J Korean Med Sci.
2021 Jul;36(26):e178. 10.3346/jkms.2021.36.e178.
Clinical Outcomes of Clipping and Coiling in Elderly Patients with Unruptured Cerebral Aneurysms: a National Cohort Study in Korea
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University Bundang Hospital, Seongnam, Korea
- 2Department of Neurosurgery, Seoul National University College of Medicine, Seoul, Korea
- 3Department of Neurosurgery, Chungnam University Sejong Hospital, Sejong, Korea
- KMID: 2518156
- DOI: http://doi.org/10.3346/jkms.2021.36.e178
Abstract
- Background
We aimed to analyze outcomes of clipping and coiling in treating unruptured intracranial aneurysms (UIAs) in elderly patients and to identify the age at which perioperative risk increases based on national cohort data in South Korea.
Methods
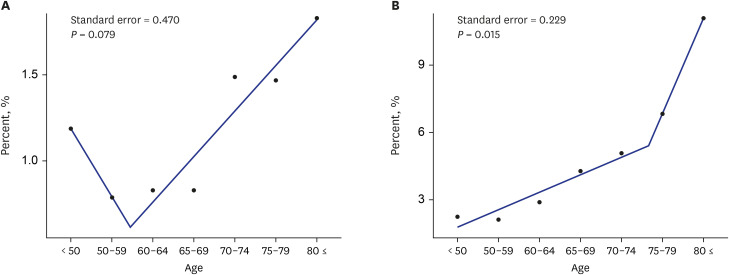
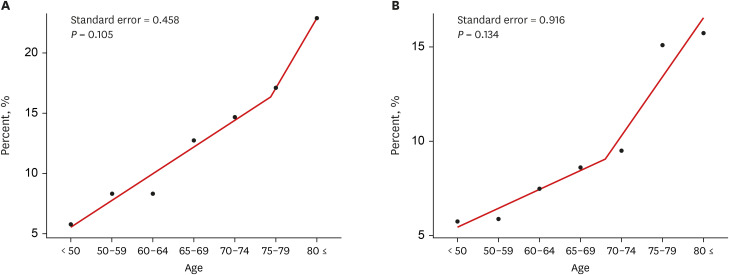
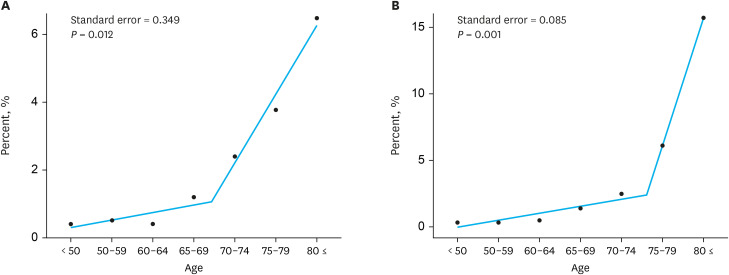
The incidence of perioperative intracranial hemorrhage (ICRH), perioperative cerebral infarction (CI), mortality, and moderate to severe disability data of the patients who underwent coiling or clipping for UIAs were retrieved. Estimated breakpoint (EBP) was calculated to identify the age at which the risk of treatment increases.
Results
A total of 38,207 patients were treated for UIAs. Among these, 22,093 (57.8%) patients underwent coiling and 16,114 (42.2%) patients underwent clipping. The incidence of ICRH, requiring a secondary operation, within 3 months in patients ≥ 65 years that underwent coiling and clipping was 1.13% and 4.81%, respectively, and that of both groups assessed were significantly higher in patients ≥ 75 years (coiling, P = 0.013, relative risk (RR) 1.81; clipping, P = 0.015) than younger patients. The incidence of CI within 3 months in patients aged ≥ 65 was 13.90% and 9.19% in the coiling and clipping groups, respectively. The incidence of CI after coiling in patients aged ≥ 75 years (P < 0.001, RR 1.96) and after clipping in patients aged ≥ 70 years (P < 0.001, RR 1.76) was significantly higher than that in younger patients. The mortality rates within 1 year in patients with perioperative ICRH or CI were 2.41% and 3.39% for coiling and clipping groups, respectively, in patients ≥ 65. These rates increased significantly at age 70 in the coiling group and at age 75 for the clipping group (P = 0.012 and P < 0.001, respectively).
