bu ZD, Yan Y, Li ZY, Wu AW, Zhang LH, et al. The 8th edition of the American Joint Committee on Cancer tumornode-metastasis staging system for gastric cancer is superior to the 7th edition: results from a Chinese mono-institutional study of 1663 patients. Gastric Cancer. 2018; 21:643–52.
Article16. Japanese Gastric Cancer Association. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017; 20:1–19.17. Li Z, Bai B, Ji G, Li J, Zhao Q. Relationship between ClavienDindo classification and long-term survival outcomes after curative resection for gastric cancer: a propensity scorematched analysis. Int J Surg. 2018; 60:67–73.
Article18. Sugiura T, Iwakiri K, Kotoyori M, Kobayashi M. Relationship between severity of reflux esophagitis according to the Los Angeles classification and esophageal motility. J Gastroenterol. 2001; 36:226–30.
Article19. Jung DH, Lee Y, Kim DW, Park YS, Ahn SH, Park DJ, et al. Laparoscopic proximal gastrectomy with double tract reconstruction is superior to laparoscopic total gastrectomy for proximal early gastric cancer. Surg Endosc. 2017; 31:3961–9.
Article20. Wang L, Xia Y, Jiang T, Li F, Wang W, Zhang D, et al. Shortterm surgical outcomes of laparoscopic proximal gastrectomy with double-tract reconstruction versus laparoscopic total gastrectomy for adenocarcinoma of esophagogastric junction: a matched-cohort study. J Surg Res. 2020; 246:292–9.
Article21. Nakamura M, Yamaue H. Reconstruction after proximal gastrectomy for gastric cancer in the upper third of the stomach: a review of the literature published from 2000 to 2014. Surg Today. 2016; 46:517–27.
Article22. Fayers P, Aaronson N, Bjordal K, Groenvold M, Curran D, Bottomley A. The EORTC QLQ-C30 Scoring Manual. 3rd ed. Brussels: European Organisation for Research and Treatment of Cancer;2001.23. Hongo M, Kinoshita Y, Miwa H, Ashida K. The demographic characteristics and health-related quality of life in a large cohort of reflux esophagitis patients in Japan with reference to the effect of lansoprazole: the REQUEST study. J Gastroenterol. 2008; 43:920–7.
Article24. Javadi S, Shafikhani AA. Anxiety and depression in patients with gastroesophageal reflux disorder. Electron Physician. 2017; 9:5107–12.
Article25. Yoshikawa H, Furuta K, Ueno M, Egawa M, Yoshino A, Kondo S, et al. Oral symptoms including dental erosion in gastroesophageal reflux disease are associated with decreased salivary flow volume and swallowing function. J Gastroenterol. 2012; 47:412–20.
Article26. Shibata T, Nakamura M, Omori T, Tahara T, Ichikawa Y, Okubo M, et al. Association between individual response to food taste and gastroesophageal symptoms. J Dig Dis. 2015; 16:337–41.
Article27. Kauppila JH, Ringborg C, Johar A, Lagergren J, Lagergren P. Health-related quality of life after gastrectomy, esophagectomy, and combined esophagogastrectomy for gastroesophageal junction adenocarcinoma. Gastric Cancer. 2018; 21:533–41.
Article28. Kim SM, Cho J, Kang D, Oh SJ, Kim AR, Sohn TS, et al. A randomized controlled trial of vagus nerve-preserving distal gastrectomy versus conventional distal gastrectomy for postoperative quality of life in early stage gastric cancer patients. Ann Surg. 2016; 263:1079–84.
Article29. Inokuchi M, Sugita H, Otsuki S, Sato Y, Nakagawa M, Kojima K. Long-term effectiveness of preserved celiac branch of vagal nerve after Roux-en-Y reconstruction in laparoscopy-assisted distal gastrectomy. Dig Surg. 2014; 31:341–6.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Proximal Gastrectomy for Upper-third Early Gastric Cancer
- Proximal Gastrectomy with Double Tract Reconstruction Using the Remnant Antrum in Early Upper Gastric Cancer
- Laparoscopic Proximal Gastrectomy as a Surgical Treatment for Upper Third Early Gastric Cancer
- Updated Review of Proximal Gastrectomy for Gastric Cancer or Cancer of the Gastroesophageal Junction
- Single-Port Laparoscopic Proximal Gastrectomy with Double Tract Reconstruction for Early Gastric Cancer: Report of a Case