Conclusion
The risk of treatment increases with age, and this risk increases dramatically in patients aged ≥ 70 years. Therefore, the treatment decisions in patients aged ≥ 70 years should be made with utmost care.
Figure
Cited by 2 articles
-
Clinical Outcomes of Coil Embolization for Unruptured Intracranial Aneurysms Categorized by Region and Hospital Size : A Nationwide Cohort Study in Korea
Bong-Gyu Ryu, Si Un Lee, Hwan Seok Shim, Jeong-Mee Park, Yong Jae Lee, Young-Deok Kim, Tackeun Kim, Seung Pil Ban, Hyoung Soo Byoun, Jae Seung Bang, O-ki Kwon, Chang Wan Oh
J Korean Neurosurg Soc. 2023;66(6):690-702. doi: 10.3340/jkns.2023.0033.A Case of Severe Delayed Vasospasm after Clipping Surgery for an Unruptured Intracranial Aneurysm
Joong-Goo Kim, Chul-Hoo Kang, Jae Jon Sheen, Yunsun Song, Jong-Kook Rhim
Neurointervention. 2024;19(2):123-128. doi: 10.5469/neuroint.2024.00150.
Reference
-
1. Thompson BG, Brown RD Jr, Amin-Hanjani S, Broderick JP, Cockroft KM, Connolly ES Jr, et al. Guidelines for the management of patients with unruptured intracranial aneurysms: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015; 46(8):2368–2400. PMID: 26089327.2. Juvela S, Poussa K, Lehto H, Porras M. Natural history of unruptured intracranial aneurysms: a long-term follow-up study. Stroke. 2013; 44(9):2414–2421. PMID: 23868274.
Article3. Wiebers DO, Whisnant JP, Huston J 3rd, Meissner I, Brown RD Jr, Piepgras DG, et al. Unruptured intracranial aneurysms: natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003; 362(9378):103–110. PMID: 12867109.
Article4. United Nations, Department of Economic and Social Affairs, Population Division. World Population Prospects 2019: Highlights. New York, NY, USA: United Nations, Department of Economic and Social Affairs, Population Division;2019.5. Lee SU, Kim T, Kwon OK, Bang JS, Ban SP, Byoun HS, et al. Trends in the incidence and treatment of cerebrovascular diseases in Korea: Part II. Cerebral infarction, cerebral arterial stenosis, and moyamoya disease. J Korean Neurosurg Soc. 2020; 63(1):69–79. PMID: 31064040.6. Lee SU, Kim T, Kwon OK, Bang JS, Ban SP, Byoun HS, et al. Trends in the incidence and treatment of cerebrovascular diseases in Korea: Part I. Intracranial aneurysm, intracerebral hemorrhage, and arteriovenous malformation. J Korean Neurosurg Soc. 2020; 63(1):56–68. PMID: 31064041.7. Vernooij MW, Ikram MA, Tanghe HL, Vincent AJ, Hofman A, Krestin GP, et al. Incidental findings on brain MRI in the general population. N Engl J Med. 2007; 357(18):1821–1828. PMID: 17978290.
Article8. Mahaney KB, Brown RD Jr, Meissner I, Piepgras DG, Huston J 3rd, Zhang J, et al. Age-related differences in unruptured intracranial aneurysms: 1-year outcomes. J Neurosurg. 2014; 121(5):1024–1038. PMID: 25170670.
Article9. Jalbert JJ, Isaacs AJ, Kamel H, Sedrakyan A. Clipping and coiling of unruptured intracranial aneurysms among medicare beneficiaries, 2000 to 2010. Stroke. 2015; 46(9):2452–2457. PMID: 26251248.
Article10. Bekelis K, Gottlieb DJ, Su Y, O'Malley AJ, Labropoulos N, Goodney P, et al. Comparison of clipping and coiling in elderly patients with unruptured cerebral aneurysms. J Neurosurg. 2017; 126(3):811–818. PMID: 27203150.
Article11. Brinjikji W, Rabinstein AA, Lanzino G, Kallmes DF, Cloft HJ. Effect of age on outcomes of treatment of unruptured cerebral aneurysms: a study of the National Inpatient Sample 2001–2008. Stroke. 2011; 42(5):1320–1324. PMID: 21441142.12. Kwinta BM, Kliś KM, Krzyżewski RM, Wilk A, Dragan M, Grzywna E, et al. Elective management of unruptured intracranial aneurysms in elderly patients in a high-volume center. World Neurosurg. 2019; 126:e1343–51. PMID: 30898743.
Article13. Sturiale CL, Brinjikji W, Murad MH, Lanzino G. Endovascular treatment of intracranial aneurysms in elderly patients: a systematic review and meta-analysis. Stroke. 2013; 44(7):1897–1902. PMID: 23686977.14. O'Neill AH, Chandra RV, Slater LA, Chong W, Xenos C, Danks AR, et al. Influence of comorbidities on treatment of unruptured intracranial aneurysms in the elderly. J Clin Neurosci. 2019; 62:38–45. PMID: 30655235.15. Jung YJ, Ahn JS, Park ES, Kwon DH, Kwun BD, Kim CJ. Surgical results of unruptured intracranial aneurysms in the elderly: single center experience in the past ten years. J Korean Neurosurg Soc. 2011; 49(6):329–333. PMID: 21887389.16. Oishi H, Yamamoto M, Nonaka S, Shimizu T, Yoshida K, Mitsuhashi T, et al. Treatment results of endosaccular coil embolization of asymptomatic unruptured intracranial aneurysms in elderly patients. J Neurointerv Surg. 2015; 7(9):660–665. PMID: 25034903.
Article17. Ikawa F, Michihata N, Akiyama Y, Iihara K, Matano F, Morita A, et al. Treatment risk for elderly patients with unruptured cerebral aneurysm from a nationwide database in Japan. World Neurosurg. 2019; 132:e89–98. PMID: 31518740.
Article18. Silva NA, Shao B, Sylvester MJ, Eloy JA, Gandhi CD. Unruptured aneurysms in the elderly: perioperative outcomes and cost analysis of endovascular coiling and surgical clipping. Neurosurg Focus. 2018; 44(5):E4.
Article19. Muramatsu N, Akiyama H. Japan: super-aging society preparing for the future. Gerontologist. 2011; 51(4):425–432. PMID: 21804114.
Article20. Han SB, Hyon JY, Woo SJ, Lee JJ, Kim TH, Kim KW. Prevalence of dry eye disease in an elderly Korean population. Arch Ophthalmol. 2011; 129(5):633–638. PMID: 21555618.
Article21. Park JH, Lee JJ, Lee SB, Huh Y, Choi EA, Youn JC, et al. Prevalence of major depressive disorder and minor depressive disorder in an elderly Korean population: results from the Korean Longitudinal Study on Health and Aging (KLoSHA). J Affect Disord. 2010; 125(1-3):234–240. PMID: 20188423.
Article22. Orimo H, Ito H, Suzuki T, Araki A, Hosoi T, Sawabe M. Reviewing the definition of elderly. Nippon Ronen Igakkai Zasshi. 2006; 43(1):27–34. PMID: 16521795.
Article23. Paik JE, Choi HK. Successful aging according to Korean elderly: The definition, types, and predicting variables. J Korean Home Manage Assoc. 2005; 23(3):1–16.24. Khosla A, Brinjikji W, Cloft H, Lanzino G, Kallmes DF. Age-related complications following endovascular treatment of unruptured intracranial aneurysms. AJNR Am J Neuroradiol. 2012; 33(5):953–957. PMID: 22241386.
Article25. Brinjikji W, Rabinstein AA, Nasr DM, Lanzino G, Kallmes DF, Cloft HJ. Better outcomes with treatment by coiling relative to clipping of unruptured intracranial aneurysms in the United States, 2001–2008. AJNR Am J Neuroradiol. 2011; 32(6):1071–1075. PMID: 21511860.
Article26. Barker FG 2nd, Amin-Hanjani S, Butler WE, Ogilvy CS, Carter BS. In-hospital mortality and morbidity after surgical treatment of unruptured intracranial aneurysms in the United States, 1996–2000: the effect of hospital and surgeon volume. Neurosurgery. 2003; 52(5):995–1007. PMID: 12699540.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Current Update on the Randomized Controlled Trials of Intracranial Aneurysms
- Treatment outcome after coiling or clipping for elderly patients with unruptured intracranial aneurysms
- Comprehension of Two Modalities: Endovascular Coiling and Microsurgical Clipping in Treatment of Intracranial Aneurysms
- Cost Analysis for the Management of Cerebral Aneurysms: Comparison between Clipping and Coiling
- Benefits of Surgical Treatment for Unruptured Intracranial Aneurysms in Elderly Patients